Abstract
Objective—To assess possible ECG changes caused by dobutamine stress and their relation to wall motion disturbances in patients with coronary artery disease. Design—Prospective recording and analysis of 12 lead ECG at rest and during each stage of dobutamine stress echocardiography, and correlation with wall motion changes. Setting—A tertiary referral centre for cardiac disease equipped with non-invasive facilities for pharmacological stress tests. Subjects—27 patients, mean (SD) age 60 (8) years, with documented evidence of coronary artery disease in whom dobutamine stress echo was clinically indicated, and 17 controls of similar age. Results—In controls, all ECG intervals shortened with increasing heart rate but in the patient group only PR and QT intervals shortened while QRS duration broadened and QTc interval prolonged progressively. In the 27 patients, 16 developed chest pain, 15 with reduced left ventricular long axis systolic excursion (p < 0.001), and all showed reduced peak lengthening rate; ST segment shift appeared in 16, 13 of whom developed chest pain, but did not correlate with reduction of either systolic long axis excursion or peak lengthening rate; QRS duration broadened in 20, 16 with reduction of long axis excursion (p < 0.02) which was more often seen at the septum (p < 0.005); QTc interval prolonged in 19, all of whom had associated reduction of peak long axis lengthening rate (p < 0.02). Conclusions—QRS duration and QTc interval both normally shorten with dobutamine stress, while in coronary artery disease they both lengthen: changes in QRS duration correlate with systolic and QTc interval with diastolic left ventricular wall motion disturbances. ST segment shift also occurred in most patients, but without consistent correlation with wall motion abnormalities. It was thus less discriminating than the other two abnormalities in this respect. Keywords: long axis; QRS duration; QTc interval; stress echocardiography; coronary artery disease
Full Text
The Full Text of this article is available as a PDF (155.5 KB).
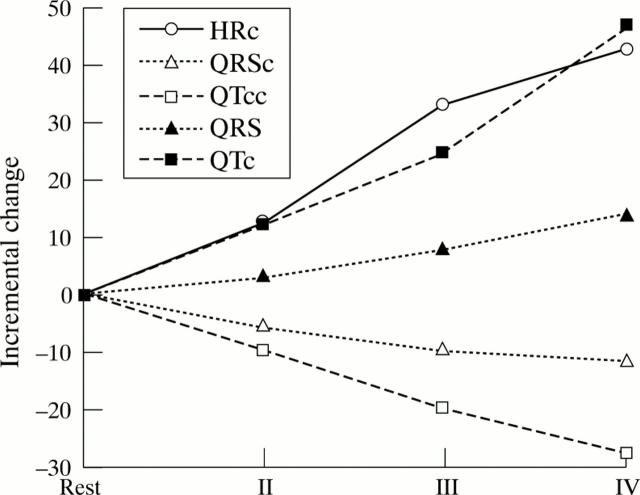
Figure 1 .
A graph showing the incremental change in heart rate, QRS duration, and QTc interval during dobutamine stress. Note the trend of divergence between patients and controls with increase in heart rate: a consistent shortening of intervals in controls and prolongation in patients.
Figure 2 .
