Abstract
BACKGROUND—Abdominal distension is one of the cardinal features of irritable bowel syndrome (IBS) with patients often ranking it as more intrusive than their pain or bowel dysfunction. If this symptom could be quantified accurately and reliably it would provide, for the first time, an objective way of assessing this disorder. Using the principle of inductance plethysmography we have developed a microprocessor based system capable of recording even minimal changes in girth over 24 hours and we describe its validation and establish normal ranges. METHODS—Twenty four hour recordings were made in 20 healthy female volunteers (aged 23-58 years) to assess changes in abdominal girth with respect to time, posture, meals, and sleep. Normal daily activity was encouraged and meals were standardised. The feeling of abdominal distension was also assessed using a visual analogue scale. FINDINGS—Measurement of abdominal girth using abdominal inductance plethysmography (AIP) at a static point in time showed a close relationship with that measured using a tape measure (rho=0.8910, p<0.001). Furthermore, girth was significantly greater both in the sitting and standing postures compared with lying (p<0.01). Measurement over a 24 hour period showed that girth was significantly greater at the end compared with the beginning of the day, and ingestion of a standard meal also increased its value (p<0.05). Sleep was associated with a reduction in girth (p<0.05). CONCLUSIONS—AIP promises to add an objective dimension to the assessment of IBS which could prove invaluable in clinical trials. Furthermore, it should aid research into the pathogenesis of this symptom for which no satisfactory explanation has yet emerged. Keywords: abdominal distension; irritable bowel syndrome
Full Text
The Full Text of this article is available as a PDF (176.0 KB).
Figure 1 .
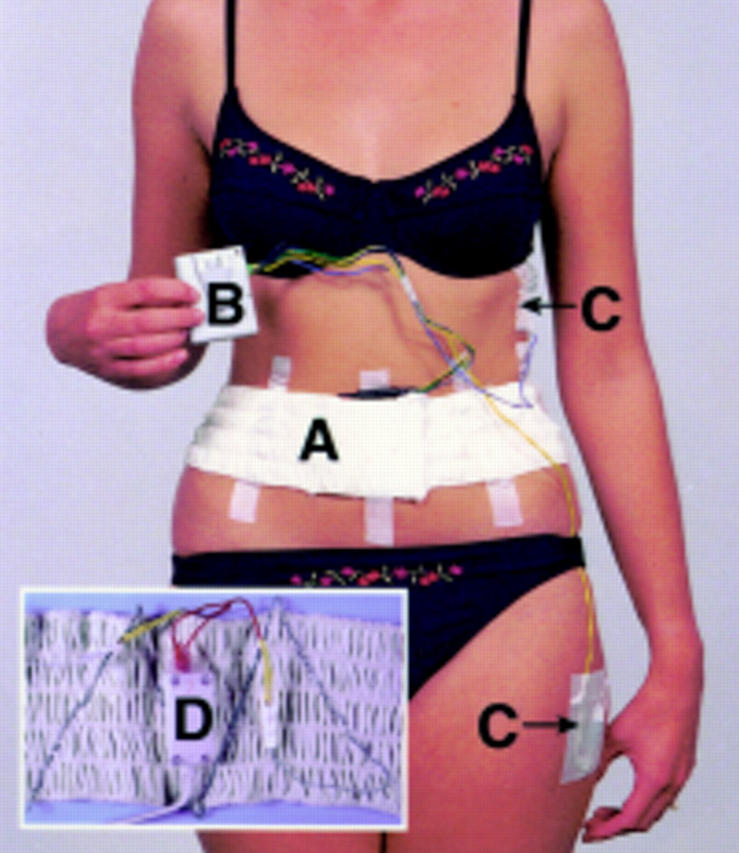
Photograph of a subject wearing the equipment. A, the belt; B, data logger; and C, mercury tilt switches. Insert shows a close up of the belt revealing the wire sewn in a zig zag fashion and connected to an oscillator (D) which is secured under the belt.
