Abstract
OBJECTIVE—To determine the prevalence of the Brugada sign (right bundle branch block with ST elevation in V1-V3) in idiopathic ventricular fibrillation and in an age matched healthy population. DESIGN—ECGs from 39 consecutive patients with idiopathic ventricular fibrillation and 592 healthy controls were reviewed. They were classified as definite, questionable, and no Brugada sign (according to predetermined criteria) by four investigators blinded to the subjects' status. RESULTS—Eight patients (21%) with idiopathic ventricular fibrillation but none of the 592 controls had a definite Brugada sign (p < 0.005). Thus the estimated 95% confidence limits for the prevalence of a definite Brugada sign among healthy controls was less than 0.5%. A questionable Brugada sign was seen in two patients with idiopathic ventricular fibrillation (5%) but also in five controls (1%) (p < 0.05). Normal ECGs were found following resuscitation and during long term follow up in 31 patients with idiopathic ventricular fibrillation (79%). Patients with idiopathic ventricular fibrillation and a normal ECG and those with the Brugada syndrome were of similar age and had similar spontaneous and inducible arrhythmias. However, the two groups differed in terms of sex, family history, and the incidence of sleep related ventricular fibrillation. CONCLUSIONS—A definite Brugada sign is a specific marker of arrhythmic risk. However, less than obvious ECG abnormalities have little diagnostic value, as a "questionable" Brugada sign was observed in 1% of healthy controls. In this series of consecutive patients with idiopathic ventricular fibrillation, most had normal ECGs. Keywords: sudden death; cardiac arrest; ventricular fibrillation; Brugada syndrome
Full Text
The Full Text of this article is available as a PDF (219.9 KB).
Figure 1 .
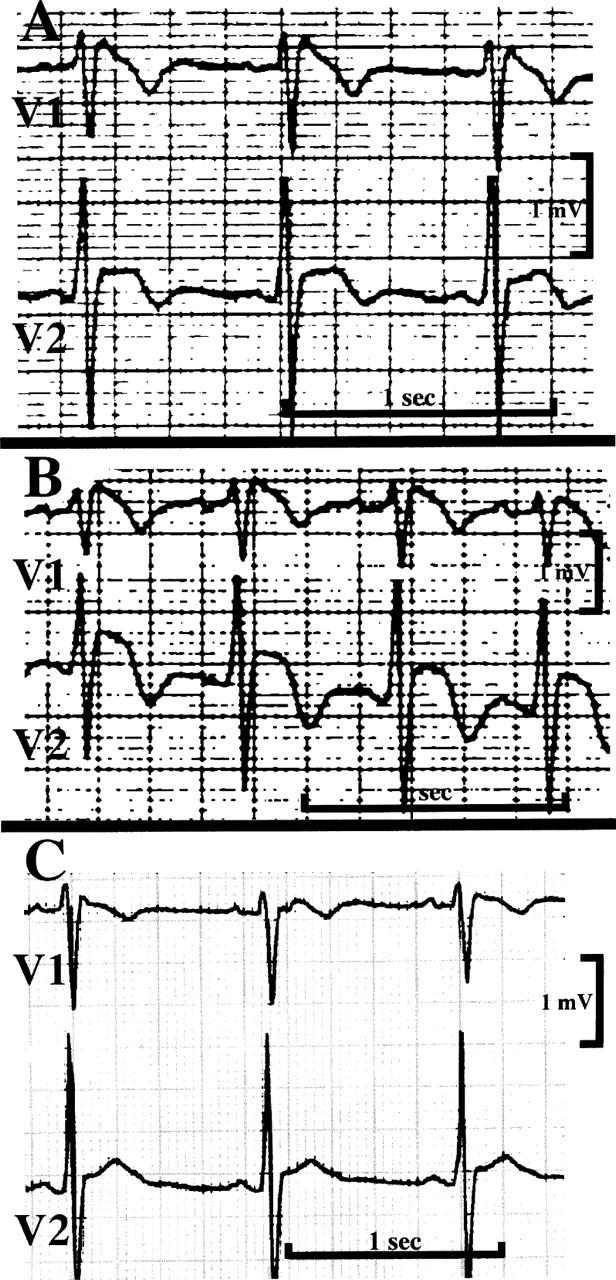
Three ECGs (leads V1-V2) of a patient with idiopathic ventricular fibrillation. The top and middle traces were graded as "definite Brugada sign". The bottom trace (recorded three years after diagnosis) was graded as "questionable Brugada sign". The middle and bottom traces were recorded during treatment with quinidine.
