Abstract
BACKGROUND—Lipids may exacerbate symptoms induced by gut stimuli. AIM—To determine the mechanism whereby fat exerts this effect. SUBJECTS—Twenty four healthy subjects were studied during fasting. METHODS—We measured perception (0-6 scale) in response to jejunal balloon distension and transmucosal electrical nerve stimulation; phasic stimuli (one minute) were randomly applied at five minute intervals during intestinal infusion (2 ml/min) of saline and then Intralipid 2 kcal/min (high fat; n=8 subjects), Intralipid 0.5 kcal/min (low fat; n=8), or saline (n=8). RESULTS—Intestinal lipids increased the perception of jejunal distension regardless of concentration (by 53% with high fat, 49% with low fat, and 17% with saline; p<0.05 for both fat loads). This effect could not be attributed to changes in intestinal compliance as intraballoon pressures remained unchanged during lipid infusion (2% change; NS). Sensitisation induced by lipids seemed to be specifically related to intestinal mechanoreceptors because electrical stimulation, which non-specifically activates gut afferents, was perceived equally during saline and lipid administration (10%, 11%, and 15% change during high fat, low fat, and saline, respectively; NS). CONCLUSION—Physiological amounts of lipids heighten intestinal sensitivity by modulating intestinal mechanoreceptor response. Keywords: intestinal sensitivity; intestinal distension; intestinal electrical nerve stimulation; intestinal afferents; abdominal symptoms
Full Text
The Full Text of this article is available as a PDF (135.1 KB).
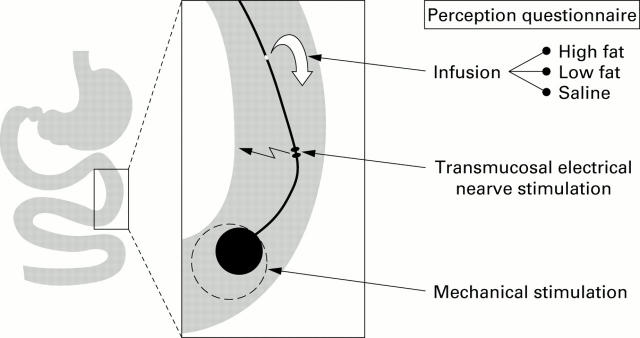
Figure 1 .
Diagrammatic representation of the probe used. The probe incorporated a perfusion port, a bipolar electrode for electrical stimulation, and an inflatable balloon. Electrical stimuli and distensions (one minute duration) were randomly tested (at five minute intervals) during infusion of either saline, low fat, or high fat while measuring intraballoon pressures and perception on a 0-6 scale.
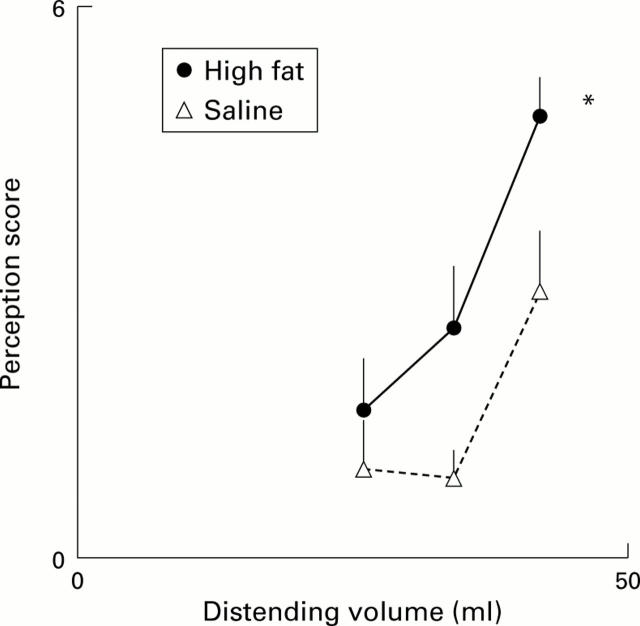
Figure 2 .
Perception of intestinal distension. Intestinal fat infusion significantly increased perception (*p<0.05). Data for the three highest stimuli tested in each subject during both saline and high fat infusion are shown.
