Abstract
BACKGROUND—Patients with gastro-oesophageal reflux disease (GORD) frequently report that meals high in fat worsen heartburn. Nevertheless, studies to determine whether high fat meals promote gastro-oesophageal reflux have produced conflicting and equivocal conclusions. PATIENTS AND METHODS—To determine, alternatively, whether fat in the small intestinal lumen intensifies the perception of heartburn, we studied 11 patients with typical heartburn from GORD. After being placed on omeprazole to suppress endogenous acid, these fasting subjects underwent oesophageal perfusions with graded doses of HCl at pH values of 1.0, 1.5, 2.0, and 2.5. Oesophageal perfusions were conducted while the duodenum was perfused with saline (control) and again with fat at 8 g/h. RESULTS—Time to onset, intensity, and severity of heartburn varied with dose of oesophageal acid (p<0.01). Time to onset was significantly (p<0.01) shorter, and intensity and severity of heartburn significantly (p<0.05) greater, during duodenal perfusion with fat. CONCLUSION—We conclude that duodenal fat intensifies the perception of heartburn. Keywords: gastro-oesophageal reflux disease; heartburn; perception; fat
Full Text
The Full Text of this article is available as a PDF (147.1 KB).
Figure 1 .
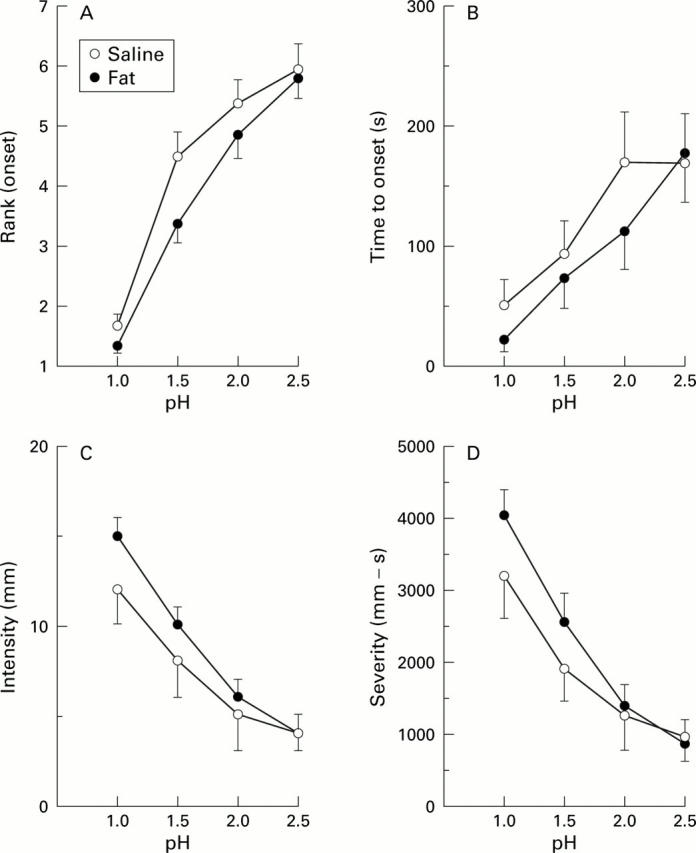
(A) Rank orders (mean (SEM) on a scale of 1-8) for times of onset of heartburn in the 11 subjects during duodenal perfusions with fat versus saline while the oesophagus was perfused with HCl at each of the four pH values (1.0, 1.5, 2.0, and 2.5). Ranks of 1.5 were assigned for oesophageal perfusions at pH 1.0 that were missing in two of the subjects (see text). (B-D) Mean (SEM) values for the 11 subjects during duodenal perfusions with fat versus saline while the oesophagus was perfused with HCl at each of four pH values. There are missing data for two of the 11 subjects when the oesophagus was perfused at pH 1.0 during duodenal instillations of fat and saline. (B) Time (seconds) to onset of heartburn (limits 0-301 seconds). (C) Perceived intensity of heartburn (mm on an analogue scale; limits 0-20 mm). (D) Severity of heartburn (duration×intensity; limits 0-6000 mm-second).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barbera R., Feinle C., Read N. W. Nutrient-specific modulation of gastric mechanosensitivity in patients with functional dyspepsia. Dig Dis Sci. 1995 Aug;40(8):1636–1641. doi: 10.1007/BF02212683. [DOI] [PubMed] [Google Scholar]
- Becker D. J., Sinclair J., Castell D. O., Wu W. C. A comparison of high and low fat meals on postprandial esophageal acid exposure. Am J Gastroenterol. 1989 Jul;84(7):782–786. [PubMed] [Google Scholar]
- Castiglione F., Emde C., Armstrong D., Bauerfeind P., Schneider C., Stacher G., Blum A. L. Oesophageal pH-metry: should meals be standardized? Scand J Gastroenterol. 1992 May;27(5):350–354. doi: 10.3109/00365529209000086. [DOI] [PubMed] [Google Scholar]