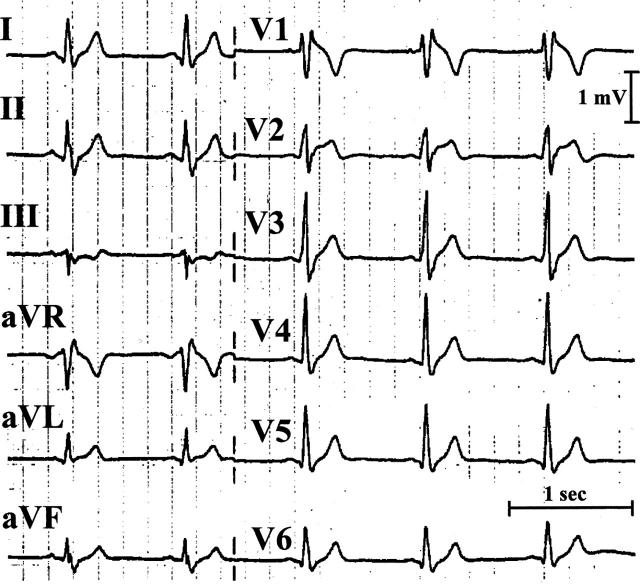
Figure 2 .
ECG of a patient with idiopathic ventricular fibrillation showing a "definite" Brugada sign. RsR' with obvious ST elevation is shown. Additional ECGs of this patient have been published previously.11
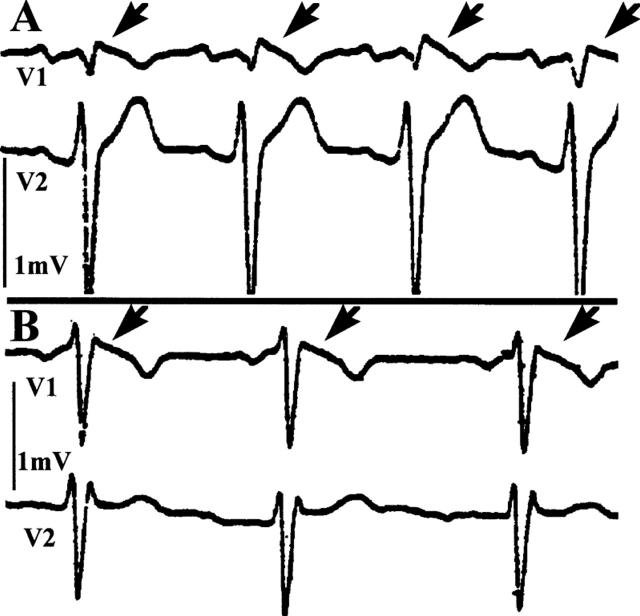
Figure 3 .
ECGs (leads V1-V2) of two patients with "questionable" Brugada sign. RsR' with minor ST elevation is shown (arrows). Both patients belong to the control group.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- APONTE G. E. The enigma of "bangungut". Ann Intern Med. 1960 Jun;52:1258–1263. doi: 10.7326/0003-4819-52-6-1258. [DOI] [PubMed] [Google Scholar]
- Alings M., Wilde A. "Brugada" syndrome: clinical data and suggested pathophysiological mechanism. Circulation. 1999 Feb 9;99(5):666–673. doi: 10.1161/01.cir.99.5.666. [DOI] [PubMed] [Google Scholar]
- Antzelevitch C. The Brugada syndrome. J Cardiovasc Electrophysiol. 1998 May;9(5):513–516. doi: 10.1111/j.1540-8167.1998.tb01844.x. [DOI] [PubMed] [Google Scholar]
- Atarashi H., Ogawa S., Harumi K., Hayakawa H., Sugimoto T., Okada R., Murayama M., Toyama J. Characteristics of patients with right bundle branch block and ST-segment elevation in right precordial leads. Idiopathic Ventricular Fibrillation Investigators. Am J Cardiol. 1996 Sep 1;78(5):581–583. doi: 10.1016/s0002-9149(96)00360-8. [DOI] [PubMed] [Google Scholar]
- Baron R. C., Thacker S. B., Gorelkin L., Vernon A. A., Taylor W. R., Choi K. Sudden death among Southeast Asian refugees. An unexplained nocturnal phenomenon. JAMA. 1983 Dec 2;250(21):2947–2951. [PubMed] [Google Scholar]
- Belhassen B., Pelleg A., Miller H. I., Laniado S. Serial electrophysiological studies in a young patient with recurrent ventricular fibrillation. Pacing Clin Electrophysiol. 1981 Jan;4(1):92–99. doi: 10.1111/j.1540-8159.1981.tb03680.x. [DOI] [PubMed] [Google Scholar]
- Belhassen B., Shapira I., Shoshani D., Paredes A., Miller H., Laniado S. Idiopathic ventricular fibrillation: inducibility and beneficial effects of class I antiarrhythmic agents. Circulation. 1987 Apr;75(4):809–816. doi: 10.1161/01.cir.75.4.809. [DOI] [PubMed] [Google Scholar]
- Belhassen B., Viskin S., Fish R., Glick A., Setbon I., Eldar M. Effects of electrophysiologic-guided therapy with Class IA antiarrhythmic drugs on the long-term outcome of patients with idiopathic ventricular fibrillation with or without the Brugada syndrome. J Cardiovasc Electrophysiol. 1999 Oct;10(10):1301–1312. doi: 10.1111/j.1540-8167.1999.tb00183.x. [DOI] [PubMed] [Google Scholar]
- Belhassen B., Viskin S. Idiopathic ventricular tachycardia and fibrillation. J Cardiovasc Electrophysiol. 1993 Jun;4(3):356–368. doi: 10.1111/j.1540-8167.1993.tb01236.x. [DOI] [PubMed] [Google Scholar]