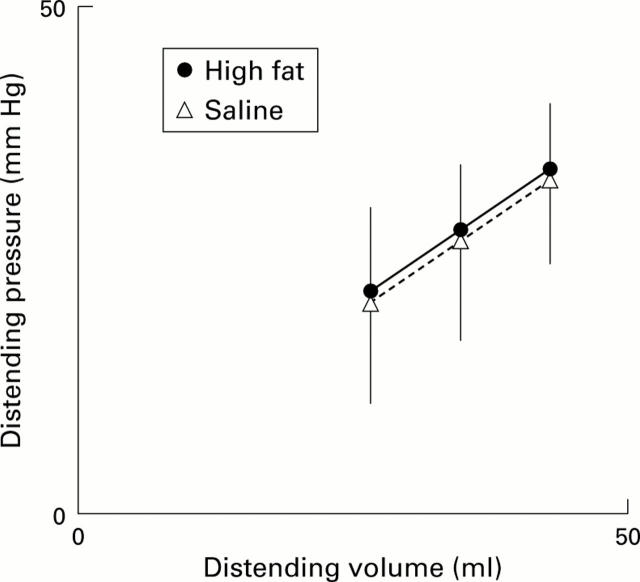
Figure 3 .
Intestinal compliance. Intestinal fat infusion did not induce any change in intestinal compliance that could explain increased perception of distension. Data for the three highest stimuli tested in each subject during both saline and high fat infusions are shown.
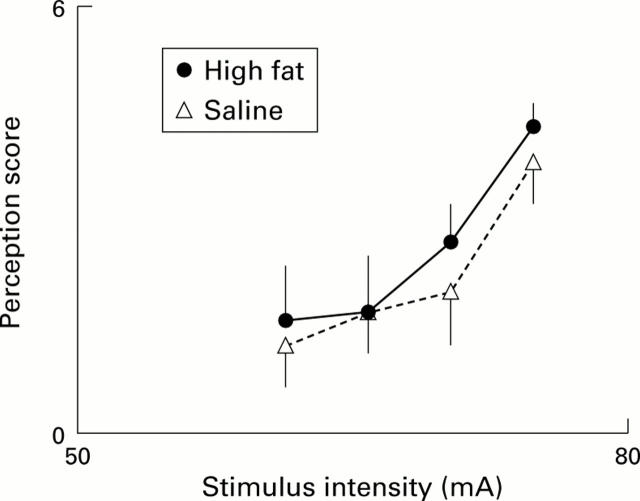
Figure 4 .
Perception of intestinal electrical nerve stimulation. Intestinal infusion had no effect on perception of transmucosal electrical nerve stimulation. Data for the four highest stimuli tested in each subject during both saline and high fat infusions are shown.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Accarino A. M., Azpiroz F., Malagelada J. R. Selective dysfunction of mechanosensitive intestinal afferents in irritable bowel syndrome. Gastroenterology. 1995 Mar;108(3):636–643. doi: 10.1016/0016-5085(95)90434-4. [DOI] [PubMed] [Google Scholar]
- Accarino A. M., Azpiroz F., Malagelada J. R. Selective dysfunction of mechanosensitive intestinal afferents in irritable bowel syndrome. Gastroenterology. 1995 Mar;108(3):636–643. doi: 10.1016/0016-5085(95)90434-4. [DOI] [PubMed] [Google Scholar]
- Accarino A. M., Azpiroz F., Malagelada J. R. Symptomatic responses to stimulation of sensory pathways in the jejunum. Am J Physiol. 1992 Nov;263(5 Pt 1):G673–G677. doi: 10.1152/ajpgi.1992.263.5.G673. [DOI] [PubMed] [Google Scholar]
- Barber W. D., Yuan C. S. Gastric vagal-evoked and greater splanchnic-evoked unitary responses in the hypothalamus. Am J Physiol. 1993 Jun;264(6 Pt 1):G1133–G1141. doi: 10.1152/ajpgi.1993.264.6.G1133. [DOI] [PubMed] [Google Scholar]
- Barbera R., Feinle C., Read N. W. Abnormal sensitivity to duodenal lipid infusion in patients with functional dyspepsia. Eur J Gastroenterol Hepatol. 1995 Nov;7(11):1051–1057. doi: 10.1097/00042737-199511000-00007. [DOI] [PubMed] [Google Scholar]
- Barbera R., Feinle C., Read N. W. Nutrient-specific modulation of gastric mechanosensitivity in patients with functional dyspepsia. Dig Dis Sci. 1995 Aug;40(8):1636–1641. doi: 10.1007/BF02212683. [DOI] [PubMed] [Google Scholar]
- Cook I. J., van Eeden A., Collins S. M. Patients with irritable bowel syndrome have greater pain tolerance than normal subjects. Gastroenterology. 1987 Oct;93(4):727–733. doi: 10.1016/0016-5085(87)90434-3. [DOI] [PubMed] [Google Scholar]
- Distrutti E., Azpiroz F., Soldevilla A., Malagelada J. R. Gastric wall tension determines perception of gastric distention. Gastroenterology. 1999 May;116(5):1035–1042. doi: 10.1016/s0016-5085(99)70006-5. [DOI] [PubMed] [Google Scholar]
- Feinle C., D'Amato M., Read N. W. Cholecystokinin-A receptors modulate gastric sensory and motor responses to gastric distension and duodenal lipid. Gastroenterology. 1996 May;110(5):1379–1385. doi: 10.1053/gast.1996.v110.pm8613041. [DOI] [PubMed] [Google Scholar]
- Feinle C., Grundy D., Read N. W. Effects of duodenal nutrients on sensory and motor responses of the human stomach to distension. Am J Physiol. 1997 Sep;273(3 Pt 1):G721–G726. doi: 10.1152/ajpgi.1997.273.3.G721. [DOI] [PubMed] [Google Scholar]
