Abstract
BACKGROUND AND AIMS—Conventional short term manometry is a valuable tool in the diagnosis of achalasia but the technique may fail to detect intermittent motor events. The aim of this study was to investigate the pattern of lower oesophageal sphincter (LOS) and oesophageal pressures during prolonged recording in patients with achalasia. METHODS—Eleven patients with idiopathic achalasia were studied. Prolonged combined oesophageal pH and manometric recordings of the pharynx, LOS, and stomach were performed using a pH glass electrode and a multiple lumen assembly incorporating a Dent sleeve connected to a portable water perfused manometric system. RESULTS—LOS pressure varied during the day. Postprandial LOS pressures were lower than those recorded preprandially (1.2 v 1.8 kPa; p=0.005) and basal LOS pressures were significantly higher during phase III of the migrating motor complex than during the subsequent phase I (3.3 v 1.8 kPa; p=0.028). Complete LOS relaxations were occasionally observed in seven patients (0.48/h). Complete LOS relaxations were longer in duration than incomplete LOS relaxations (10.8 v 2.8 s; p=0.01) and 57% of complete relaxations fulfilled the criteria of a transient LOS relaxation (TLOSR). Complete LOS relaxations were associated with oesophageal pressure waves with higher amplitudes and longer durations. In addition, a higher proportion of these oesophageal pressure waves were spontaneous (55.6% v 0%; p<0.02) and multipeaked (72.7% v 0%). During prolonged manometry, high amplitude oesophageal pressure waves (>10 kPa) were recorded in six patients and retrograde oesophageal pressure waves in four, phenomena which were not observed during short term manometry. CONCLUSION—In contrast with short term stationary manometry, prolonged manometry in achalasia patients revealed the occurrence of complete LOS relaxations, TLOSRs, variations in LOS pressure associated with a meal or phase III, and high amplitude and retrograde oesophageal pressure waves. Keywords: achalasia; lower oesophageal sphincter; manometry; oesophagus
Full Text
The Full Text of this article is available as a PDF (189.7 KB).
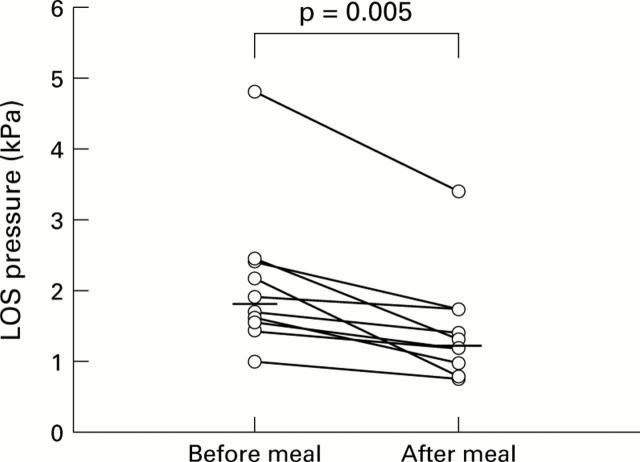
Figure 1 .
Effect of a liquid nutrient meal on basal lower oesophageal sphincter (LOS) pressure. Basal LOS pressures were significantly lower after the meal than those recorded during the one hour period preceding the meal.
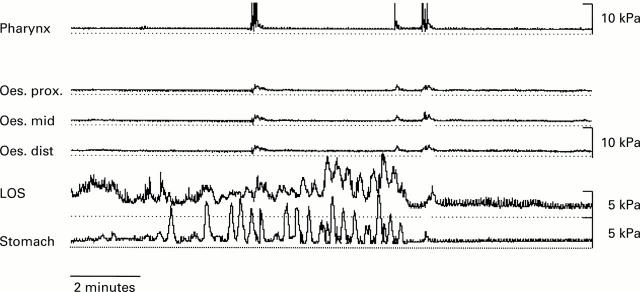
Figure 2 .
Typical example of basal lower oesophageal sphincter (LOS) pressure during phase III of the migrating motor complex cycle. The signal obtained from the intragastric sidehole shows a 3/minute rhythm. Intragastric pressure peaks exceed basal LOS pressure. Basal LOS pressure is higher during phase III than during the subsequent phase I.
