Abstract
Objective—To determine whether a programme of simple, moderate exercise training increases blood volume and improves orthostatic tolerance in patients with attacks of syncope or near syncope related to orthostatic stress. Design—An open study in 14 patients referred with unexplained attacks of syncope, who were shown to have a low tolerance to an orthostatic stress test. Measurements were made of plasma and blood volumes, orthostatic tolerance to a test of combined head up tilt and lower body suction, and baroreceptor sensitivity by applying subatmospheric pressures to a chamber over the neck. Cardiorespiratory fitness was assessed from the relation between heart rate and oxygen uptake during a graded treadmill exercise test. Assessments were made before and after undertaking an exercise training programme (Canadian Air Force 5BX/XBX). Results—After the training period, 12 of the 14 patients showed evidence of improved cardiorespiratory fitness. All 12 patients were symptomatically improved; they showed increases in plasma and blood volumes and in orthostatic tolerance, and decreases in baroreceptor sensitivity. Despite the improved orthostatic tolerance, values of blood pressure both while supine and initially following tilting were lower than before training. Conclusions—Exercise training has a role in the management of patients with syncope and poor orthostatic tolerance. It improves symptoms and increases orthostatic tolerance without increasing resting blood pressure. Keywords: orthostasis; syncope; baroreceptors; exercise
Full Text
The Full Text of this article is available as a PDF (128.5 KB).
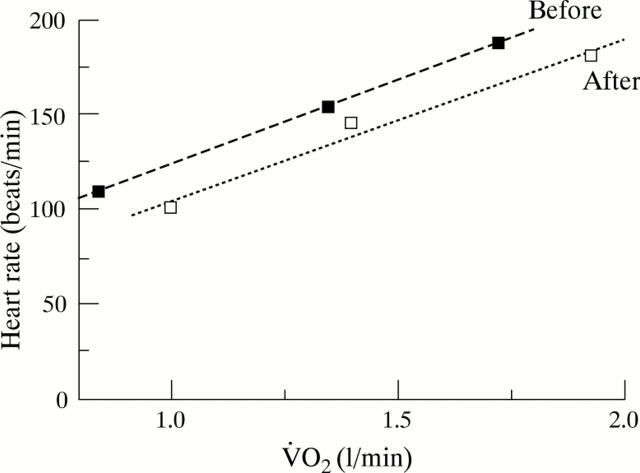
Figure 1 .
Relations between heart rate and oxygen consumption during exercise in one of the patients before and after undertaking the training programme. The lines are the linear regression and show the lower heart rates after training, at corresponding levels of oxygen consumption.
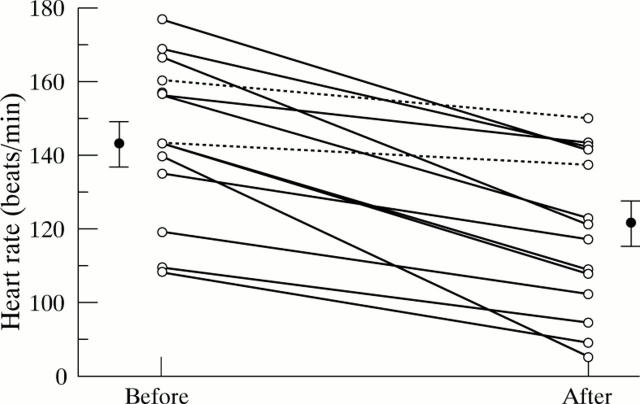
Figure 2 .
Values of heart rate taken from the regression lines (for example, fig 1) at values of oxygen consumption (V̇O2) of 1.5 l/min. Points shown are values before and after training. Solid points with bars are the means with SE from all points. The dashed lines are the data from the two subjects in whom the change in the elevation of the regression line did not reach statistical significance. After training, all patients had lower values of heart rate at a V̇O2 of 1.5 l/min.
Figure 3 .
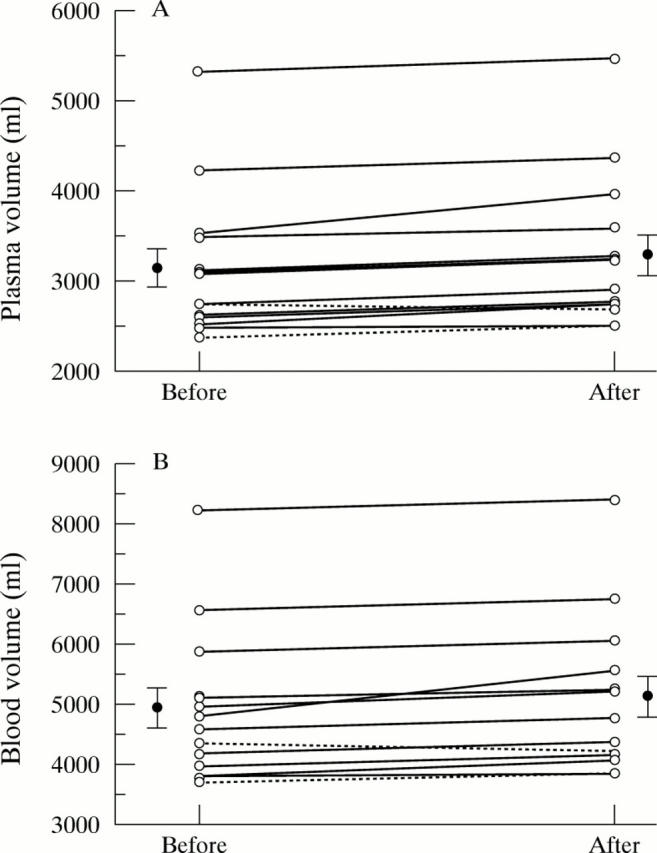
Values of plasma volume before and after training. Points joined by dashed lines are from patients who failed to show a significant change in the slope of the heart rate to V̇O2 relation.