- Brugada J., Brugada P. What to do in patients with no structural heart disease and sudden arrhythmic death? Am J Cardiol. 1996 Sep 12;78(5A):69–75. doi: 10.1016/s0002-9149(96)00505-x. [DOI] [PubMed] [Google Scholar]
- Brugada J., Brugada R., Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998 Feb 10;97(5):457–460. doi: 10.1161/01.cir.97.5.457. [DOI] [PubMed] [Google Scholar]
- Brugada P., Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992 Nov 15;20(6):1391–1396. doi: 10.1016/0735-1097(92)90253-j. [DOI] [PubMed] [Google Scholar]
- Brugada R., Brugada J., Antzelevitch C., Kirsch G. E., Potenza D., Towbin J. A., Brugada P. Sodium channel blockers identify risk for sudden death in patients with ST-segment elevation and right bundle branch block but structurally normal hearts. Circulation. 2000 Feb 8;101(5):510–515. doi: 10.1161/01.cir.101.5.510. [DOI] [PubMed] [Google Scholar]
- Chen Q., Kirsch G. E., Zhang D., Brugada R., Brugada J., Brugada P., Potenza D., Moya A., Borggrefe M., Breithardt G. Genetic basis and molecular mechanism for idiopathic ventricular fibrillation. Nature. 1998 Mar 19;392(6673):293–296. doi: 10.1038/32675. [DOI] [PubMed] [Google Scholar]
- Corrado D., Nava A., Buja G., Martini B., Fasoli G., Oselladore L., Turrini P., Thiene G. Familial cardiomyopathy underlies syndrome of right bundle branch block, ST segment elevation and sudden death. J Am Coll Cardiol. 1996 Feb;27(2):443–448. doi: 10.1016/0735-1097(95)00485-8. [DOI] [PubMed] [Google Scholar]
- Fujiki A., Usui M., Nagasawa H., Mizumaki K., Hayashi H., Inoue H. ST segment elevation in the right precordial leads induced with class IC antiarrhythmic drugs: insight into the mechanism of Brugada syndrome. J Cardiovasc Electrophysiol. 1999 Feb;10(2):214–218. doi: 10.1111/j.1540-8167.1999.tb00662.x. [DOI] [PubMed] [Google Scholar]
- Gussak I., Antzelevitch C., Bjerregaard P., Towbin J. A., Chaitman B. R. The Brugada syndrome: clinical, electrophysiologic and genetic aspects. J Am Coll Cardiol. 1999 Jan;33(1):5–15. doi: 10.1016/s0735-1097(98)00528-2. [DOI] [PubMed] [Google Scholar]
- Gussak I., Bjerregaard P., Egan T. M., Chaitman B. R. ECG phenomenon called the J wave. History, pathophysiology, and clinical significance. J Electrocardiol. 1995 Jan;28(1):49–58. doi: 10.1016/s0022-0736(05)80007-x. [DOI] [PubMed] [Google Scholar]
- Kasanuki H., Ohnishi S., Ohtuka M., Matsuda N., Nirei T., Isogai R., Shoda M., Toyoshima Y., Hosoda S. Idiopathic ventricular fibrillation induced with vagal activity in patients without obvious heart disease. Circulation. 1997 May 6;95(9):2277–2285. doi: 10.1161/01.cir.95.9.2277. [DOI] [PubMed] [Google Scholar]
- Lemery R., Brugada P., Della Bella P., Dugernier T., Wellens H. J. Ventricular fibrillation in six adults without overt heart disease. J Am Coll Cardiol. 1989 Mar 15;13(4):911–916. doi: 10.1016/0735-1097(89)90235-0. [DOI] [PubMed] [Google Scholar]