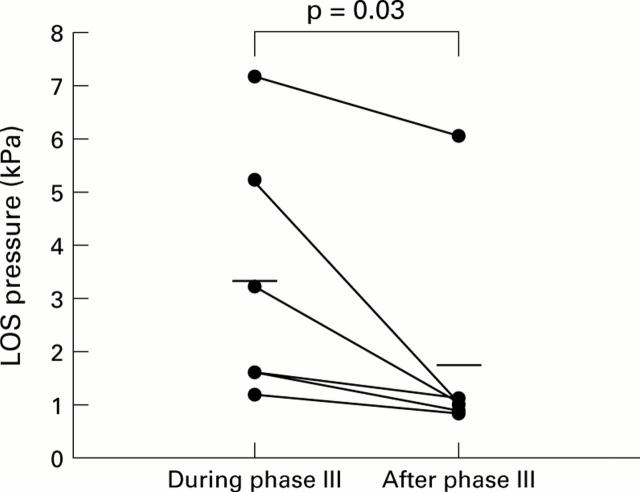
Figure 3 .
Effect of migrating motor complex (MMC) cycle activity on basal lower oesophageal sphincter (LOS) pressure. LOS pressure was significantly higher during phase III of the MMC cycle than during the 15 minute period afterwards (phase I).
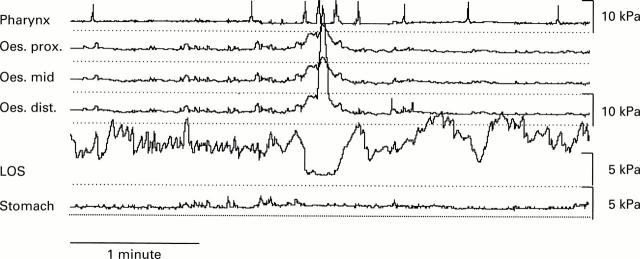
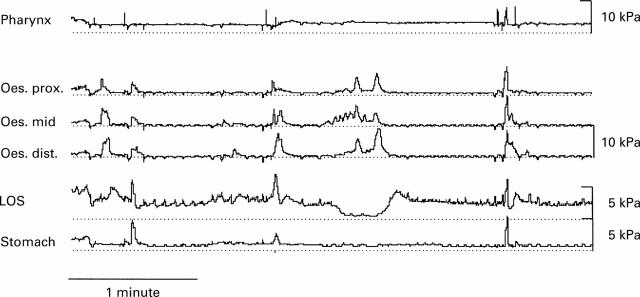
Figure 4 .
Example of a complete lower oesophageal sphincter (LOS) relaxation. This complete LOS relaxation was associated with a common cavity phenomenon and a high amplitude pressure wave (34.2 kPa) in the distal oesophagus. Several subsequent swallows were not followed by oesophageal pressure waves or LOS relaxation.
Figure 5 .
Transient lower oesophageal sphincter (LOS) relaxation. This relaxation met the criteria of a transient LOS relaxation.
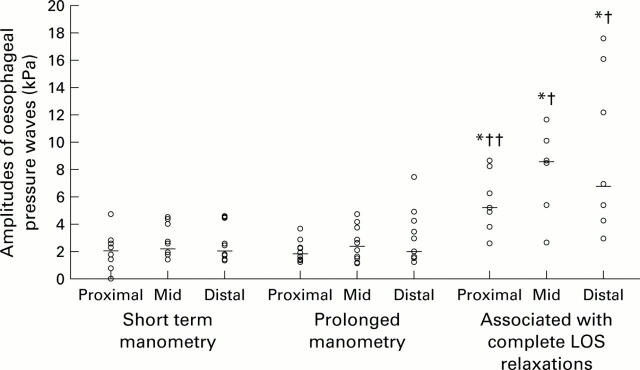
Figure 6 .
Amplitudes of oesophageal pressure waves during short term and prolonged manometry and of those associated with a complete lower oesophageal sphincter (LOS) relaxation. Oesophageal pressure waves associated with complete LOS relaxations had a higher amplitude in the proximal, mid, and distal oesophagus compared with amplitudes during short term and prolonged manometric recording. (*p<0.02 v prolonged manometry; †p<0.03, ††p< 0.05 v short term manometry).
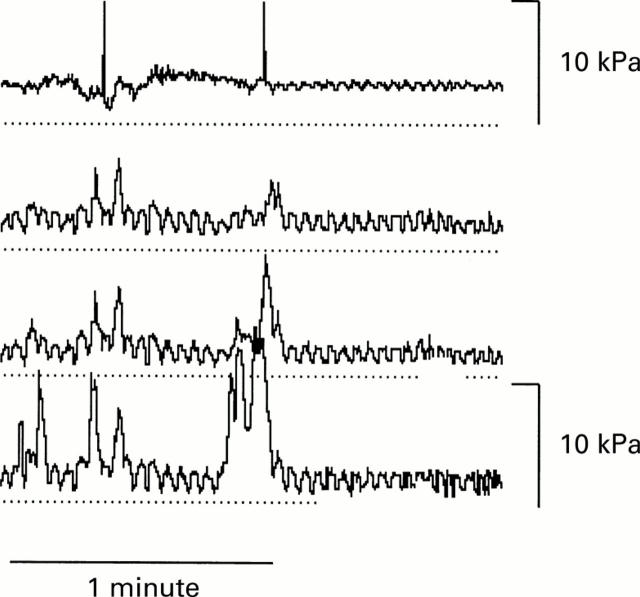
Figure 7 .
