Abstract
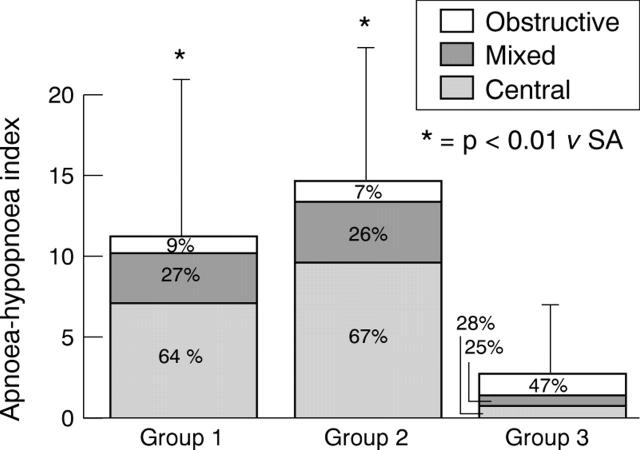
OBJECTIVE—To evaluate the incidence of sleep apnoea in acute and chronic coronary syndromes. DESIGN—Analysis of sleep and breathing characteristics in a polysomnographic study. SETTING—Cardiology department in tertiary referral centre. PATIENTS—23 patients were studied soon after acute myocardial infarction (group 1), 22 after clinical stabilisation of unstable angina (group 2), and 22 who had stable angina (group 3). Conditions liable to cause sleep apnoea, such as obesity, chronic obstructive pulmonary disease, neurological disorders, or the use of benzodiazepines, were exclusion criteria. MAIN OUTCOME MEASURES—Sleep apnoea and hypopnoea, oxygen saturation, and sleep indices evaluated soon after clinical stabilisation in groups 1 and 2 and also in group 3. RESULTS—Sleep apnoea, mainly of the central type, was equally present in groups 1 and 2 (mean (SD) apnoea-hypopnoea index: 11.10 (19.42) and 14.79 (20.52), respectively) and more severe than in group 3 (2.82 (6.43), p < 0.01). Total time spent at SaO2 < 90%, although significantly greater in group 1 and 2 (0.89 (2.4), 1.42 (3.23) min) than in group 3 (0.01 (0.05) min, p < 0.05), was clinically irrelevant. More arousals per hour of sleep (p < 0.05) were detected in group 1 (5.15 (3.71)) and group 2 (5.31 (2.14)) than in group 3 (2.83 (1.51)). CONCLUSIONS—Sleep apnoea, chiefly of the central type, not only characterises acute myocardial infarction, as found by others, but also unstable angina studied after recent stabilisation. Patient selection by exclusion of other causes of breathing disorders shows that coronary disease related apnoea is absent in the chronic coronary syndrome. In acute syndromes the lack of clinically significant apnoea related oxygen desaturation, together with the low associated incidence of major ischaemic and arrhythmic events, suggests that sleep apnoea is benign in these circumstances, despite a worsening of sleep quality. Keywords: acute myocardial infarction; unstable angina; stable angina; sleep apnoea
Full Text
The Full Text of this article is available as a PDF (91.3 KB).
Figure 1 .
Respiratory events during sleep. Percentages indicate relative distribution of central, mixed, and obstructive events.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Andreas S., Schulz R., Werner G. S., Kreuzer H. Prevalence of obstructive sleep apnoea in patients with coronary artery disease. Coron Artery Dis. 1996 Jul;7(7):541–545. [PubMed] [Google Scholar]
- Bokinsky G., Miller M., Ault K., Husband P., Mitchell J. Spontaneous platelet activation and aggregation during obstructive sleep apnea and its response to therapy with nasal continuous positive airway pressure. A preliminary investigation. Chest. 1995 Sep;108(3):625–630. doi: 10.1378/chest.108.3.625. [DOI] [PubMed] [Google Scholar]
- Bradley T. D., Floras J. S. Pathophysiologic and therapeutic implications of sleep apnea in congestive heart failure. J Card Fail. 1996 Sep;2(3):223–240. doi: 10.1016/s1071-9164(96)80045-5. [DOI] [PubMed] [Google Scholar]
- Davies R. J., Belt P. J., Roberts S. J., Ali N. J., Stradling J. R. Arterial blood pressure responses to graded transient arousal from sleep in normal humans. J Appl Physiol (1985) 1993 Mar;74(3):1123–1130. doi: 10.1152/jappl.1993.74.3.1123. [DOI] [PubMed] [Google Scholar]
- Davies S. W., John L. M., Wedzicha J. A., Lipkin D. P. Overnight studies in severe chronic left heart failure: arrhythmias and oxygen desaturation. Br Heart J. 1991 Feb;65(2):77–83. doi: 10.1136/hrt.65.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg P. R., Sherman L. A., Schectman K., Perez J., Sobel B. E., Jaffe A. S. Fibrinopeptide A: a marker of acute coronary thrombosis. Circulation. 1985 May;71(5):912–918. doi: 10.1161/01.cir.71.5.912. [DOI] [PubMed] [Google Scholar]
- Fitzgerald D. J., Roy L., Catella F., FitzGerald G. A. Platelet activation in unstable coronary disease. N Engl J Med. 1986 Oct 16;315(16):983–989. doi: 10.1056/NEJM198610163151602. [DOI] [PubMed] [Google Scholar]
- Franklin K. A., Nilsson J. B., Sahlin C., Näslund U. Sleep apnoea and nocturnal angina. Lancet. 1995 Apr 29;345(8957):1085–1087. doi: 10.1016/s0140-6736(95)90820-x. [DOI] [PubMed] [Google Scholar]
- Guilleminault C., Robinson A. Sleep-disordered breathing and hypertension: past lessons, future directions. Sleep. 1997 Sep;20(9):806–811. doi: 10.1093/sleep/20.9.806. [DOI] [PubMed] [Google Scholar]
