Abstract
The clinical and pathological findings of four females with primary biliary cirrhosis (PBC) with an unusual and hitherto not well recognised course are reported. Patients suffered severe pruritus and weight loss with progressive icteric cholestasis which did not respond to such treatments as ursodeoxycholic acid and immunosuppressives. In all cases liver histology revealed marked bile duct loss without however significant fibrosis or cirrhosis. Further diagnostic studies and repeat biopsies confirmed the absence of liver cirrhosis as well as other potential causes of hyperbilirubinaemia. Comparison of the fibrosis-ductopenia relationship for our cases with that for a group of 101 non-cirrhotic PBC patients indicated that in the former the severity of bile duct loss relative to the amount of fibrosis was significantly higher. The proportion of portal triads containing an interlobular bile duct was 3%, 4%, 6%, and 10% compared with 45% (median; range 8.3-100%) for controls (p<0.001). Three patients received a liver transplant 6-7 years after the first manifestation of PBC because of progressive cholestasis, refractory pruritus, and weight loss, while the fourth patient is considering this option. In one case cirrhosis had developed at the time of transplantation while the others still had non-cirrhotic disease. These cases suggest that cholestatic jaundice in non-cirrhotic PBC may be secondary to extensive "premature" or accelerated intrahepatic bile duct loss. Although the extent of fibrosis may be limited initially, progression to cirrhosis appears to be inevitable in the long run. Despite intact protein synthesis and absence of cirrhotic complications, liver transplantation in the pre-cirrhotic stage for preventing malnutrition and to improve quality of life should be considered for these patients. Keywords: primary biliary cirrhosis; jaundice; ductopenia; portal tract; cholestasis; liver biopsy
Full Text
The Full Text of this article is available as a PDF (195.7 KB).
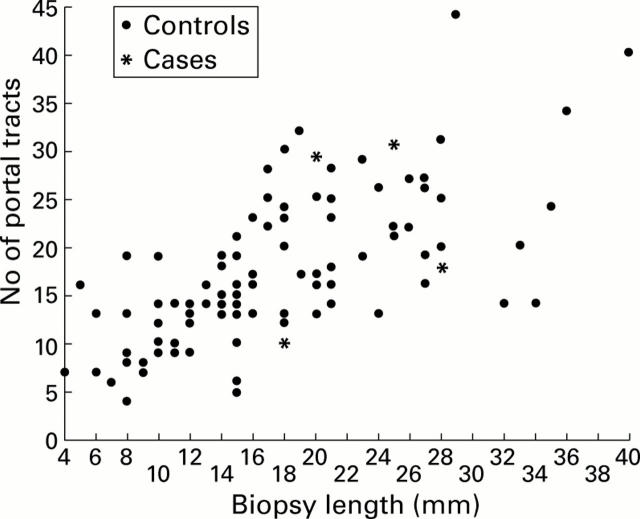
Figure 1 .
Scatterplot showing the relationship between biopsy length and number of portal tracts.
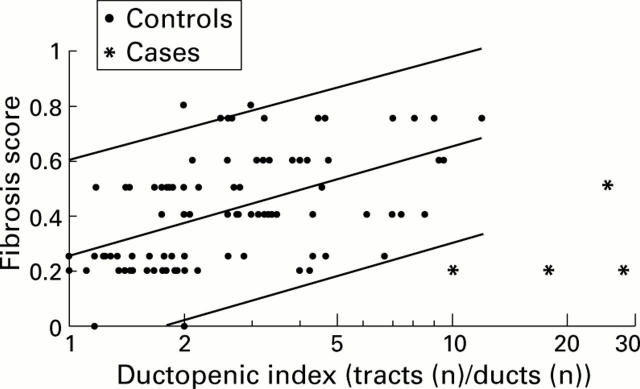
Figure 2 .
Scatterplot showing the relationship between the ductopenic index (ratio of portal tracts (n) to ducts (n)) and fibrosis score. A high index indicates severe ductopenia. The central line indicates the least squares regression line. The upper line represents the 97.5 percentile and the lower line the 2.5 percentile. Note the logarithmically scaled horizontal axis. Three of four cases fell outside the 95% reference interval of the control biopsy specimens.