Example of a retrograde oesophageal pressure wave.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Adams C. W., Brain R. H., Trounce J. R. Ganglion cells in achalasia of the cardia. Virchows Arch A Pathol Anat Histol. 1976 Nov 22;372(1):75–79. doi: 10.1007/BF00429718. [DOI] [PubMed] [Google Scholar]
- Aggestrup S., Uddman R., Sundler F., Fahrenkrug J., Håkanson R., Sørensen H. R., Hambraeus G. Lack of vasoactive intestinal polypeptide nerves in esophageal achalasia. Gastroenterology. 1983 May;84(5 Pt 1):924–927. [PubMed] [Google Scholar]
- Benjamin S. B., Richter J. E., Cordova C. M., Knuff T. E., Castell D. O. Prospective manometric evaluation with pharmacologic provocation of patients with suspected esophageal motility dysfunction. Gastroenterology. 1983 May;84(5 Pt 1):893–901. [PubMed] [Google Scholar]
- CASSELLA R. R., BROWN A. L., Jr, SAYRE G. P., ELLIS F. H., Jr ACHALASIA OF THE ESOPHAGUS: PATHOLOGIC AND ETIOLOGIC CONSIDERATIONS. Ann Surg. 1964 Sep;160:474–487. doi: 10.1097/00000658-196409000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csendes A., Smok G., Braghetto I., González P., Henríquez A., Csendes P., Pizurno D. Histological studies of Auerbach's plexuses of the oesophagus, stomach, jejunum, and colon in patients with achalasia of the oesophagus: correlation with gastric acid secretion, presence of parietal cells and gastric emptying of solids. Gut. 1992 Feb;33(2):150–154. doi: 10.1136/gut.33.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Giorgio R., Di Simone M. P., Stanghellini V., Barbara G., Tonini M., Salvioli B., Mattioli S., Corinaldesi R. Esophageal and gastric nitric oxide synthesizing innervation in primary achalasia. Am J Gastroenterol. 1999 Sep;94(9):2357–2362. doi: 10.1111/j.1572-0241.1999.01357.x. [DOI] [PubMed] [Google Scholar]
- Dent J., Dodds W. J., Friedman R. H., Sekiguchi T., Hogan W. J., Arndorfer R. C., Petrie D. J. Mechanism of gastroesophageal reflux in recumbent asymptomatic human subjects. J Clin Invest. 1980 Feb;65(2):256–267. doi: 10.1172/JCI109667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dent J., Dodds W. J., Sekiguchi T., Hogan W. J., Arndorfer R. C. Interdigestive phasic contractions of the human lower esophageal sphincter. Gastroenterology. 1983 Mar;84(3):453–460. [PubMed] [Google Scholar]
- Dent J., Holloway R. H., Toouli J., Dodds W. J. Mechanisms of lower oesophageal sphincter incompetence in patients with symptomatic gastrooesophageal reflux. Gut. 1988 Aug;29(8):1020–1028. doi: 10.1136/gut.29.8.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Martino N., Bortolotti M., Izzo G., Maffettone V., Monaco L., Del Genio A. 24-hour esophageal ambulatory manometry in patients with achalasia of the esophagus. Dis Esophagus. 1997 Apr;10(2):121–127. doi: 10.1093/dote/10.2.121. [DOI] [PubMed] [Google Scholar]
- Dodds W. J., Dent J., Hogan W. J., Patel G. K., Toouli J., Arndorfer R. C. Paradoxical lower esophageal sphincter contraction induced by cholecystokinin-octapeptide in patients with achalasia. Gastroenterology. 1981 Feb;80(2):327–333. [PubMed] [Google Scholar]
- Dooley C. P., Taylor I. L., Valenzuela J. E. Impaired acid secretion and pancreatic polypeptide release in some patients with achalasia. Gastroenterology. 1983 Apr;84(4):809–813. [PubMed] [Google Scholar]
- Friesen D. L., Henderson R. D., Hanna W. Ultrastructure of the esophageal muscle in achalasia and diffuse esophageal spasm. Am J Clin Pathol. 1983 Mar;79(3):319–325. doi: 10.1093/ajcp/79.3.319. [DOI] [PubMed] [Google Scholar]