- Hanly P. J., Millar T. W., Steljes D. G., Baert R., Frais M. A., Kryger M. H. Respiration and abnormal sleep in patients with congestive heart failure. Chest. 1989 Sep;96(3):480–488. doi: 10.1378/chest.96.3.480. [DOI] [PubMed] [Google Scholar]
- Huang J., Sopher S. M., Leatham E., Redwood S., Camm A. J., Kaski J. C. Heart rate variability depression in patients with unstable angina. Am Heart J. 1995 Oct;130(4):772–779. doi: 10.1016/0002-8703(95)90076-4. [DOI] [PubMed] [Google Scholar]
- Hung J., Whitford E. G., Parsons R. W., Hillman D. R. Association of sleep apnoea with myocardial infarction in men. Lancet. 1990 Aug 4;336(8710):261–264. doi: 10.1016/0140-6736(90)91799-g. [DOI] [PubMed] [Google Scholar]
- Lofaso F., Verschueren P., Rande J. L., Harf A., Goldenberg F. Prevalence of sleep-disordered breathing in patients on a heart transplant waiting list. Chest. 1994 Dec;106(6):1689–1694. doi: 10.1378/chest.106.6.1689. [DOI] [PubMed] [Google Scholar]
- Marchant B., Stevenson R., Vaishnav S., Wilkinson P., Ranjadayalan K., Timmis A. D. Influence of the autonomic nervous system on circadian patterns of myocardial ischaemia: comparison of stable angina with the early postinfarction period. Br Heart J. 1994 Apr;71(4):329–333. doi: 10.1136/hrt.71.4.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merlini P. A., Bauer K. A., Oltrona L., Ardissino D., Cattaneo M., Belli C., Mannucci P. M., Rosenberg R. D. Persistent activation of coagulation mechanism in unstable angina and myocardial infarction. Circulation. 1994 Jul;90(1):61–68. doi: 10.1161/01.cir.90.1.61. [DOI] [PubMed] [Google Scholar]
- Ohayon M. M., Guilleminault C., Paiva T., Priest R. G., Rapoport D. M., Sagales T., Smirne S., Zulley J. An international study on sleep disorders in the general population: methodological aspects of the use of the Sleep-EVAL system. Sleep. 1997 Dec;20(12):1086–1092. doi: 10.1093/sleep/20.12.1086. [DOI] [PubMed] [Google Scholar]
- Phillips B. A., Berry D. T., Schmitt F. A., Harbison L., Lipke-Molby T. Sleep-disordered breathing in healthy aged persons: two- and three-year follow-up. Sleep. 1994 Aug;17(5):411–415. doi: 10.1093/sleep/17.5.411. [DOI] [PubMed] [Google Scholar]
- Pizarro J., Warner M. M., Ryan M., Mitchell G. S., Bisgard G. E. Intracarotid norepinephrine infusions inhibit ventilation in goats. Respir Physiol. 1992 Dec;90(3):299–310. doi: 10.1016/0034-5687(92)90110-i. [DOI] [PubMed] [Google Scholar]
- Rångemark C., Hedner J. A., Carlson J. T., Gleerup G., Winther K. Platelet function and fibrinolytic activity in hypertensive and normotensive sleep apnea patients. Sleep. 1995 Apr;18(3):188–194. doi: 10.1093/sleep/18.3.188. [DOI] [PubMed] [Google Scholar]
- Saito T., Yoshikawa T., Sakamoto Y., Tanaka K., Inoue T., Ogawa R. Sleep apnea in patients with acute myocardial infarction. Crit Care Med. 1991 Jul;19(7):938–941. doi: 10.1097/00003246-199107000-00019. [DOI] [PubMed] [Google Scholar]
- Schäfer H., Koehler U., Ploch T., Peter J. H. Sleep-related myocardial ischemia and sleep structure in patients with obstructive sleep apnea and coronary heart disease. Chest. 1997 Feb;111(2):387–393. doi: 10.1378/chest.111.2.387. [DOI] [PubMed] [Google Scholar]
- Stradling J., Davies R. J. Sleep apnea and hypertension--what a mess! Sleep. 1997 Sep;20(9):789–793. doi: 10.1093/sleep/20.9.789a. [DOI] [PubMed] [Google Scholar]
- Théroux P., Latour J. G., Léger-Gauthier C., De Lara J. Fibrinopeptide A and platelet factor levels in unstable angina pectoris. Circulation. 1987 Jan;75(1):156–162. doi: 10.1161/01.cir.75.1.156. [DOI] [PubMed] [Google Scholar]
- Vanoli E., Adamson P. B., Ba-Lin, Pinna G. D., Lazzara R., Orr W. C. Heart rate variability during specific sleep stages. A comparison of healthy subjects with patients after myocardial infarction. Circulation. 1995 Apr 1;91(7):1918–1922. doi: 10.1161/01.cir.91.7.1918. [DOI] [PubMed] [Google Scholar]
- White D. P. Central sleep apnea. Med Clin North Am. 1985 Nov;69(6):1205–1219. doi: 10.1016/s0025-7125(16)30983-x. [DOI] [PubMed] [Google Scholar]
- Yamashiro Y., Kryger M. H. Review: sleep in heart failure. Sleep. 1993 Sep;16(6):513–523. doi: 10.1093/sleep/16.6.513. [DOI] [PubMed] [Google Scholar]
- Young T., Palta M., Dempsey J., Skatrud J., Weber S., Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993 Apr 29;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]