Abstract
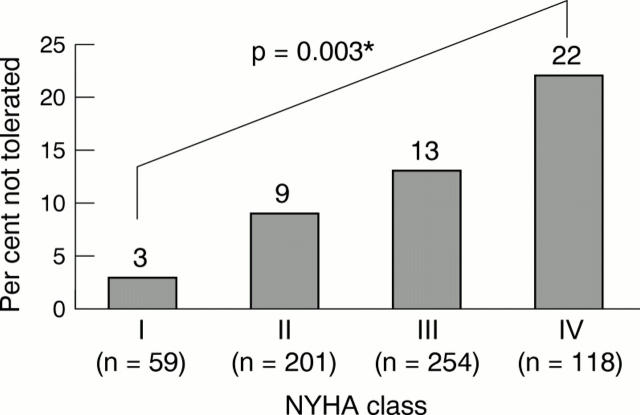
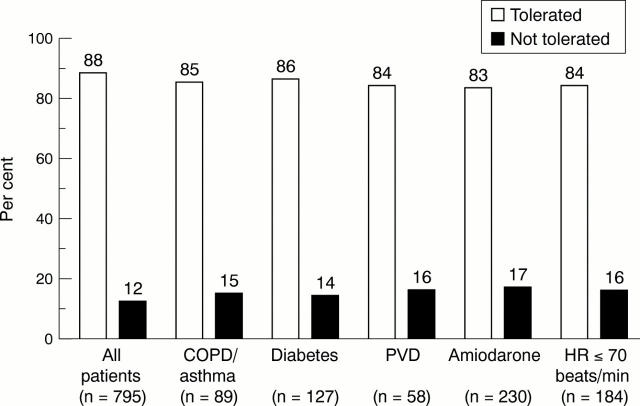
OBJECTIVE—To determine baseline predictors of tolerance to the α/β blocker carvedilol in everyday clinical practice. DESIGN—Retrospective analysis of tolerance to carvedilol in patients with chronic heart failure. Tolerance was defined as currently on carvedilol or on it at the time of death or heart transplantation. To meet the criteria for tolerance, carvedilol had to be prescribed at a stable dose for ⩾ 3 months. SETTING—Everyday clinical practice, comprising both hospital specialist practice and private practice. Tolerance was assessed in all patients prescribed carvedilol for chronic heart failure in those practices. PATIENTS—808 consecutive patients in both hospital specialist (611 patients) and private practice (197 patients). MAIN OUTCOME MEASURES—Baseline predictors of tolerance assessed by proportional hazards analysis. Both univariate and multivariate analyses were performed. RESULTS—Within the entire cohort of 808 patients, 95 had stopped carvedilol, 606 were currently receiving the drug, 50 had died, and 44 had received a heart transplant. Overall, 88% of patients tolerated carvedilol (87% in the hospital specialist group, 92% in the private practitioner group). Factors that indicated impaired tolerance by univariate analysis were increased age in years (hazard ratio 1.01, 95% confidence interval (CI) 1.0 to 1.3), low diastolic blood pressure (hazard ratio 1.04, 95% CI 1.02 to 1.08), and raised plasma urea concentration (hazard ratio 1.04, 95% CI 1.02 to 1.05). New York Heart Association (NYHA) class was also a marker of tolerance (proportion not tolerated: 3% class I; 9% class II; 13% class III, 22% class IV). By multivariate analysis, no single baseline variable was an independent marker of inability to tolerate carvedilol. Tolerance was also assessed in relation to traditional precautions or relative contraindications to β blockade. Tolerance in these subgroups was: chronic obstructive airways disease/asthma 85% (89 patients), diabetes 86% (127 patients), peripheral vascular disease 84% (58 patients), concomitant amiodarone treatment 83% (230 patients), and heart rate < 70 beats/min 84% (184 patients). CONCLUSIONS—β Blocker treatment was well tolerated in everyday clinical practice, including non-hospital-based private practice. There was no single predictor of poor tolerance on multivariate analysis, although there was a clear association with NYHA class as well as age, diastolic blood pressure, and plasma urea on univariate analysis. Carvedilol was tolerated well among selected patients with traditional contraindications to β blockade in this situation. Keywords: chronic heart failure; β blockade; carvedilol
Full Text
The Full Text of this article is available as a PDF (147.8 KB).