- Fass R., Naliboff B., Higa L., Johnson C., Kodner A., Munakata J., Ngo J., Mayer E. A. Differential effect of long-term esophageal acid exposure on mechanosensitivity and chemosensitivity in humans. Gastroenterology. 1998 Dec;115(6):1363–1373. doi: 10.1016/s0016-5085(98)70014-9. [DOI] [PubMed] [Google Scholar]
- Feinle C., D'Amato M., Read N. W. Cholecystokinin-A receptors modulate gastric sensory and motor responses to gastric distension and duodenal lipid. Gastroenterology. 1996 May;110(5):1379–1385. doi: 10.1053/gast.1996.v110.pm8613041. [DOI] [PubMed] [Google Scholar]
- Feinle C., Grundy D., Read N. W. Effects of duodenal nutrients on sensory and motor responses of the human stomach to distension. Am J Physiol. 1997 Sep;273(3 Pt 1):G721–G726. doi: 10.1152/ajpgi.1997.273.3.G721. [DOI] [PubMed] [Google Scholar]
- Feinle C., Grundy D., Read N. W. Fat increases vection-induced nausea independent of changes in gastric emptying. Physiol Behav. 1995 Dec;58(6):1159–1165. doi: 10.1016/0031-9384(95)02061-6. [DOI] [PubMed] [Google Scholar]
- Feinle C., Read N. W. Ondansetron reduces nausea induced by gastroduodenal stimulation without changing gastric motility. Am J Physiol. 1996 Oct;271(4 Pt 1):G591–G597. doi: 10.1152/ajpgi.1996.271.4.G591. [DOI] [PubMed] [Google Scholar]
- Galmiche J. P. Gastro-oesophageal reflux: does it matter what you eat? Gut. 1998 Mar;42(3):318–319. doi: 10.1136/gut.42.3.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holloway R. H., Lyrenas E., Ireland A., Dent J. Effect of intraduodenal fat on lower oesophageal sphincter function and gastro-oesophageal reflux. Gut. 1997 Apr;40(4):449–453. doi: 10.1136/gut.40.4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwakiri K., Kobayashi M., Kotoyori M., Yamada H., Sugiura T., Nakagawa Y. Relationship between postprandial esophageal acid exposure and meal volume and fat content. Dig Dis Sci. 1996 May;41(5):926–930. doi: 10.1007/BF02091532. [DOI] [PubMed] [Google Scholar]
- Jänig W., Khasar S. G., Levine J. D., Miao F. J. The role of vagal visceral afferents in the control of nociception. Prog Brain Res. 2000;122:273–287. doi: 10.1016/s0079-6123(08)62145-7. [DOI] [PubMed] [Google Scholar]
- Meyer J. H., Elashoff J. D., Lake R. Gastric emptying of indigestible versus digestible oils and solid fats in normal humans. Dig Dis Sci. 1999 Jun;44(6):1076–1082. doi: 10.1023/a:1026699401535. [DOI] [PubMed] [Google Scholar]
- Meyer J. H., Hlinka M., Kao D., Lake R., MacLaughlin E., Graham L. S., Elashoff J. D. Gastric emptying of oil from solid and liquid meals. Effect of human pancreatic insufficiency. Dig Dis Sci. 1996 Sep;41(9):1691–1699. doi: 10.1007/BF02088732. [DOI] [PubMed] [Google Scholar]
- Meyer J. H., Hlinka M., Tabrizi Y., DiMaso N., Raybould H. E. Chemical specificities and intestinal distributions of nutrient-driven satiety. Am J Physiol. 1998 Oct;275(4 Pt 2):R1293–R1307. doi: 10.1152/ajpregu.1998.275.4.R1293. [DOI] [PubMed] [Google Scholar]
