Abstract
Objective—To determine the prevalence of sleep disordered breathing within a United Kingdom heart failure population. Subjects—104 patients and 21 matched normal volunteers. Methods—Overnight home pulse oximetry with simultaneous ECG recording in the patient group; daytime sleepiness was assessed using the Epworth sleepiness scale (ESS); 41 patients underwent polysomnography to assess the validity of oximetry as a screening test for Cheyne-Stokes respiration. Results—Home oximetry was a good screening test for Cheyne-Stokes respiration (specificity 81%, sensitivity 87%). Patients with poorer New York Heart Association (NYHA) classes had higher sleepiness scores (p < 0.005). Twenty three patients had "abnormal" patterns of nocturnal desaturation suggestive of Cheyne-Stokes respiration. The mean (SEM) frequency of dips in SaO2 exceeding 4% was 10.3 (0.9) per hour in the patients and 4.8 (0.6) in normal controls (p < 0.005). Ejection fraction correlated negatively with dip frequency (r = −0.5. p < 0.005). The patient subgroup with ⩾ 15 dips/hour had a higher mean (SEM) NYHA class (3.0 (0.2) v 2.3 (0.1), p < 0.05), and experienced more ventricular ectopy (220 (76) v 78 (21) beats/hour, p < 0.05). There was no excess of serious arrhythmia. Conclusions—Nocturnal desaturation is common in patients with treated heart failure. Low ejection fraction was related to dip frequency. Lack of correlation between dips and ESS suggests that arousal from sleep is more important than hypoxia in the aetiology of daytime sleepiness in heart failure. Overnight oximetry is a useful screening test for Cheyne-Stokes respiration in patients with known heart failure. Keywords: Cheyne-Stokes respiration; nocturnal desaturation; heart failure
Full Text
The Full Text of this article is available as a PDF (147.6 KB).
Figure 1 .
Bland and Altman plot showing the short term reproducibility of overnight home pulse oximetry in patients with controlled heart failure. ζw = 1.3 dips/h; mean difference = −0.2 dips/h; coefficient of variation = 7.9.
Figure 2 .
Receiver-operator curve demonstrating the ability of pulse oximetry to discriminate between normal breathing and Cheyne-Stokes respiration in heart failure. *Indicates a desaturation index of 15 dips/h (see text).
Figure 3 .

Sample "normal" (upper panel) and "abnormal" (lower panel) overnight oximetry recordings.
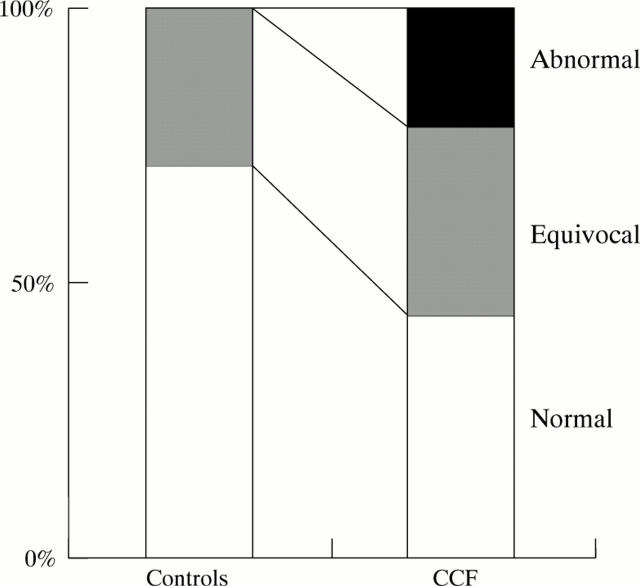
Figure 4 .
Cumulative histograms showing frequency of disordered breathing in 104 patients with chronic heart failure and 21 normal volunteers.
Figure 5 .

Relation between ejection fraction and desaturation events in all subjects.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ancoli-Israel S., Engler R. L., Friedman P. J., Klauber M. R., Ross P. A., Kripke D. F. Comparison of patients with central sleep apnea. With and without Cheyne-Stokes respiration. Chest. 1994 Sep;106(3):780–786. doi: 10.1378/chest.106.3.780. [DOI] [PubMed] [Google Scholar]
- Blackshear J. L., Kaplan J., Thompson R. C., Safford R. E., Atkinson E. J. Nocturnal dyspnea and atrial fibrillation predict Cheyne-Stokes respirations in patients with congestive heart failure. Arch Intern Med. 1995 Jun 26;155(12):1297–1302. [PubMed] [Google Scholar]
- Cripps T., Rocker G., Stradling J. Nocturnal hypoxia and arrhythmias in patients with impaired left ventricular function. Br Heart J. 1992 Oct;68(4):382–386. doi: 10.1136/hrt.68.10.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findley L. J., Zwillich C. W., Ancoli-Israel S., Kripke D., Tisi G., Moser K. M. Cheyne-Stokes breathing during sleep in patients with left ventricular heart failure. South Med J. 1985 Jan;78(1):11–15. doi: 10.1097/00007611-198501000-00004. [DOI] [PubMed] [Google Scholar]
- Hanly P. J., Millar T. W., Steljes D. G., Baert R., Frais M. A., Kryger M. H. Respiration and abnormal sleep in patients with congestive heart failure. Chest. 1989 Sep;96(3):480–488. doi: 10.1378/chest.96.3.480. [DOI] [PubMed] [Google Scholar]
- Hanly P. J., Millar T. W., Steljes D. G., Baert R., Frais M. A., Kryger M. H. The effect of oxygen on respiration and sleep in patients with congestive heart failure. Ann Intern Med. 1989 Nov 15;111(10):777–782. doi: 10.7326/0003-4819-111-10-777. [DOI] [PubMed] [Google Scholar]
- Hanly P. J., Zuberi-Khokhar N. S. Increased mortality associated with Cheyne-Stokes respiration in patients with congestive heart failure. Am J Respir Crit Care Med. 1996 Jan;153(1):272–276. doi: 10.1164/ajrccm.153.1.8542128. [DOI] [PubMed] [Google Scholar]
- Javaheri S., Parker T. J., Wexler L., Michaels S. E., Stanberry E., Nishyama H., Roselle G. A. Occult sleep-disordered breathing in stable congestive heart failure. Ann Intern Med. 1995 Apr 1;122(7):487–492. doi: 10.7326/0003-4819-122-7-199504010-00002. [DOI] [PubMed] [Google Scholar]
- Johns M. W. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991 Dec;14(6):540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- Johns M. W. Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth Sleepiness Scale. Chest. 1993 Jan;103(1):30–36. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- Packer M. Sudden unexpected death in patients with congestive heart failure: a second frontier. Circulation. 1985 Oct;72(4):681–685. doi: 10.1161/01.cir.72.4.681. [DOI] [PubMed] [Google Scholar]
- Stradling J. R., Crosby J. H. Predictors and prevalence of obstructive sleep apnoea and snoring in 1001 middle aged men. Thorax. 1991 Feb;46(2):85–90. doi: 10.1136/thx.46.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warley A. R., Mitchell J. H., Stradling J. R. Evaluation of the Ohmeda 3700 pulse oximeter. Thorax. 1987 Nov;42(11):892–896. doi: 10.1136/thx.42.11.892. [DOI] [PMC free article] [PubMed] [Google Scholar]