Abstract
BACKGROUND—Mitochondrial DNA (mtDNA) defects are an important cause of disease. Although gastrointestinal symptoms are common in these patients, their pathogenesis remains uncertain. AIM—To investigate the role of the mtDNA defect in the production of gastrointestinal dysfunction. PATIENT—A 20 year old woman who presented at 15 years of age with recurrent vomiting and pseudo-obstruction, who did not respond to conservative management and ultimately had subtotal gastrectomy and Roux-en-y reconstruction. She subsequently presented with status epilepticus and was found to have a mitochondrial respiratory chain disorder due to a pathogenic mtDNA point mutation (A3243G). METHODS—Resected bowel was studied using light and electron microscopy and mtDNA analysed from both mucosal and muscular layers using polymerase chain reaction generated RFLP analysis. RESULTS— Histological and electron microscopic studies revealed no morphological abnormalities in the resected stomach, and molecular genetic analysis failed to identify the genetic defect in either the mucosal or muscle layers. CONCLUSION—This study suggests that in some individuals with gastrointestinal symptoms associated with established mitochondrial DNA disease, the primary pathology of the mitochondrial enteropathy lies outside the gastrointestinal tract. Keywords: mitochondrial encephalomyopathy; cyclical vomiting; pseudo-obstruction
Full Text
The Full Text of this article is available as a PDF (141.7 KB).
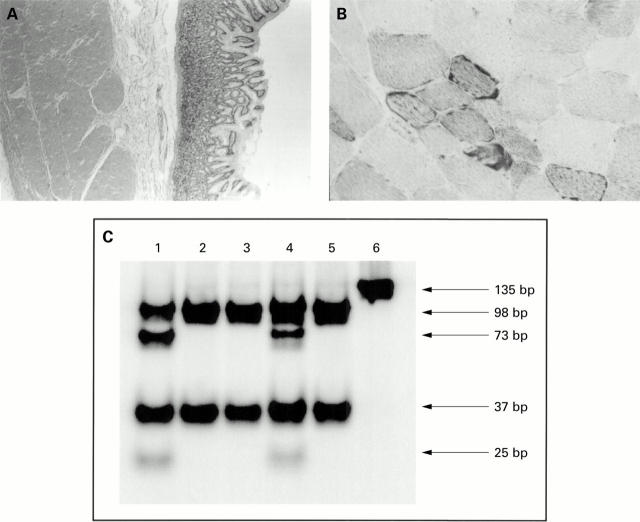
Figure 1 .
(A) Histology of the resected stomach. Cross section of the stomach showing normal histology. (B) Succinate dehydrogenase (SDH) activity in skeletal muscle. Skeletal muscle in cross section. SDH is a mitochondrial enzyme and this section shows the classical accumulation of mitochondria around the periphery of the fibre (classically called ragged red with Gomori Trichrome staining) which suggests a mitochondrial disorder. (C) Last hot cycle PCR of mtDNA. Autoradiograph of a 12% polyacrylamide gel showing the results of the Hae III digest. The 135 bp radiolabelled PCR uncut product is shown in lane 6. When this is digested it produces two bands (98 bp and 37 bp) in the wild-type (lane 5=normal control). The A3243G MELAS mutation introduces an additional Hae III site in the 98 bp fragment, resulting in 73 bp and 25 bp fragments. Patient tissues are shown in lanes 1-4: lane 1, skeletal muscle; lane 2, stomach mucosal layer; lane 3, stomach muscle layer; lane 4, white blood cell. The two extra bands arising from the A3243G mutation are easily seen in her skeletal muscle and blood, but not in either the muscle or mucosal layers of her stomach.