- Meyer J. H., Tabrizi Y., DiMaso N., Hlinka M., Raybould H. E. Length of intestinal contact on nutrient-driven satiety. Am J Physiol. 1998 Oct;275(4 Pt 2):R1308–R1319. doi: 10.1152/ajpregu.1998.275.4.R1308. [DOI] [PubMed] [Google Scholar]
- Moran T. H., Baldessarini A. R., Salorio C. F., Lowery T., Schwartz G. J. Vagal afferent and efferent contributions to the inhibition of food intake by cholecystokinin. Am J Physiol. 1997 Apr;272(4 Pt 2):R1245–R1251. doi: 10.1152/ajpregu.1997.272.4.R1245. [DOI] [PubMed] [Google Scholar]
- Mélone J. Vagal receptors sensitive to lipids in the small intestine of the cat. J Auton Nerv Syst. 1986 Nov;17(3):231–241. doi: 10.1016/0165-1838(86)90060-3. [DOI] [PubMed] [Google Scholar]
- Nebel O. T., Castell D. O. Inhibition of the lower oesophageal sphincter by fat--a mechanism for fatty food intolerance. Gut. 1973 Apr;14(4):270–274. doi: 10.1136/gut.14.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nebel O. T., Castell D. O. Lower esophageal sphincter pressure changes after food ingestion. Gastroenterology. 1972 Nov;63(5):778–783. [PubMed] [Google Scholar]
- Nebel O. T., Fornes M. F., Castell D. O. Symptomatic gastroesophageal reflux: incidence and precipitating factors. Am J Dig Dis. 1976 Nov;21(11):953–956. doi: 10.1007/BF01071906. [DOI] [PubMed] [Google Scholar]
- Pehl C., Waizenhoefer A., Wendl B., Schmidt T., Schepp W., Pfeiffer A. Effect of low and high fat meals on lower esophageal sphincter motility and gastroesophageal reflux in healthy subjects. Am J Gastroenterol. 1999 May;94(5):1192–1196. doi: 10.1111/j.1572-0241.1999.01064.x. [DOI] [PubMed] [Google Scholar]
- Penagini R., Mangano M., Bianchi P. A. Effect of increasing the fat content but not the energy load of a meal on gastro-oesophageal reflux and lower oesophageal sphincter motor function. Gut. 1998 Mar;42(3):330–333. doi: 10.1136/gut.42.3.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price S. F., Smithson K. W., Castell D. O. Food sensitivity in reflux esophagitis. Gastroenterology. 1978 Aug;75(2):240–243. [PubMed] [Google Scholar]
- Randich A., Gebhart G. F. Vagal afferent modulation of nociception. Brain Res Brain Res Rev. 1992 May-Aug;17(2):77–99. doi: 10.1016/0165-0173(92)90009-b. [DOI] [PubMed] [Google Scholar]
- Welch I. M., Sepple C. P., Read N. W. Comparisons of the effects on satiety and eating behaviour of infusion of lipid into the different regions of the small intestine. Gut. 1988 Mar;29(3):306–311. doi: 10.1136/gut.29.3.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zmarzty S. A., Read N. W. An examination of the effects of isoenergetic intragastric infusions of pure macronutrients on cold pain perception in healthy human volunteers. Physiol Behav. 1999 Jan 1;65(4-5):643–648. doi: 10.1016/s0031-9384(98)00231-5. [DOI] [PubMed] [Google Scholar]