Abstract
BACKGROUND—Non-cardiac chest pain assessed by cardiologists in their outpatient clinics or by coronary angiography usually has a poor symptomatic functional and psychological outcome. Randomised trials have shown the effectiveness of specialist psychological treatment with those who have persistent symptoms, but such treatment is not always acceptable to patients and may not be feasible in routine clinical settings. OBJECTIVES—To describe a sample of patients referred to cardiac outpatient clinics from primary care in a single health district who were consecutively reassured by cardiologists that there was not a cardiac cause for their presenting symptom of chest pain. DESIGN—Systematic recording of referral and medical information of patients consecutively reassured by cardiologists. Reassessment in research clinic six weeks later (with a view to inclusion in a randomised trial of psychological treatment, which has been separately reported) and followed up at six months. SETTING—A cardiac clinic in a teaching hospital providing a district service to patients referred from primary care. PATIENTS—133 patients from the Oxfordshire district presenting with chest pain and consecutively reassured that there was no cardiac cause during the recruitment period; 69 had normal coronary angiograms and 64 were reassured without angiography. INTERVENTION—A subgroup (n = 56) with persistent disabling chest pain at six weeks were invited to take part in a randomised controlled trial of cognitive behavioural treatment. MAIN OUTCOME MEASURES—Standardised interview and self report measures of chest pain, other physical symptoms, mood and anxiety, everyday activities, and beliefs about the cause of symptoms at six week assessment; repeat of self report measures at six months. RESULTS—Patients had a good outcome at six weeks, but most had persistent, clinically significant symptoms and distress. Some found the six week assessment and discussion useful. The psychological treatment was helpful to most of those recruited to the treatment trial, but a minority (15%) of those treated appeared to need more intensive and individual collaborative management. Patients reassured following angiography were compared with those reassured without invasive investigation. They had longer histories of chest pain, more often reported breathlessness on exertion, and were more likely to have previously been diagnosed as having angina, treated with antianginal medication, and admitted to hospital as emergencies. CONCLUSION—These findings suggest a need for "stepped" aftercare, with management tailored according to clinical need. This may range from simple reassurance and explanation in the cardiac clinic to more intensive individual psychological treatment of associated underlying and often enduring psychological problems. Simple ways in which the cardiologist might improve care to patients with non-cardiac chest pain are suggested, and the need for access to specialist psychological treatment discussed. Keywords: non-cardiac chest pain; psychological problems; cognitive behavioural treatment
Full Text
The Full Text of this article is available as a PDF (108.8 KB).
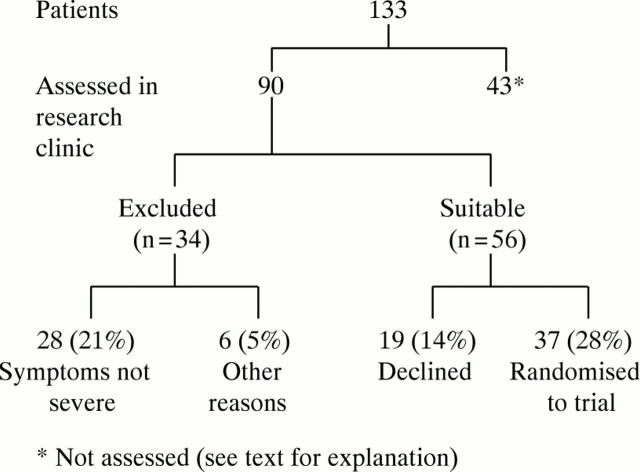
Figure 1 .
Flow chart of consecutive patients attending research clinic during 16 month period.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chambers J. Chest pain: heart, body or mind? J Psychosom Res. 1997 Aug;43(2):161–165. doi: 10.1016/s0022-3999(97)00021-4. [DOI] [PubMed] [Google Scholar]
- Derogatis L. R., Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983 Aug;13(3):595–605. [PubMed] [Google Scholar]
- Jain D., Fluck D., Sayer J. W., Ray S., Paul E. A., Timmis A. D. One-stop chest pain clinic can identify high cardiac risk. J R Coll Physicians Lond. 1997 Jul-Aug;31(4):401–404. [PMC free article] [PubMed] [Google Scholar]
- Klimes I., Mayou R. A., Pearce M. J., Coles L., Fagg J. R. Psychological treatment for atypical non-cardiac chest pain: a controlled evaluation. Psychol Med. 1990 Aug;20(3):605–611. doi: 10.1017/s0033291700017116. [DOI] [PubMed] [Google Scholar]
- Lloyd G., Cooper A., Jackson G. Information delivery: the provision of written information for patients following coronary angiography and post-discharge management. Int J Clin Pract. 1997 Sep;51(6):387–388. [PubMed] [Google Scholar]
- Mayou R. A., Bryant B. M., Sanders D., Bass C., Klimes I., Forfar C. A controlled trial of cognitive behavioural therapy for non-cardiac chest pain. Psychol Med. 1997 Sep;27(5):1021–1031. doi: 10.1017/s0033291797005254. [DOI] [PubMed] [Google Scholar]
- Mayou R., Bryant B., Forfar C., Clark D. Non-cardiac chest pain and benign palpitations in the cardiac clinic. Br Heart J. 1994 Dec;72(6):548–553. doi: 10.1136/hrt.72.6.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby D. E., Fox K. A., Flint L. L., Boon N. A. A 'same day' direct-access chest pain clinic: improved management and reduced hospitalization. QJM. 1998 May;91(5):333–337. doi: 10.1093/qjmed/91.5.333. [DOI] [PubMed] [Google Scholar]
- Pilowsky I. Dimensions of hypochondriasis. Br J Psychiatry. 1967 Jan;113(494):89–93. doi: 10.1192/bjp.113.494.89. [DOI] [PubMed] [Google Scholar]
- Potts S. G., Bass C. M. Psychological morbidity in patients with chest pain and normal or near-normal coronary arteries: a long-term follow-up study. Psychol Med. 1995 Mar;25(2):339–347. doi: 10.1017/s0033291700036242. [DOI] [PubMed] [Google Scholar]
- Speckens A. E., van Hemert A. M., Spinhoven P., Hawton K. E., Bolk J. H., Rooijmans H. G. Cognitive behavioural therapy for medically unexplained physical symptoms: a randomised controlled trial. BMJ. 1995 Nov 18;311(7016):1328–1332. doi: 10.1136/bmj.311.7016.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]