Figure 1 .
Per cent of patients unable to tolerate carvedilol treatment, grouped according to New York Heart Association (NYHA) functional class. Data analysed by proportional hazards analysis on time to discontinuation (intolerance), with NYHA class fitted using indicator variables.*Proportional hazards analysis on time to discontinuation (intolerance) with NYHA class fitted using indicator variables.
Figure 2 .
Per cent of patients able to tolerate carvedilol treatment, grouped according to traditional contraindications and precautions in prescribing a β blocker. COPD, chronic obstructive pulmonary disease; HR, heart rate; PVD, peripheral vascular disease.
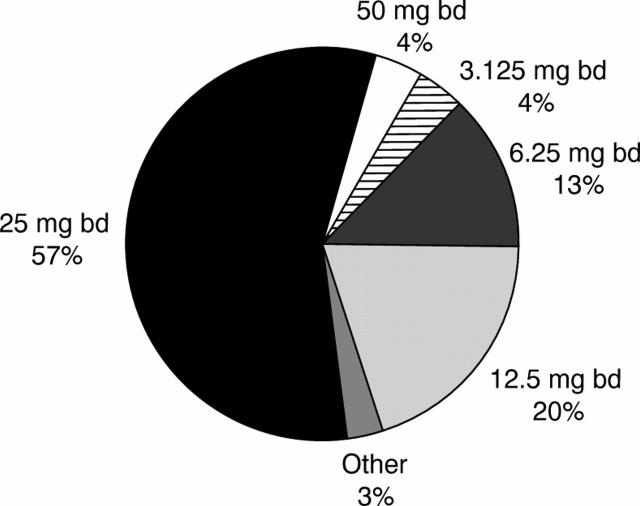
Figure 3 .
First stable dose of carvedilol achieved in study patients.
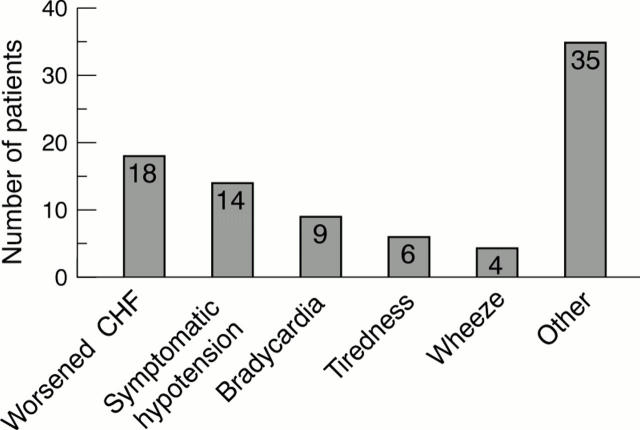
Figure 4 .
Reason for discontinuation of carvedilol among study patients. CHF, chronic heart failure.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bristow M. R., Gilbert E. M., Abraham W. T., Adams K. F., Fowler M. B., Hershberger R. E., Kubo S. H., Narahara K. A., Ingersoll H., Krueger S. Carvedilol produces dose-related improvements in left ventricular function and survival in subjects with chronic heart failure. MOCHA Investigators. Circulation. 1996 Dec 1;94(11):2807–2816. doi: 10.1161/01.cir.94.11.2807. [DOI] [PubMed] [Google Scholar]
- Packer M., Bristow M. R., Cohn J. N., Colucci W. S., Fowler M. B., Gilbert E. M., Shusterman N. H. The effect of carvedilol on morbidity and mortality in patients with chronic heart failure. U.S. Carvedilol Heart Failure Study Group. N Engl J Med. 1996 May 23;334(21):1349–1355. doi: 10.1056/NEJM199605233342101. [DOI] [PubMed] [Google Scholar]
- Ruffolo R. R., Jr, Gellai M., Hieble J. P., Willette R. N., Nichols A. J. The pharmacology of carvedilol. Eur J Clin Pharmacol. 1990;38 (Suppl 2):S82–S88. doi: 10.1007/BF01409471. [DOI] [PubMed] [Google Scholar]