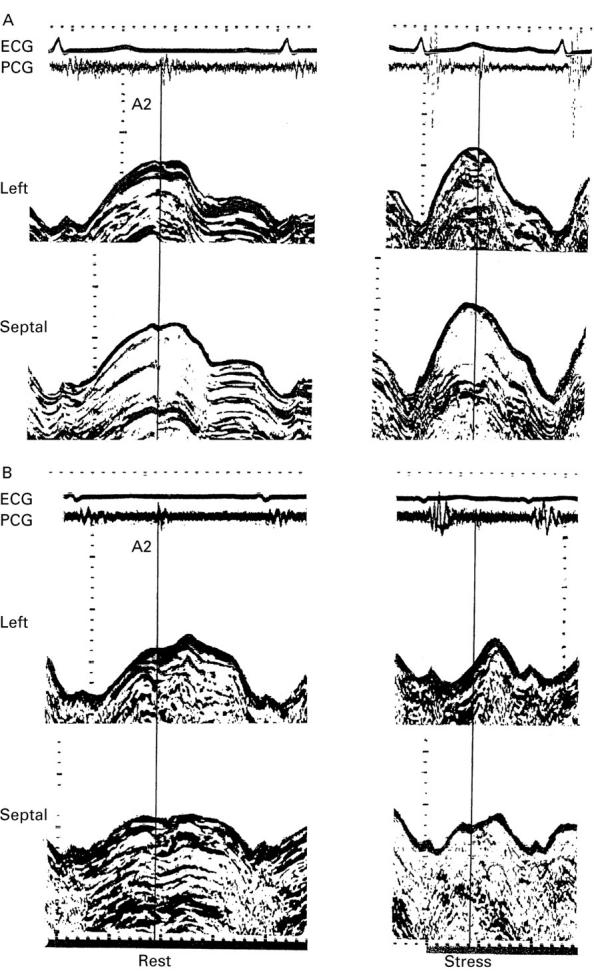
(A) M mode recording of left (top) and septal (below) long axis at rest (left) and peak stress (right) taken from a control. (B) Similar recordings taken from a patient with coronary artery disease. Note the increase in long axis amplitude of systolic excursion and lengthening velocity with stress in the control and the reduction of both in the patient.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahnve S., Sullivan M., Myers J., Froelicher V. Computer analysis of exercise-induced changes in QRS duration in patients with angina pectoris and in normal subjects. Am Heart J. 1986 May;111(5):903–908. doi: 10.1016/0002-8703(86)90640-x. [DOI] [PubMed] [Google Scholar]
- Alam M., Höglund C., Thorstrand C., Hellekant C. Haemodynamic significance of the atrioventricular plane displacement in patients with coronary artery disease. Eur Heart J. 1992 Feb;13(2):194–200. doi: 10.1093/oxfordjournals.eurheartj.a060146. [DOI] [PubMed] [Google Scholar]
- Alam M. The atrioventricular plane displacement as a means of evaluating left ventricular systolic function in acute myocardial infarction. Clin Cardiol. 1991 Jul;14(7):588–594. doi: 10.1002/clc.4960140711. [DOI] [PubMed] [Google Scholar]
- Gibson D. G., Brown D. Measurement of instantaneous left ventricular dimension and filling rate in man, using echocardiography. Br Heart J. 1973 Nov;35(11):1141–1149. doi: 10.1136/hrt.35.11.1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenbaum R. A., Ho S. Y., Gibson D. G., Becker A. E., Anderson R. H. Left ventricular fibre architecture in man. Br Heart J. 1981 Mar;45(3):248–263. doi: 10.1136/hrt.45.3.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henein M. Y., O'Sullivan C., Davies S. W., Sigwart U., Gibson D. G. Effects of acute coronary occlusion and previous ischaemic injury on left ventricular wall motion in humans. Heart. 1997 Apr;77(4):338–345. doi: 10.1136/hrt.77.4.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henein M. Y., Priestley K., Davarashvili T., Buller N., Gibson D. G. Early changes in left ventricular subendocardial function after successful coronary angioplasty. Br Heart J. 1993 Jun;69(6):501–506. doi: 10.1136/hrt.69.6.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones C. J., Raposo L., Gibson D. G. Functional importance of the long axis dynamics of the human left ventricle. Br Heart J. 1990 Apr;63(4):215–220. doi: 10.1136/hrt.63.4.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis R. P., Rittogers S. E., Froester W. F., Boudoulas H. A critical review of the systolic time intervals. Circulation. 1977 Aug;56(2):146–158. doi: 10.1161/01.cir.56.2.146. [DOI] [PubMed] [Google Scholar]
- Nonogi H., Hess O. M., Ritter M., Krayenbuehl H. P. Diastolic properties of the normal left ventricle during supine exercise. Br Heart J. 1988 Jul;60(1):30–38. doi: 10.1136/hrt.60.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pai R. G., Bodenheimer M. M., Pai S. M., Koss J. H., Adamick R. D. Usefulness of systolic excursion of the mitral anulus as an index of left ventricular systolic function. Am J Cardiol. 1991 Jan 15;67(2):222–224. doi: 10.1016/0002-9149(91)90453-r. [DOI] [PubMed] [Google Scholar]
- Xiao H. B., Brecker S. J., Gibson D. G. Effects of abnormal activation on the time course of the left ventricular pressure pulse in dilated cardiomyopathy. Br Heart J. 1992 Oct;68(4):403–407. doi: 10.1136/hrt.68.10.403. [DOI] [PMC free article] [PubMed] [Google Scholar]