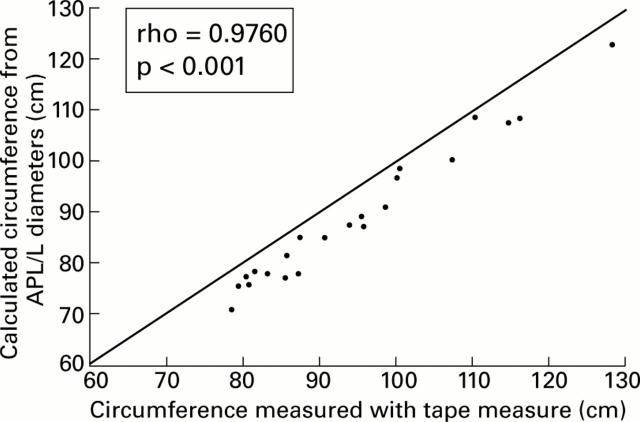
Figure 2 .
Relationship between abdominal circumference calculated from anteroposterior (AP) and lateral (L) diameters and that obtained from the tape measure (line represents line of equality).
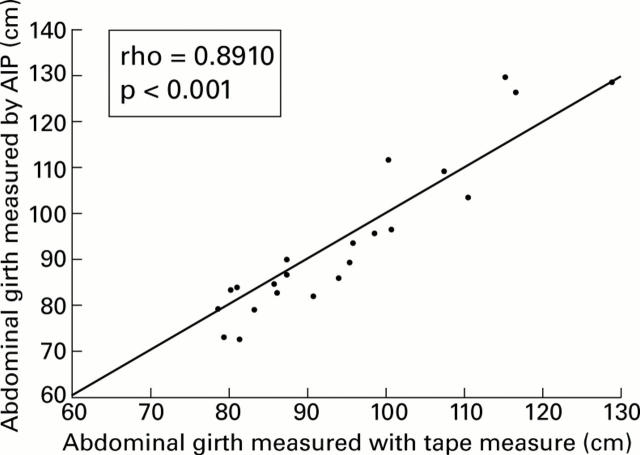
Figure 3 .
Relationship between abdominal girth measured by abdominal inductance plethysmography (AIP) and that obtained with the tape measure (line represents line of equality).
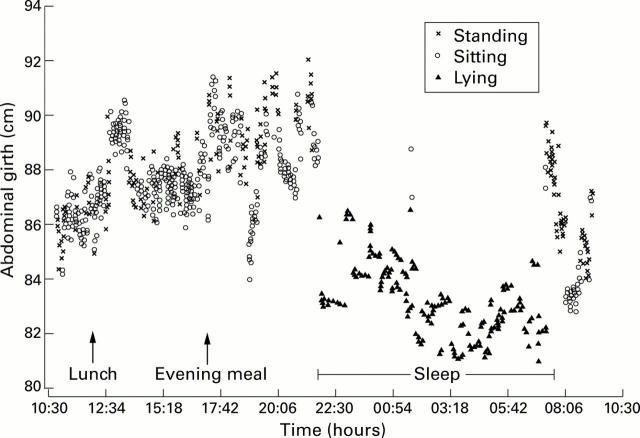
Figure 4 .
Typical recording of abdominal girth over 24 hours in a normal healthy volunteer. Note the gradual increase in girth during the day, increase with meal ingestion, and slow reduction in girth during sleep.
Figure 5 .
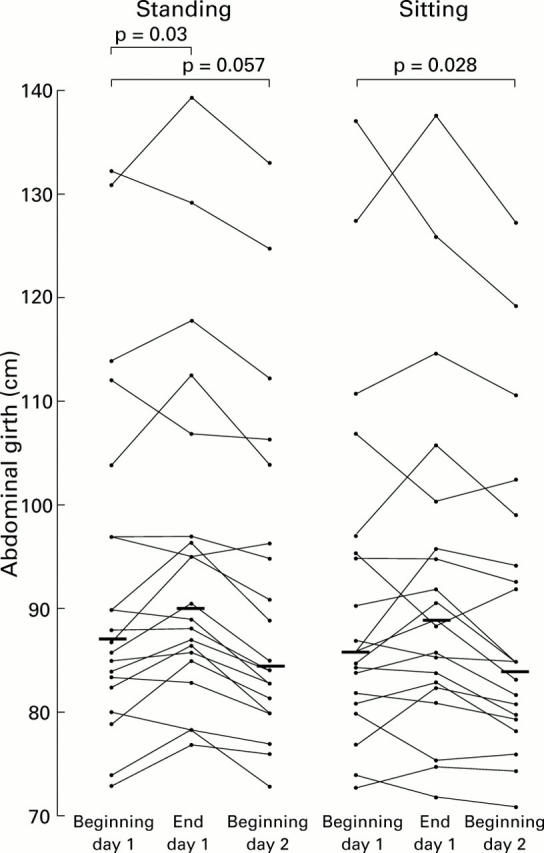
Abdominal girth measured by abdominal inductance plethysmography at the beginning of day 1, at the end of day 1, and at the beginning of day 2 for standing and sitting postures. Bars represent median values.