- Greco A. V., Bianco A., Altomonte L., D'Acquarica L., Ghirlanda G. Effect of somatostatin on lower esophageal sphincter (les) pressure and serum gastrin in normal and achalasic subjects. Horm Metab Res. 1982 Jan;14(1):26–28. doi: 10.1055/s-2007-1018911. [DOI] [PubMed] [Google Scholar]
- Guelrud M., Rossiter A., Souney P. F., Rossiter G., Fanikos J., Mujica V. The effect of vasoactive intestinal polypeptide on the lower esophageal sphincter in achalasia. Gastroenterology. 1992 Aug;103(2):377–382. doi: 10.1016/0016-5085(92)90824-i. [DOI] [PubMed] [Google Scholar]
- Guelrud M., Rossiter A., Souney P. F., Sulbaran M. Transcutaneous electrical nerve stimulation decreases lower esophageal sphincter pressure in patients with achalasia. Dig Dis Sci. 1991 Aug;36(8):1029–1033. doi: 10.1007/BF01297442. [DOI] [PubMed] [Google Scholar]
- Hall K. E., Greenberg G. R., El-Sharkawy T. Y., Diamant N. E. Relationship between porcine motilin-induced migrating motor complex-like activity, vagal integrity, and endogenous motilin release in dogs. Gastroenterology. 1984 Jul;87(1):76–85. [PubMed] [Google Scholar]
- Holloway R. H., Blank E., Takahashi I., Dodds W. J., Layman R. D. Motilin: a mechanism incorporating the opossum lower esophageal sphincter into the migrating motor complex. Gastroenterology. 1985 Sep;89(3):507–515. doi: 10.1016/0016-5085(85)90444-5. [DOI] [PubMed] [Google Scholar]
- Holloway R. H., Dodds W. J., Helm J. F., Hogan W. J., Dent J., Arndorfer R. C. Integrity of cholinergic innervation to the lower esophageal sphincter in achalasia. Gastroenterology. 1986 Apr;90(4):924–929. doi: 10.1016/0016-5085(86)90869-3. [DOI] [PubMed] [Google Scholar]
- Holloway R. H., Kocyan P., Dent J. Provocation of transient lower esophageal sphincter relaxations by meals in patients with symptomatic gastroesophageal reflux. Dig Dis Sci. 1991 Aug;36(8):1034–1039. doi: 10.1007/BF01297443. [DOI] [PubMed] [Google Scholar]
- Holloway R. H., Penagini R., Ireland A. C. Criteria for objective definition of transient lower esophageal sphincter relaxation. Am J Physiol. 1995 Jan;268(1 Pt 1):G128–G133. doi: 10.1152/ajpgi.1995.268.1.G128. [DOI] [PubMed] [Google Scholar]
- Holloway R. H., Wyman J. B., Dent J. Failure of transient lower oesophageal sphincter relaxation in response to gastric distension in patients with achalasia: evidence for neural mediation of transient lower oesophageal sphincter relaxations. Gut. 1989 Jun;30(6):762–767. doi: 10.1136/gut.30.6.762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz P. O., Richter J. E., Cowan R., Castell D. O. Apparent complete lower esophageal sphincter relaxation in achalasia. Gastroenterology. 1986 Apr;90(4):978–983. doi: 10.1016/0016-5085(86)90876-0. [DOI] [PubMed] [Google Scholar]
- Lu C., Schulze-Delrieu K., Shirazi S., Cram M., Raab J. Dynamic imaging of obstructed opossum esophagus. From altered load to altered contractility. Dig Dis Sci. 1994 Jul;39(7):1377–1388. doi: 10.1007/BF02088037. [DOI] [PubMed] [Google Scholar]
- Mearin F., Malagelada J. R. Complete lower esophageal sphincter relaxation observed in some achalasia patients is functionally inadequate. Am J Physiol Gastrointest Liver Physiol. 2000 Mar;278(3):G376–G383. doi: 10.1152/ajpgi.2000.278.3.G376. [DOI] [PubMed] [Google Scholar]
- Mittal R. K., Fisher M. J. Electrical and mechanical inhibition of the crural diaphragm during transient relaxation of the lower esophageal sphincter. Gastroenterology. 1990 Nov;99(5):1265–1268. doi: 10.1016/0016-5085(90)91148-y. [DOI] [PubMed] [Google Scholar]
- Miyata M., Sakamoto T., Hashimoto T., Nakamura M., Sakaguchi H., Kawashima Y. Effect of secretin on lower esophageal sphincter pressure in patients with esophageal achalasia. Gastroenterol Jpn. 1991 Dec;26(6):712–715. doi: 10.1007/BF02782857. [DOI] [PubMed] [Google Scholar]