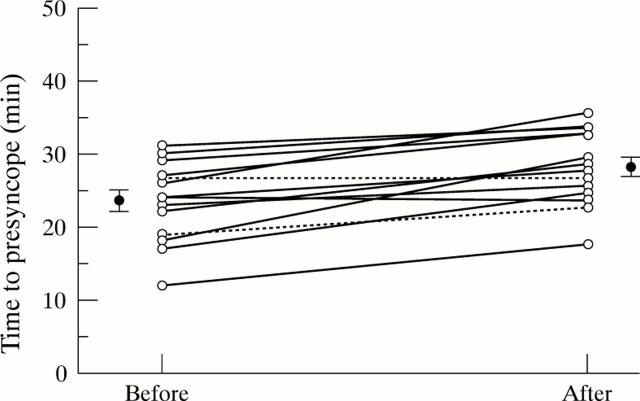
Figure 4 .
Values of orthostatic tolerance (time to presyncope) in patients before and after training. The stages of the test were: 0-20 minutes, head up tilt; 20-30 minutes, tilt and lower body suction at −20 mm Hg; after 30 minutes, tilt and lower body suction at −40 mm Hg. Dashed lines are from patients failing to show significant change in heart rate to V̇O2 relation. All other patients showed increased tolerance, with eight changing up to the next stress level.
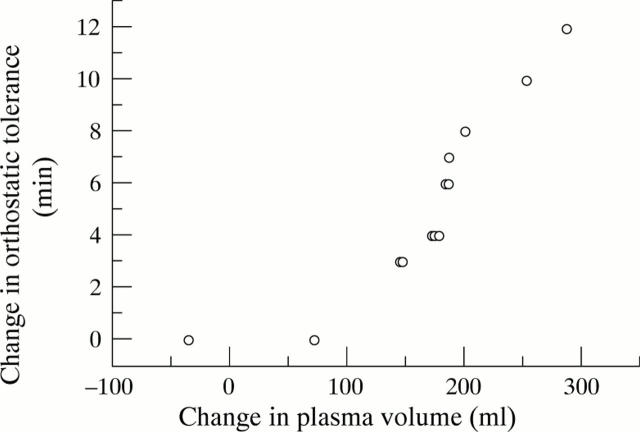
Figure 5 .
Relation between change in orthostatic tolerance and change in plasma volume. Note that all patents who showed increases in plasma volume of 150 ml or more showed increases in orthostatic tolerance.
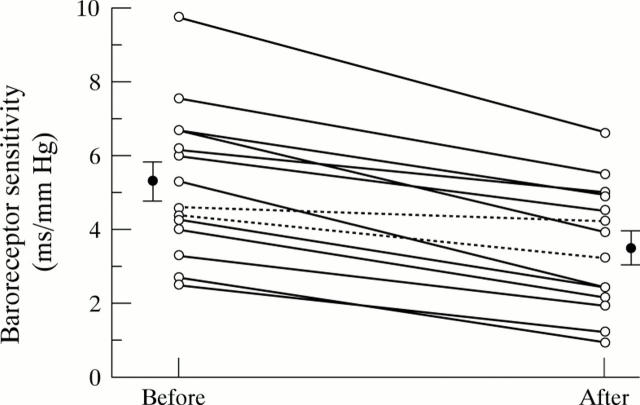
Figure 6 .
