Abstract
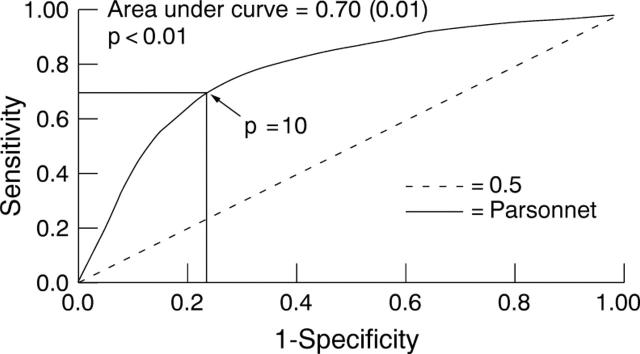
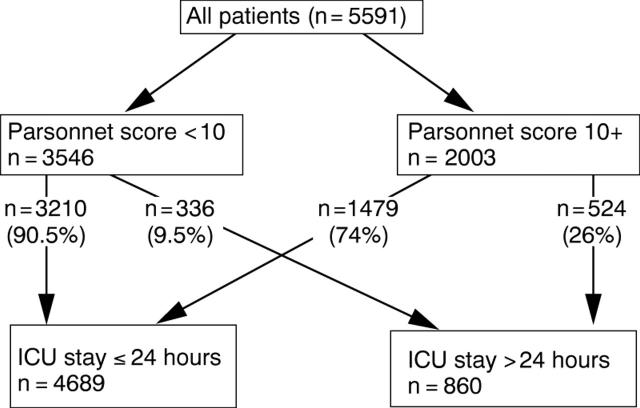
OBJECTIVE—To investigate the value of the Parsonnet score (PS) in identifying preoperatively patients that are likely to spend < 24 hours on the intensive care unit (ICU) following cardiac surgery. METHOD—Prospectively collected data on 5591 patients were analysed. PS, mortality, the length of stay on the ICU (ICU-LOS), number of patients with clinical evidence of stroke, need for haemofiltration, resternotomy for bleeding, tracheostomy, and use of intra-aortic balloon pump were documented as outcomes. A receiver operating characteristic (ROC) curve constructed using PS as a predictor of ICU stay < 24 hours identified a PS of 10 as the best cut off point that would predict ICU-LOS < 24 hours. The patients were therefore stratified by PS into two groups, those with a PS of 0 to 9 (PS 0-9) and those with a PS of 10 and above (PS 10+). RESULTS—The ROC curve constructed using PS as a predictor of ICU stay < 24 hours had an area under the curve of 0.70 (0.01). The maximum efficiency of the test was at a sensitivity of 0.68. This corresponded to PS 10. The positive predictive value of the test at this score was 90.5%. Patients with PS 0-9 had a mean ICU stay of 1.49 days, while patients with PS 10+ had a mean ICU stay of 2.89 days (p = 0.01). The risk of stroke, use of intra-aortic balloon pump, requirement for haemofiltration, need for tracheostomy, and risk of resternotomy for bleeding were each significantly less in patients with PS 0-9 versus those with a score of PS 10+ (p < 0.01 in all cases). The risk of a single complication was 4.7% (PS 0-9) v 15.2% (PS 10+) (p < 0.01). CONCLUSION—PS is an impartial and objective method of predicting postoperative complications and ICU stay < 24 hours. This is of value in selecting a cohort of patients likely to maintain a smooth flow of patients through the cardiothoracic unit when resources are limited to a few free ICU beds. Keywords: Parsonnet score; intensive care; length of hospital stay; rationing
Full Text
The Full Text of this article is available as a PDF (111.2 KB).
