Abstract
OBJECTIVE—To create a risk model for predicting major adverse complicating events of percutaneous transluminal coronary angioplasty (PTCA), and to test the accuracy of the model on a prospective cohort of patients SETTING—Tertiary cardiac centre METHODS—Available software can predict probabilities of events using Bayes's theorem. To establish the accuracy of these predictive tools, a Bayes table was created to evaluate major adverse complicating events (MACE)—death, emergency coronary artery bypass grafting (CABG), or Q wave infarct occurring during the in-patient episode—on the first 1500 patients in the department PTCA database (development group); the predictive value of this model was then tested with the subsequent 1000 patients (evaluation group). The following probabilities were assessed to determine their association with MACE: age, sex, left ventricular function, American Heart Association lesion morphology classification, cardiogenic shock, previous CABG, diabetes, hypertension, multivessel PTCA. MAIN OUTCOME MEASURES—To establish the discriminatory ability of the predictive index, calibration plots and receiver operating characteristic (ROC) curves were obtained to compare the development and evaluation groups. RESULTS—The ROC curve plotted to determine the discriminatory value of the Bayesian table created from the development group (n = 1500) in predicting MACE in the evaluation group (n = 1000) showed a moderately predictive area under the curve of 0.76 (SEM 0.07). This predictive accuracy was confirmed with separately constructed calibration plots. CONCLUSIONS—Accurate predictions of MACE can be identified in populations undergoing percutaneous intervention. The database used allows operators to obtain consent from patients appropriately from their own experience rather than from other published data. If a national PTCA database existed along similar lines, individual operators and interventional centres could compare themselves with nationally available data. Keywords: percutaneous transluminal coronary angioplasty; Bayesian risk; outcome prediction
Full Text
The Full Text of this article is available as a PDF (121.9 KB).
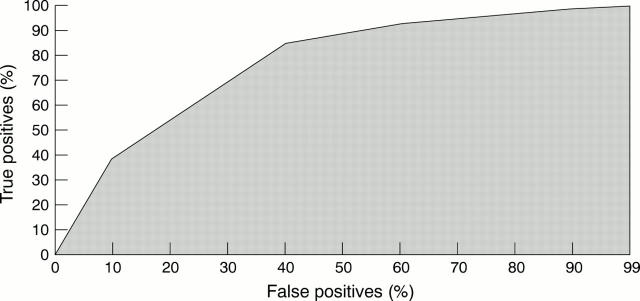
Figure 1 .
Receiver operating characteristic (ROC) curve plotted to determine the discriminatory value of the Bayesian table created from the development group (n = 1500) in predicting major adverse cardiac events (MACE) in the evaluation group (n = 1000). The area under the ROC curve is a moderately predictive 0.76 (SEM 0.07).
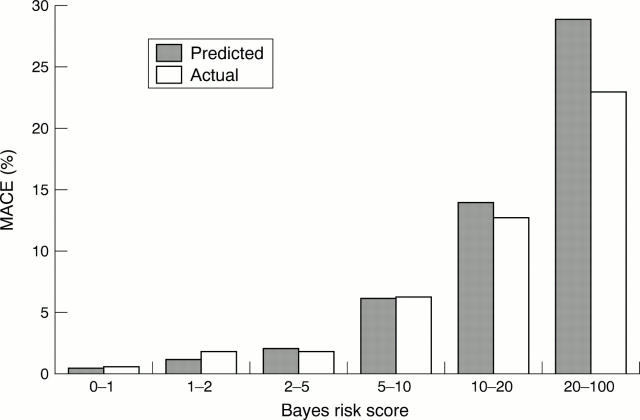
Figure 2 .
Bayes's risk groups were calculated from the development group and plotted against the incidence of major adverse cardiac events (MACE). These were compared against the actual event rate of MACE using the same risk groups created from the evaluation group. This calibration plot shows an accurate assessment of risk in the low risk groups, but it was less accurate for patients with greater risk.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bredlau C. E., Roubin G. S., Leimgruber P. P., Douglas J. S., Jr, King S. B., 3rd, Gruentzig A. R. In-hospital morbidity and mortality in patients undergoing elective coronary angioplasty. Circulation. 1985 Nov;72(5):1044–1052. doi: 10.1161/01.cir.72.5.1044. [DOI] [PubMed] [Google Scholar]
- Edwards F. H., Graeber G. M. The theorem of Bayes as a clinical research tool. Surg Gynecol Obstet. 1987 Aug;165(2):127–129. [PubMed] [Google Scholar]
- Holmes D. R., Jr, Holubkov R., Vlietstra R. E., Kelsey S. F., Reeder G. S., Dorros G., Williams D. O., Cowley M. J., Faxon D. P., Kent K. M. Comparison of complications during percutaneous transluminal coronary angioplasty from 1977 to 1981 and from 1985 to 1986: the National Heart, Lung, and Blood Institute Percutaneous Transluminal Coronary Angioplasty Registry. J Am Coll Cardiol. 1988 Nov;12(5):1149–1155. doi: 10.1016/0735-1097(88)92593-4. [DOI] [PubMed] [Google Scholar]
- Kimmel S. E., Berlin J. A., Strom B. L., Laskey W. K. Development and validation of simplified predictive index for major complications in contemporary percutaneous transluminal coronary angioplasty practice. The Registry Committee of the Society for Cardiac Angiography and Interventions. J Am Coll Cardiol. 1995 Oct;26(4):931–938. doi: 10.1016/0735-1097(95)00294-4. [DOI] [PubMed] [Google Scholar]
- Laskey W., Boyle J., Johnson L. W. Multivariable model for prediction of risk of significant complication during diagnostic cardiac catheterization. The Registry Committee of the Society for Cardiac Angiography & Interventions. Cathet Cardiovasc Diagn. 1993 Nov;30(3):185–190. doi: 10.1002/ccd.1810300302. [DOI] [PubMed] [Google Scholar]
- Wasson J. H., Sox H. C., Neff R. K., Goldman L. Clinical prediction rules. Applications and methodological standards. N Engl J Med. 1985 Sep 26;313(13):793–799. doi: 10.1056/NEJM198509263131306. [DOI] [PubMed] [Google Scholar]