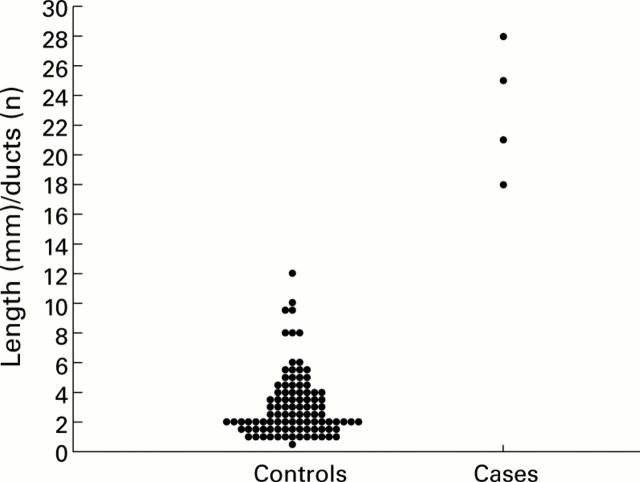
Figure 3 .
Plot showing the difference in length (mm)/ducts (n) ratio between the controls and cases. A high ratio indicates severe ductopenia.
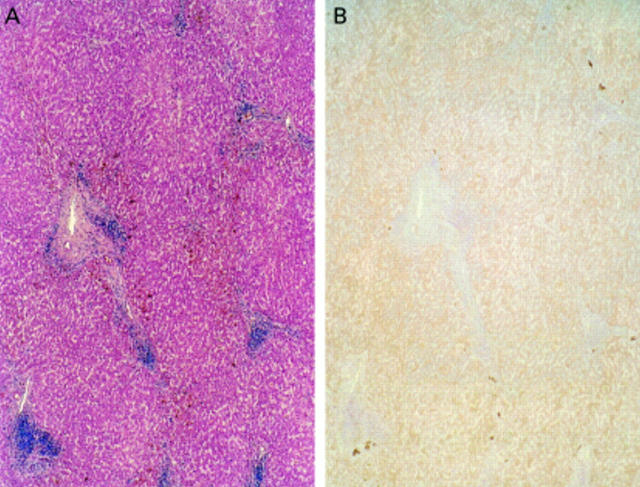
Figure 4 .
(A) Haematoxylin-eosin coloured liver biopsy from patient No 2 showing at least four portal tracts. The amount of fibrosis is very limited and there are no portoportal or portoseptal connections. (B) Anticytokeratin 19 (keratin 19) stained liver biopsy from patient No 2 showing the same portal tracts as in (A) with total absence of pre-existent interlobular bile ducts and only very moderate ductular proliferation (darkish brown coloured cells).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alvarez F., Berg P. A., Bianchi F. B., Bianchi L., Burroughs A. K., Cancado E. L., Chapman R. W., Cooksley W. G., Czaja A. J., Desmet V. J. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999 Nov;31(5):929–938. doi: 10.1016/s0168-8278(99)80297-9. [DOI] [PubMed] [Google Scholar]
- Burnett D. A., Lysenko N., Ockner R. K. Flavaspidic acid: effects on cell respiration and oxidative phosphorylation in isolated hepatocytes. Biochem Biophys Res Commun. 1979 Jul 12;89(1):116–121. doi: 10.1016/0006-291x(79)90951-3. [DOI] [PubMed] [Google Scholar]
- Chazouillères O., Wendum D., Serfaty L., Montembault S., Rosmorduc O., Poupon R. Primary biliary cirrhosis-autoimmune hepatitis overlap syndrome: clinical features and response to therapy. Hepatology. 1998 Aug;28(2):296–301. doi: 10.1002/hep.510280203. [DOI] [PubMed] [Google Scholar]
- Chen C. Y., Lu C. L., Chiu C. F., Chang F. Y., Lee S. D. Primary biliary cirrhosis associated with mixed type autoimmune hemolytic anemia and sicca syndrome: a case report and review of literature. Am J Gastroenterol. 1997 Sep;92(9):1547–1549. [PubMed] [Google Scholar]
- Crawford A. R., Lin X. Z., Crawford J. M. The normal adult human liver biopsy: a quantitative reference standard. Hepatology. 1998 Aug;28(2):323–331. doi: 10.1002/hep.510280206. [DOI] [PubMed] [Google Scholar]
- Crosbie O. M., Crown J. P., Nolan N. P., Murray R., Hegarty J. E. Resolution of paraneoplastic bile duct paucity following successful treatment of Hodgkin's disease. Hepatology. 1997 Jul;26(1):5–8. doi: 10.1002/hep.510260101. [DOI] [PubMed] [Google Scholar]
- Desmet V. J., Gerber M., Hoofnagle J. H., Manns M., Scheuer P. J. Classification of chronic hepatitis: diagnosis, grading and staging. Hepatology. 1994 Jun;19(6):1513–1520. [PubMed] [Google Scholar]
- Desmet V. J. Vanishing bile duct disorders. Prog Liver Dis. 1992;10:89–121. [PubMed] [Google Scholar]
- Desmet V. J. Vanishing bile duct syndrome in drug-induced liver disease. J Hepatol. 1997;26 (Suppl 1):31–35. doi: 10.1016/s0168-8278(97)82330-6. [DOI] [PubMed] [Google Scholar]
- Hubscher S. G., Lumley M. A., Elias E. Vanishing bile duct syndrome: a possible mechanism for intrahepatic cholestasis in Hodgkin's lymphoma. Hepatology. 1993 Jan;17(1):70–77. [PubMed] [Google Scholar]