- Nebel O. T., Castell D. O. Lower esophageal sphincter pressure changes after food ingestion. Gastroenterology. 1972 Nov;63(5):778–783. [PubMed] [Google Scholar]
- Ott D. J., Richter J. E., Chen Y. M., Wu W. C., Gelfand D. W., Castell D. O. Radiographic and manometric correlation in achalasia with apparent relaxation of the lower esophageal sphincter. Gastrointest Radiol. 1989 Winter;14(1):1–5. doi: 10.1007/BF01889144. [DOI] [PubMed] [Google Scholar]
- Paterson W. G. Esophageal and lower esophageal sphincter response to balloon distention in patients with achalasia. Dig Dis Sci. 1997 Jan;42(1):106–112. doi: 10.1023/a:1018893206926. [DOI] [PubMed] [Google Scholar]
- Penagini R., Bartesaghi B., Zannini P., Negri G., Bianchi P. A. Lower oesophageal sphincter hypersensitivity to opioid receptor stimulation in patients with idiopathic achalasia. Gut. 1993 Jan;34(1):16–20. doi: 10.1136/gut.34.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qualman S. J., Haupt H. M., Yang P., Hamilton S. R. Esophageal Lewy bodies associated with ganglion cell loss in achalasia. Similarity to Parkinson's disease. Gastroenterology. 1984 Oct;87(4):848–856. [PubMed] [Google Scholar]
- Samsom M., Smout A. J., Hebbard G., Fraser R., Omari T., Horowitz M., Dent J. A novel portable perfused manometric system for recording of small intestinal motility. Neurogastroenterol Motil. 1998 Apr;10(2):139–148. doi: 10.1046/j.1365-2982.1998.00093.x. [DOI] [PubMed] [Google Scholar]
- Schoeman M. N., Tippett M. D., Akkermans L. M., Dent J., Holloway R. H. Mechanisms of gastroesophageal reflux in ambulant healthy human subjects. Gastroenterology. 1995 Jan;108(1):83–91. doi: 10.1016/0016-5085(95)90011-x. [DOI] [PubMed] [Google Scholar]
- Sekiyama N., Kakumoto Y., Nakagawa S., Wada T. Studies on exogenous and endogenous interaction of gastrin and secretin in a case of achalasia. Gastroenterol Jpn. 1977;12(5):395–399. doi: 10.1007/BF02774537. [DOI] [PubMed] [Google Scholar]
- Sigala S., Missale G., Missale C., Villanacci V., Cestari R., Grigolato P. G., Lojacono L., Spano P. F. Different neurotransmitter systems are involved in the development of esophageal achalasia. Life Sci. 1995 Mar 10;56(16):1311–1320. doi: 10.1016/0024-3205(95)00082-8. [DOI] [PubMed] [Google Scholar]
- Sivri B., Mittal R. K. Reverse-perfused sleeve: an improved device for measurement of sphincteric function of the crural diaphragm. Gastroenterology. 1991 Oct;101(4):962–969. doi: 10.1016/0016-5085(91)90722-w. [DOI] [PubMed] [Google Scholar]
- Stuart R. C., Byrne P. J., Lawlor P., O'Sullivan G., Hennessy T. P. Meal area index: a new technique for quantitative assessment in achalasia by ambulatory manometry during eating. Br J Surg. 1992 Nov;79(11):1162–1166. doi: 10.1002/bjs.1800791118. [DOI] [PubMed] [Google Scholar]
- Tovar J. A., Prieto G., Molina M., Arana J. Esophageal function in achalasia: preoperative and postoperative manometric studies. J Pediatr Surg. 1998 Jun;33(6):834–838. doi: 10.1016/s0022-3468(98)90653-4. [DOI] [PubMed] [Google Scholar]
- Van Herwaarden M. A., Samsom M., Akkermans L. M., Smout A. J. Prolonged recording of oesophageal and lower oesophageal sphincter pressure using a portable water-perfused manometric system. Neurogastroenterol Motil. 2001 Apr;13(2):111–119. doi: 10.1046/j.1365-2982.2001.00253.x. [DOI] [PubMed] [Google Scholar]
- van Herwaarden M. A., Samsom M., Smout A. J. Excess gastroesophageal reflux in patients with hiatus hernia is caused by mechanisms other than transient LES relaxations. Gastroenterology. 2000 Dec;119(6):1439–1446. doi: 10.1053/gast.2000.20191. [DOI] [PubMed] [Google Scholar]