Figure 6 .
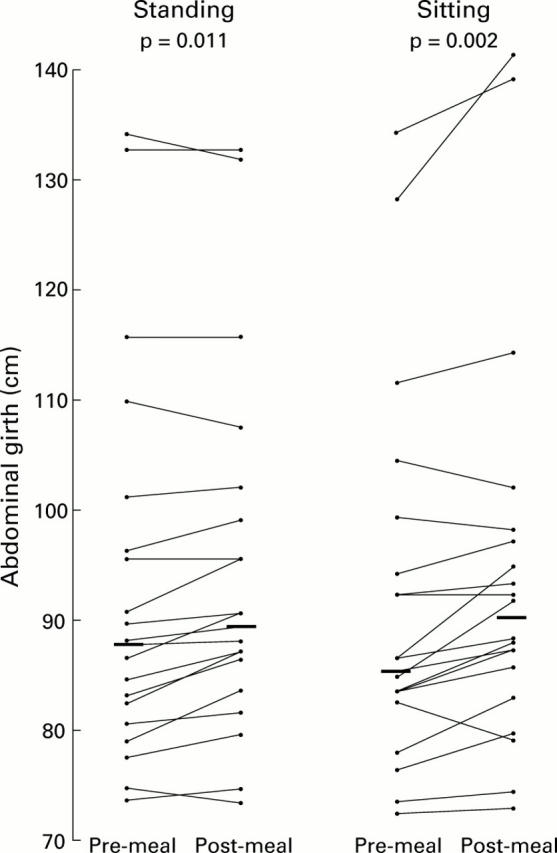
Abdominal girth measured by abdominal inductance plethysmography before and after the standard evening meal for standing and sitting postures. Bars represent median values.
Figure 7 .
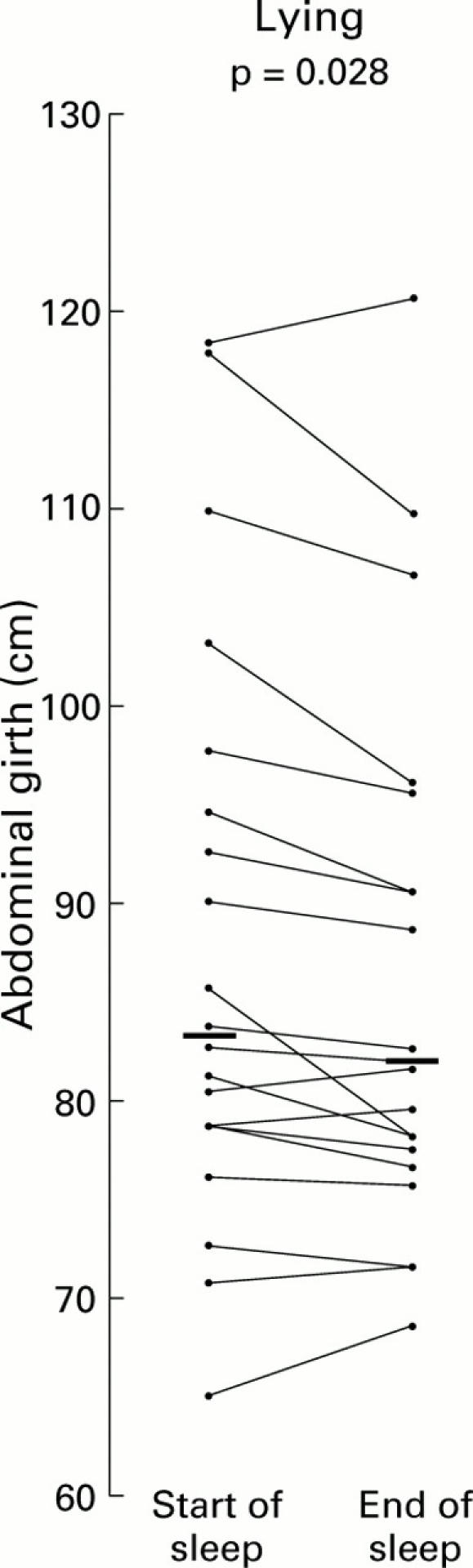
Abdominal girth measured by abdominal inductance plethysmography in the lying posture at the start and end of sleep. Bars represent median values.