- Kaplan M. M. Primary biliary cirrhosis. N Engl J Med. 1996 Nov 21;335(21):1570–1580. doi: 10.1056/NEJM199611213352107. [DOI] [PubMed] [Google Scholar]
- Ludwig J., Dickson E. R., McDonald G. S. Staging of chronic nonsuppurative destructive cholangitis (syndrome of primary biliary cirrhosis). Virchows Arch A Pathol Anat Histol. 1978 Aug 22;379(2):103–112. doi: 10.1007/BF00432479. [DOI] [PubMed] [Google Scholar]
- Ludwig J. Idiopathic adulthood ductopenia: an update. Mayo Clin Proc. 1998 Mar;73(3):285–291. doi: 10.4065/73.3.285. [DOI] [PubMed] [Google Scholar]
- Ludwig J., Rosen C. B., Lindor K. D., Helzberg J. H., Watson K. R. Chronic cholestasis in a young man. Hepatology. 1994 Nov;20(5):1351–1355. [PubMed] [Google Scholar]
- Mahl M. A., von Schönfeld J., Uppenkamp M., Breuer N. Hämolytische Anämie als Ursache eines auffälligen Bilirubinanstieges bei primärer biliärer Zirrhose. Dtsch Med Wochenschr. 1996 Oct 4;121(40):1226–1228. doi: 10.1055/s-2008-1043131. [DOI] [PubMed] [Google Scholar]
- Moreno A., Carreño V., Cano A., González C. Idiopathic biliary ductopenia in adults without symptoms of liver disease. N Engl J Med. 1997 Mar 20;336(12):835–838. doi: 10.1056/NEJM199703203361204. [DOI] [PubMed] [Google Scholar]
- Nakanuma Y., Hoso M., Mizuno Y., Unoura M. Pathologic study of primary biliary cirrhosis of early histologic stages presenting cholestatic jaundice. Liver. 1988 Dec;8(6):319–324. doi: 10.1111/j.1600-0676.1988.tb01010.x. [DOI] [PubMed] [Google Scholar]
- Neuberger J. Primary biliary cirrhosis. Lancet. 1997 Sep 20;350(9081):875–879. doi: 10.1016/S0140-6736(97)05419-6. [DOI] [PubMed] [Google Scholar]
- Popper H. The problem of histologic evaluation of primary biliary cirrhosis. Virchows Arch A Pathol Anat Histol. 1978 Aug 22;379(2):99–102. doi: 10.1007/BF00432478. [DOI] [PubMed] [Google Scholar]
- Schalm S. W. The diagnosis of cirrhosis: clinical relevance and methodology. J Hepatol. 1997 Dec;27(6):1118–1119. doi: 10.1016/s0168-8278(97)80159-6. [DOI] [PubMed] [Google Scholar]
- Schalm S. W., van Buuren H. R. Early cirrhosis--or primary cholangitis? Lancet. 1997 Jan 25;349(9047):285–285. doi: 10.1016/s0140-6736(05)64895-7. [DOI] [PubMed] [Google Scholar]
- Thompson N. P., Leader S., Jamieson C. P., Burnham W. R., Burroughs A. K. Reversible jaundice in primary biliary cirrhosis due to hyperthyroidism. Gastroenterology. 1994 May;106(5):1342–1343. doi: 10.1016/0016-5085(94)90028-0. [DOI] [PubMed] [Google Scholar]
- van Hoogstraten H. J., Hansen B. E., van Buuren H. R., ten Kate F. J., van Berge-Henegouwen G. P., Schalm S. W. Prognostic factors and long-term effects of ursodeoxycholic acid on liver biochemical parameters in patients with primary biliary cirrhosis. Dutch Multi-Centre PBC Study Group. J Hepatol. 1999 Aug;31(2):256–262. doi: 10.1016/s0168-8278(99)80222-0. [DOI] [PubMed] [Google Scholar]