Abstract
A 67 year old woman with a history of chronic atrial fibrillation presented with asthma cardiale. She took no medication and there was no family history of long QT syndrome. She was treated with furosemide, nitroprusside, acenocoumarol, and digoxin. Two days later excessively prolonged RR intervals, which were terminated by escape beats with a right bundle branch block morphology, suggested impending total AV block. There was also severe QT (0.48 s) and QTc (0.56) interval prolongation with bizarre inverted TU waves and multifocal premature ventricular complexes within the U waves. The patient experienced angina pectoris followed by episodes of torsades de pointes, which were interpreted as the result of bradycardia, and the bradycardia as the result of high grade AV block induced by increased vagal tone caused by ischaemia in the presence of digoxin intoxication (serum digoxin was 2.5 µg/l). Subsequent atropine infusion sped up the ventricular rate and shortened the QT (0.39) and QTc (0.51) intervals. Digoxin was replaced by metoprolol to control ventricular rate and angina pectoris. Within days, QT and QTc intervals became normal and the U waves disappeared. Neither torsades de pointes nor angina pectoris recurred. Based on a review of the literature, it is suggested that the electrophysiological mechanism of this effect is not only an increase of the heart rate, but also a direct action of muscarinic receptor antagonism on Purkinje cells and ventricular refractoriness. Keywords: torsades de pointes; long QT syndrome; atropine; AV block
Full Text
The Full Text of this article is available as a PDF (131.1 KB).
Figure 1 .
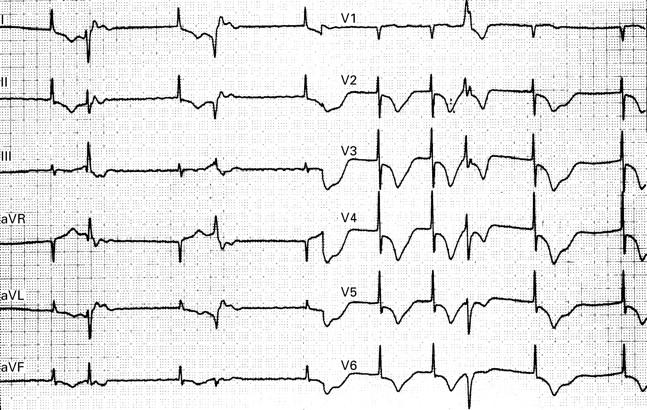
ECG two days after admission, after digoxin, in the presence of angina pectoris. Note bradycardia (50-60 beats/min) and severe QT prolongation with bizarre inverted TU waves and frequent premature ventricular complexes appearing within the U waves. QT (of the 6th beat) 0.60 s, QTc 0.57.
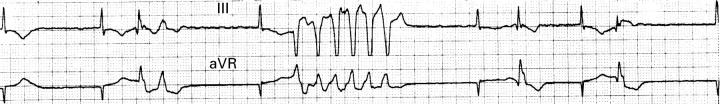
Figure 2 .
ECG shortly after that in fig 1 shows an episode of non-sustained torsades de pointes. Initiation of the tachycardia shows a typical short-long-short RR interval sequence (the 3rd beat is followed after a short pause by the 4th beat, which is followed after a long pause by the 5th beat, which is followed after a short pause by the 6th beat, which constitutes the first beat of the tachycardia).