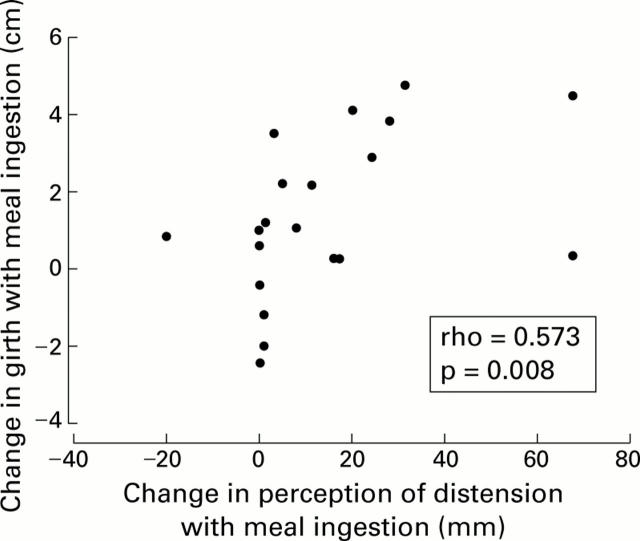
Figure 8 .
Correlation of change in perception of abdominal distension with actual girth measurement following meal ingestion.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Heaton K. W., O'Donnell L. J., Braddon F. E., Mountford R. A., Hughes A. O., Cripps P. J. Symptoms of irritable bowel syndrome in a British urban community: consulters and nonconsulters. Gastroenterology. 1992 Jun;102(6):1962–1967. doi: 10.1016/0016-5085(92)90320-x. [DOI] [PubMed] [Google Scholar]
- Maxton D. G., Martin D. F., Whorwell P. J., Godfrey M. Abdominal distension in female patients with irritable bowel syndrome: exploration of possible mechanisms. Gut. 1991 Jun;32(6):662–664. doi: 10.1136/gut.32.6.662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxton D. G., Morris J. A., Whorwell P. J. Ranking of symptoms by patients with the irritable bowel syndrome. BMJ. 1989 Nov 4;299(6708):1138–1138. doi: 10.1136/bmj.299.6708.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan S. N. A prospective study of unexplained visible abdominal bloating. N Z Med J. 1994 Oct 26;107(988):428–430. [PubMed] [Google Scholar]
- Talley N. J., Zinsmeister A. R., Van Dyke C., Melton L. J., 3rd Epidemiology of colonic symptoms and the irritable bowel syndrome. Gastroenterology. 1991 Oct;101(4):927–934. doi: 10.1016/0016-5085(91)90717-y. [DOI] [PubMed] [Google Scholar]
- Thompson W. G., Heaton K. W. Functional bowel disorders in apparently healthy people. Gastroenterology. 1980 Aug;79(2):283–288. [PubMed] [Google Scholar]
- Watson H. L., Poole D. A., Sackner M. A. Accuracy of respiratory inductive plethysmographic cross-sectional areas. J Appl Physiol (1985) 1988 Jul;65(1):306–308. doi: 10.1152/jappl.1988.65.1.306. [DOI] [PubMed] [Google Scholar]