Effects of training on baroreceptor sensitivity. Baroreceptor sensitivity decreased in all patients, although in one of those who did not show a significant change in the heart rate/V̇O2 slope, baroreceptor sensitivity did not change outside the error of the method.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bruce R. A. Exercise testing for evaluation of ventricular function. N Engl J Med. 1977 Mar 24;296(12):671–675. doi: 10.1056/NEJM197703242961206. [DOI] [PubMed] [Google Scholar]
- Chan W. L., Kong C. W., Chang M. S., Chiang B. N. Exacerbation of vasodepressor syncope by beta-adrenergic blockade. N Engl J Med. 1991 Apr 25;324(17):1219–1220. doi: 10.1056/NEJM199104253241716. [DOI] [PubMed] [Google Scholar]
- Cotes J. E., Berry G., Burkinshaw L., Davies C. T., Hall A. M., Jones P. R., Knibbs A. V. Cardiac frequency during submaximal exercise in young adults; relation to lean body mass, total body potassium and amount of leg muscle. Q J Exp Physiol Cogn Med Sci. 1973 Jul;58(3):239–250. doi: 10.1113/expphysiol.1973.sp002212. [DOI] [PubMed] [Google Scholar]
- El-Sayed H., Hainsworth R. Salt supplement increases plasma volume and orthostatic tolerance in patients with unexplained syncope. Heart. 1996 Feb;75(2):134–140. doi: 10.1136/hrt.75.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick A. P., Theodorakis G., Vardas P., Sutton R. Methodology of head-up tilt testing in patients with unexplained syncope. J Am Coll Cardiol. 1991 Jan;17(1):125–130. doi: 10.1016/0735-1097(91)90714-k. [DOI] [PubMed] [Google Scholar]
- Greenleaf J. E., Sciaraffa D., Shvartz E., Keil L. C., Brock P. J. Exercise training hypotension: implications for plasma volume, renin, and vasopressin. J Appl Physiol Respir Environ Exerc Physiol. 1981 Aug;51(2):298–305. doi: 10.1152/jappl.1981.51.2.298. [DOI] [PubMed] [Google Scholar]
- Hammond M. C., Davis D. L., Dow P. Segmental responses of dog paw vasculature. Circ Res. 1968 Jul;23(1):1–9. doi: 10.1161/01.res.23.1.1. [DOI] [PubMed] [Google Scholar]
- Kapoor W. N., Brant N. Evaluation of syncope by upright tilt testing with isoproterenol. A nonspecific test. Ann Intern Med. 1992 Mar 1;116(5):358–363. doi: 10.7326/0003-4819-116-5-358. [DOI] [PubMed] [Google Scholar]
- Kappagoda C. T., Linden R. J., Newell J. P. Effect of the Canadian Air Force training programme on a submaximal exercise test. Q J Exp Physiol Cogn Med Sci. 1979 Jul;64(3):185–204. doi: 10.1113/expphysiol.1979.sp002472. [DOI] [PubMed] [Google Scholar]
- McClellan K. J., Wiseman L. R., Wilde M. I. Midodrine. A review of its therapeutic use in the management of orthostatic hypotension. Drugs Aging. 1998 Jan;12(1):76–86. doi: 10.2165/00002512-199812010-00007. [DOI] [PubMed] [Google Scholar]
- Mungall I. P., Hainsworth R. An objective assessment of the value of exercise training to patients with chronic obstructive airways disease. Q J Med. 1980 Winter;49(193):77–85. [PubMed] [Google Scholar]
- Raffo J. A., Luksic I. Y., Kappagoda C. T., Mary D. A., Whitaker W., Linden R. J. Effects of physical training on myocardial ischaemia in patients with coronary artery disease. Br Heart J. 1980 Mar;43(3):262–269. doi: 10.1136/hrt.43.3.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M. L., Raven P. B. Cardiovascular responses to lower body negative pressure in endurance and static exercise-trained men. Med Sci Sports Exerc. 1986 Oct;18(5):545–550. [PubMed] [Google Scholar]
- Sra J. S., Jazayeri M. R., Avitall B., Dhala A., Deshpande S., Blanck Z., Akhtar M. Comparison of cardiac pacing with drug therapy in the treatment of neurocardiogenic (vasovagal) syncope with bradycardia or asystole. N Engl J Med. 1993 Apr 15;328(15):1085–1090. doi: 10.1056/NEJM199304153281504. [DOI] [PubMed] [Google Scholar]
- Wahbha M. M., Morley C. A., al-Shamma Y. M., Hainsworth R. Cardiovascular reflex responses in patients with unexplained syncope. Clin Sci (Lond) 1989 Nov;77(5):547–553. doi: 10.1042/cs0770547. [DOI] [PubMed] [Google Scholar]
- el-Bedawi K. M., Hainsworth R. Combined head-up tilt and lower body suction: a test of orthostatic tolerance. Clin Auton Res. 1994 Apr;4(1-2):41–47. doi: 10.1007/BF01828837. [DOI] [PubMed] [Google Scholar]
- el-Bedawi K. M., Wahbha M. A., Hainsworth R. Cardiac pacing does not improve orthostatic tolerance in patients with vasovagal syncope. Clin Auton Res. 1994 Oct;4(5):233–237. doi: 10.1007/BF01827427. [DOI] [PubMed] [Google Scholar]
- el-Sayed H., Goodall S. R., Hainsworth R. Re-evaluation of Evans blue dye dilution method of plasma volume measurement. Clin Lab Haematol. 1995 Jun;17(2):189–194. [PubMed] [Google Scholar]
- el-Sayed H., Hainsworth R. Relationship between plasma volume, carotid baroreceptor sensitivity and orthostatic tolerance. Clin Sci (Lond) 1995 Apr;88(4):463–470. doi: 10.1042/cs0880463. [DOI] [PubMed] [Google Scholar]