Abstract
OBJECTIVE—To explore the use of high resolution magnetic resonance imaging (MRI) of the popliteal artery in defining atheroscelerotic lesions and to monitor the remodelling response to balloon angioplasty. METHODS—Four patients (aged 49-67) with symptomatic discrete popliteal artery stenoses, as demonstrated by conventional angiography, underwent balloon angioplasty. MRI of the diseased vessel was performed before and one week, one month, three months, and six months after therapeutic balloon angioplasty. Cine phase contrast MRI was used to estimate blood flow just proximal to the lesion before and after angioplasty. RESULTS—In all patients the extent of the atherosclerotic plaque could be defined, such that even in segments of vessel which were angiographically "normal", atherosclerotic lesions with cross sectional areas ranging from 49% to 76% of potential lumen area were identified. Following angioplasty, plaque fissuring and local dissection were easily identified and serial changes in lumen diameter, blood flow. and lesion size could be documented. CONCLUSIONS—High resolution MRI can define the extent of atherosclerotic plaque in the peripheral vasculature and demonstrate the changes that occur with remodelling and restenosis following angioplasty. As a safe, reproducible technique MRI is ideal for assessing plaque and monitoring intervention, but further technological developments will be needed if similar or better images are to be achieved in other vascular beds. Keywords: magnetic resonance imaging; atherosclerosis; angioplasty
Full Text
The Full Text of this article is available as a PDF (170.3 KB).
Figure 1 .
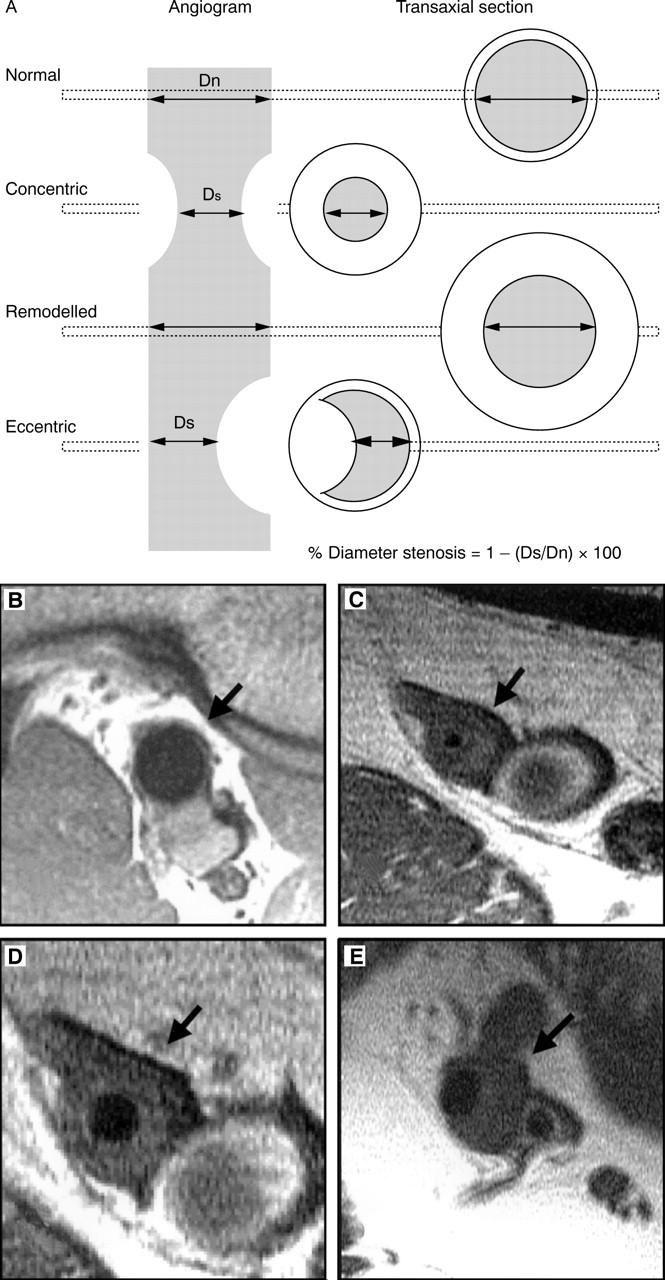
(A) Diagrammatic representation of a conventional angiogram with cross sections through the vessel wall. Cross sections are compared with high resolution magnetic resonance images of the popliteal artery (arrows) taken through a region of normal vessel (B), concentric plaque (C), remodelling (D), and eccentric plaque (E). The vessel adjacent to the artery is the popliteal vein and can be of variable size.