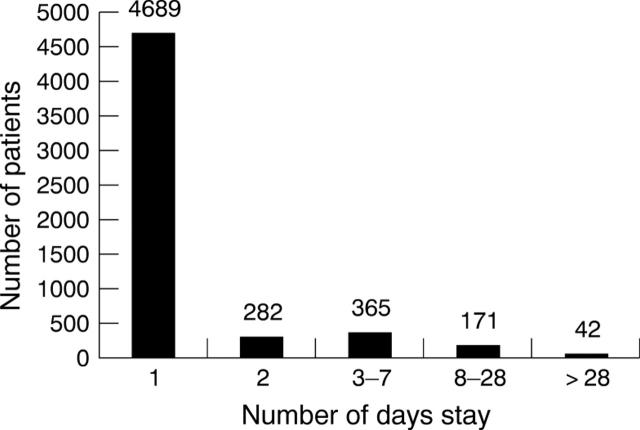
Figure 1 .
ICU-LOS versus number of patients (n = 5549).
Figure 2 .
ROC for PS as a predictor of ICU-LOS < 24 hours. Sensitivity of 0.68 and specificity of 0.77 when PS is 10.
Figure 3 .
Flow chart of patients passing through ICU using PS as a sieve.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blankenhorn D. H., Kramsch D. M. Reversal of atherosis and sclerosis. The two components of atherosclerosis. Circulation. 1989 Jan;79(1):1–7. doi: 10.1161/01.cir.79.1.1. [DOI] [PubMed] [Google Scholar]
- Collinson P. Of bombers, radiologists, and cardiologists: time to ROC. Heart. 1998 Sep;80(3):215–217. doi: 10.1136/hrt.80.3.215. [DOI] [PubMed] [Google Scholar]
- Hadorn D. C., Holmes A. C. The New Zealand priority criteria project. Part 2: Coronary artery bypass graft surgery. BMJ. 1997 Jan 11;314(7074):135–138. doi: 10.1136/bmj.314.7074.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus M. L., Chilian W. M., Kanatsuka H., Dellsperger K. C., Eastham C. L., Lamping K. G. Understanding the coronary circulation through studies at the microvascular level. Circulation. 1990 Jul;82(1):1–7. doi: 10.1161/01.cir.82.1.1. [DOI] [PubMed] [Google Scholar]
- Mounsey J. P., Griffith M. J., Heaviside D. W., Brown A. H., Reid D. S. Determinants of the length of stay in intensive care and in hospital after coronary artery surgery. Br Heart J. 1995 Jan;73(1):92–98. doi: 10.1136/hrt.73.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor C. D., Baigrie R. S., Goldman B. S., Basinski A. Assessment of priority for coronary revascularisation procedures. Revascularisation Panel and Consensus Methods Group. Lancet. 1990 May 5;335(8697):1070–1073. doi: 10.1016/0140-6736(90)92640-4. [DOI] [PubMed] [Google Scholar]
- Tu J. V., Jaglal S. B., Naylor C. D. Multicenter validation of a risk index for mortality, intensive care unit stay, and overall hospital length of stay after cardiac surgery. Steering Committee of the Provincial Adult Cardiac Care Network of Ontario. Circulation. 1995 Feb 1;91(3):677–684. doi: 10.1161/01.cir.91.3.677. [DOI] [PubMed] [Google Scholar]
- Tu J. V., Mazer C. D. Can clinicians predict ICU length of stay following cardiac surgery? Can J Anaesth. 1996 Aug;43(8):789–794. doi: 10.1007/BF03013030. [DOI] [PubMed] [Google Scholar]
- Unsworth-White M. J., Herriot A., Valencia O., Poloniecki J., Smith E. E., Murday A. J., Parker D. J., Treasure T. Resternotomy for bleeding after cardiac operation: a marker for increased morbidity and mortality. Ann Thorac Surg. 1995 Mar;59(3):664–667. doi: 10.1016/0003-4975(94)00995-3. [DOI] [PubMed] [Google Scholar]
- Weintraub W. S., Jones E. L., Craver J., Guyton R., Cohen C. Determinants of prolonged length of hospital stay after coronary bypass surgery. Circulation. 1989 Aug;80(2):276–284. doi: 10.1161/01.cir.80.2.276. [DOI] [PubMed] [Google Scholar]