- IGGO A. Tension receptors in the stomach and the urinary bladder. J Physiol. 1955 Jun 28;128(3):593–607. doi: 10.1113/jphysiol.1955.sp005327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer E. A., Gebhart G. F. Basic and clinical aspects of visceral hyperalgesia. Gastroenterology. 1994 Jul;107(1):271–293. doi: 10.1016/0016-5085(94)90086-8. [DOI] [PubMed] [Google Scholar]
- Mei N., Garnier L. Osmosensitive vagal receptors in the small intestine of the cat. J Auton Nerv Syst. 1986 Jul;16(3):159–170. doi: 10.1016/0165-1838(86)90022-6. [DOI] [PubMed] [Google Scholar]
- Musial F., Crowell M. D., Kalveram K. T., Enck P. Nutrient ingestion increases rectal sensitivity in humans. Physiol Behav. 1994 May;55(5):953–956. doi: 10.1016/0031-9384(94)90085-x. [DOI] [PubMed] [Google Scholar]
- Ness T. J., Gebhart G. F. Visceral pain: a review of experimental studies. Pain. 1990 May;41(2):167–234. doi: 10.1016/0304-3959(90)90021-5. [DOI] [PubMed] [Google Scholar]
- Notivol R., Coffin B., Azpiroz F., Mearin F., Serra J., Malagelada J. R. Gastric tone determines the sensitivity of the stomach to distention. Gastroenterology. 1995 Feb;108(2):330–336. doi: 10.1016/0016-5085(95)90057-8. [DOI] [PubMed] [Google Scholar]
- PAINTAL A. S. A study of gastric stretch receptors; their role in the peripheral mechanism of satiation of hunger and thirst. J Physiol. 1954 Nov 29;126(2):255–270. doi: 10.1113/jphysiol.1954.sp005207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price D. D., Long S., Huitt C. Sensory testing of pathophysiological mechanisms of pain in patients with reflex sympathetic dystrophy. Pain. 1992 May;49(2):163–173. doi: 10.1016/0304-3959(92)90139-3. [DOI] [PubMed] [Google Scholar]
- Ren K., Randich A., Gebhart G. F. Effects of electrical stimulation of vagal afferents on spinothalamic tract cells in the rat. Pain. 1991 Mar;44(3):311–319. doi: 10.1016/0304-3959(91)90102-4. [DOI] [PubMed] [Google Scholar]
- Taggart D., Billington B. P. Fatty foods and dyspersia. Lancet. 1966 Aug 27;2(7461):465–466. [PubMed] [Google Scholar]
- Whitehead W. E., Delvaux M. Standardization of barostat procedures for testing smooth muscle tone and sensory thresholds in the gastrointestinal tract. The Working Team of Glaxo-Wellcome Research, UK. Dig Dis Sci. 1997 Feb;42(2):223–241. doi: 10.1023/a:1018885028501. [DOI] [PubMed] [Google Scholar]
- Whitehead W. E., Holtkotter B., Enck P., Hoelzl R., Holmes K. D., Anthony J., Shabsin H. S., Schuster M. M. Tolerance for rectosigmoid distention in irritable bowel syndrome. Gastroenterology. 1990 May;98(5 Pt 1):1187–1192. doi: 10.1016/0016-5085(90)90332-u. [DOI] [PubMed] [Google Scholar]
- Zmarzty S. A., Wells A. S., Read N. W. The influence of food on pain perception in healthy human volunteers. Physiol Behav. 1997 Jul;62(1):185–191. doi: 10.1016/s0031-9384(97)00038-3. [DOI] [PubMed] [Google Scholar]