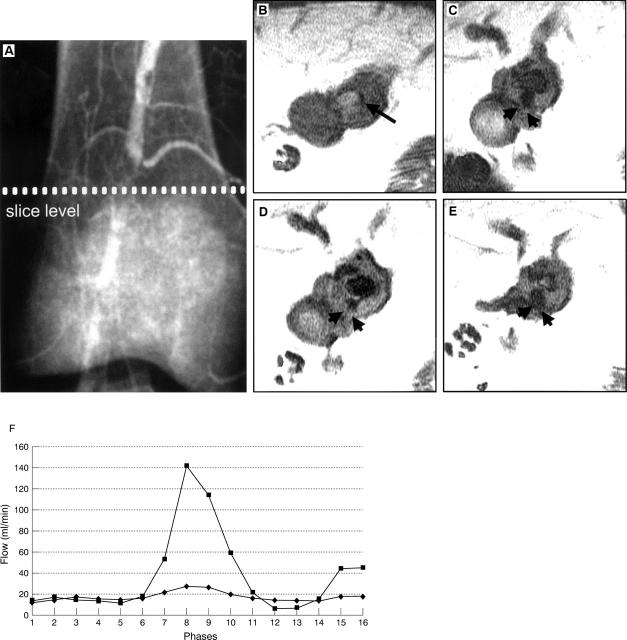
Figure 2 .
(A) Conventional angiogram of the right popliteal artery in patient 1 with a 90% stenosis, who subsequently underwent angioplasty. High resolution magnetic resonance images at the level of the stenosis show cross sections of the artery before angioplasty (B), at one week (C), at one month (D), and at three months (E). The vessel lumen appears black on all images and is shown as a small slit preangioplasty (long arrow). Angioplasty produces extensive fissuring which heals with restenosis but fissuring remains (arrowheads C-E). (F) Flow (ml/min) during 16 phases of the cardiac cycle cranial to the stenosis before angioplasty (♦) and at one week after angioplasty (▪).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brown B. G., Zhao X. Q., Sacco D. E., Albers J. J. Lipid lowering and plaque regression. New insights into prevention of plaque disruption and clinical events in coronary disease. Circulation. 1993 Jun;87(6):1781–1791. doi: 10.1161/01.cir.87.6.1781. [DOI] [PubMed] [Google Scholar]
- Davies M. J., Richardson P. D., Woolf N., Katz D. R., Mann J. Risk of thrombosis in human atherosclerotic plaques: role of extracellular lipid, macrophage, and smooth muscle cell content. Br Heart J. 1993 May;69(5):377–381. doi: 10.1136/hrt.69.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glagov S., Weisenberg E., Zarins C. K., Stankunavicius R., Kolettis G. J. Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med. 1987 May 28;316(22):1371–1375. doi: 10.1056/NEJM198705283162204. [DOI] [PubMed] [Google Scholar]
- Hackett D., Davies G., Maseri A. Pre-existing coronary stenoses in patients with first myocardial infarction are not necessarily severe. Eur Heart J. 1988 Dec;9(12):1317–1323. doi: 10.1093/oxfordjournals.eurheartj.a062449. [DOI] [PubMed] [Google Scholar]
- Libby P. Molecular bases of the acute coronary syndromes. Circulation. 1995 Jun 1;91(11):2844–2850. doi: 10.1161/01.cir.91.11.2844. [DOI] [PubMed] [Google Scholar]
- Skinner M. P., Yuan C., Mitsumori L., Hayes C. E., Raines E. W., Nelson J. A., Ross R. Serial magnetic resonance imaging of experimental atherosclerosis detects lesion fine structure, progression and complications in vivo. Nat Med. 1995 Jan;1(1):69–73. doi: 10.1038/nm0195-69. [DOI] [PubMed] [Google Scholar]
- Toussaint J. F., LaMuraglia G. M., Southern J. F., Fuster V., Kantor H. L. Magnetic resonance images lipid, fibrous, calcified, hemorrhagic, and thrombotic components of human atherosclerosis in vivo. Circulation. 1996 Sep 1;94(5):932–938. doi: 10.1161/01.cir.94.5.932. [DOI] [PubMed] [Google Scholar]
- Weissberg P. L., Clesham G. J., Bennett M. R. Is vascular smooth muscle cell proliferation beneficial? Lancet. 1996 Feb 3;347(8997):305–307. doi: 10.1016/s0140-6736(96)90472-9. [DOI] [PubMed] [Google Scholar]