- Martini B., Nava A., Thiene G., Buja G. F., Canciani B., Scognamiglio R., Daliento L., Dalla Volta S. Ventricular fibrillation without apparent heart disease: description of six cases. Am Heart J. 1989 Dec;118(6):1203–1209. doi: 10.1016/0002-8703(89)90011-2. [DOI] [PubMed] [Google Scholar]
- Miyazaki T., Mitamura H., Miyoshi S., Soejima K., Aizawa Y., Ogawa S. Autonomic and antiarrhythmic drug modulation of ST segment elevation in patients with Brugada syndrome. J Am Coll Cardiol. 1996 Apr;27(5):1061–1070. doi: 10.1016/0735-1097(95)00613-3. [DOI] [PubMed] [Google Scholar]
- Nademanee K., Veerakul G., Nimmannit S., Chaowakul V., Bhuripanyo K., Likittanasombat K., Tunsanga K., Kuasirikul S., Malasit P., Tansupasawadikul S. Arrhythmogenic marker for the sudden unexplained death syndrome in Thai men. Circulation. 1997 Oct 21;96(8):2595–2600. doi: 10.1161/01.cir.96.8.2595. [DOI] [PubMed] [Google Scholar]
- Roden D. M., Wilde A. A. Drug-induced J point elevation: a marker for genetic risk of sudden death or ECG curiosity? J Cardiovasc Electrophysiol. 1999 Feb;10(2):219–223. doi: 10.1111/j.1540-8167.1999.tb00663.x. [DOI] [PubMed] [Google Scholar]
- Scheinman M. M. Is the Brugada syndrome a distinct clinical entity? J Cardiovasc Electrophysiol. 1997 Mar;8(3):332–336. doi: 10.1111/j.1540-8167.1997.tb00797.x. [DOI] [PubMed] [Google Scholar]
- Viskin S., Belhassen B. Clinical problem-solving. When you only live twice. N Engl J Med. 1995 May 4;332(18):1221–1225. doi: 10.1056/NEJM199505043321809. [DOI] [PubMed] [Google Scholar]
- Viskin S., Belhassen B. Idiopathic ventricular fibrillation. Am Heart J. 1990 Sep;120(3):661–671. doi: 10.1016/0002-8703(90)90025-s. [DOI] [PubMed] [Google Scholar]
- Viskin S., Belhassen B. Polymorphic ventricular tachyarrhythmias in the absence of organic heart disease: classification, differential diagnosis, and implications for therapy. Prog Cardiovasc Dis. 1998 Jul-Aug;41(1):17–34. doi: 10.1016/s0033-0620(98)80020-0. [DOI] [PubMed] [Google Scholar]
- Viskin S., Lesh M. D., Eldar M., Fish R., Setbon I., Laniado S., Belhassen B. Mode of onset of malignant ventricular arrhythmias in idiopathic ventricular fibrillation. J Cardiovasc Electrophysiol. 1997 Oct;8(10):1115–1120. doi: 10.1111/j.1540-8167.1997.tb00997.x. [DOI] [PubMed] [Google Scholar]
- Wever E. F., Hauer R. N., Oomen A., Peters R. H., Bakker P. F., Robles de Medina E. O. Unfavorable outcome in patients with primary electrical disease who survived an episode of ventricular fibrillation. Circulation. 1993 Sep;88(3):1021–1029. doi: 10.1161/01.cir.88.3.1021. [DOI] [PubMed] [Google Scholar]
- Yan G. X., Antzelevitch C. Cellular basis for the electrocardiographic J wave. Circulation. 1996 Jan 15;93(2):372–379. doi: 10.1161/01.cir.93.2.372. [DOI] [PubMed] [Google Scholar]