Abstract
OBJECTIVE—To compare the accuracy and feasibility of harmonic power Doppler and digitally subtracted colour coded grey scale imaging for the assessment of perfusion defect severity by single photon emission computed tomography (SPECT) in an unselected group of patients. DESIGN—Cohort study. SETTING—Regional cardiothoracic unit. PATIENTS—49 patients (mean (SD) age 61 (11) years; 27 women, 22 men) with known or suspected coronary artery disease were studied with simultaneous myocardial contrast echo (MCE) and SPECT after standard dipyridamole stress. MAIN OUTCOME MEASURES—Regional myocardial perfusion by SPECT, performed with 99mTc tetrafosmin, scored qualitatively and also quantitated as per cent maximum activity. RESULTS—Normal perfusion was identified by SPECT in 225 of 270 segments (83%). Contrast echo images were interpretable in 92% of patients. The proportion of normal MCE by grey scale, subtracted, and power Doppler techniques were respectively 76%, 74%, and 88% (p < 0.05) at > 80% of maximum counts, compared with 65%, 69%, and 61% at < 60% of maximum counts. For each technique, specificity was lowest in the lateral wall, although power Doppler was the least affected. Grey scale and subtraction techniques were least accurate in the septal wall, but power Doppler showed particular problems in the apex. On a per patient analysis, the sensitivity was 67%, 75%, and 83% for detection of coronary artery disease using grey scale, colour coded, and power Doppler, respectively, with a significant difference between power Doppler and grey scale only (p < 0.05). Specificity was also the highest for power Doppler, at 55%, but not significantly different from subtracted colour coded images. CONCLUSIONS—Myocardial contrast echo using harmonic power Doppler has greater accuracy than with grey scale imaging and digital subtraction. However, power Doppler appears to be less sensitive for mild perfusion defects. Keywords: myocardial contrast echo; SPECT; coronary artery disease; dipyridamole stress
Full Text
The Full Text of this article is available as a PDF (254.0 KB).
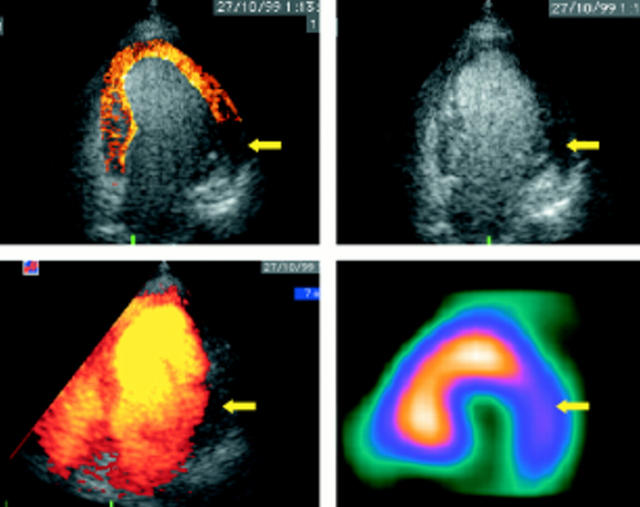
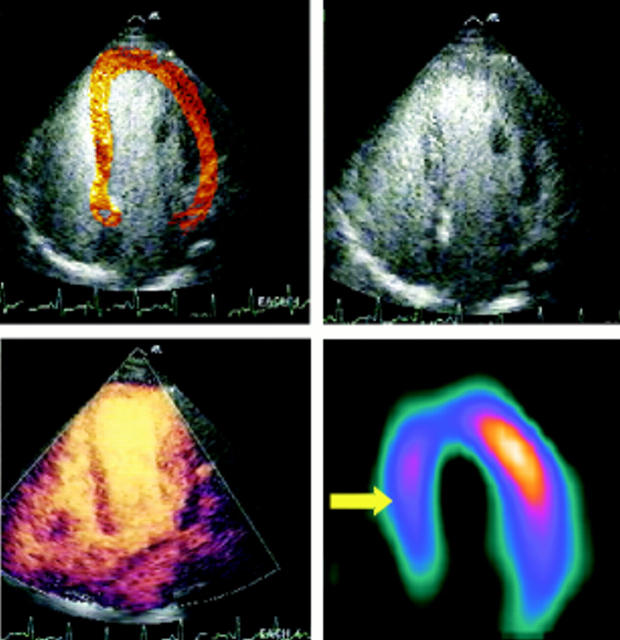
Figure 1 .
Concordant diagnosis with multiple image processing strategies. The lateral perfusion defect by single photon emission computed tomography (SPECT) is matched by lateral defects on grey scale, colour coded, and power Doppler images (arrows).
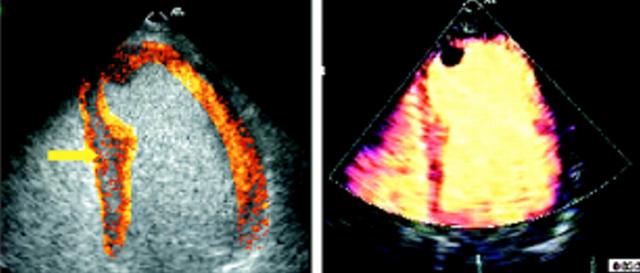
Figure 2 .
False positive contrast perfusion defect caused by a "septal stripe" (arrow). This appearance is caused by inhomogeneity of the resting image and reflects the disadvantage of simple subtraction.
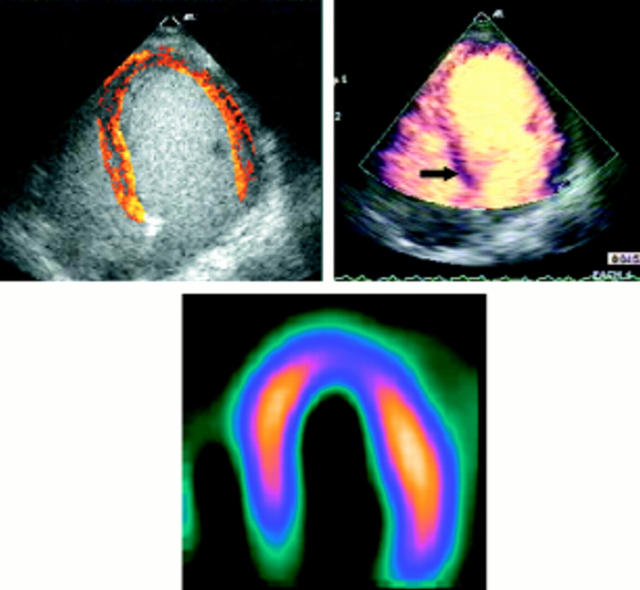
Figure 3 .
False positive perfusion defect because of attenuation. An apical perfusion defect is detected using each technique. However, power Doppler shows another apparent defect in the basal septum (arrow), not matched on SPECT or colour coded imaging. This false positive is attributed to attenuation.
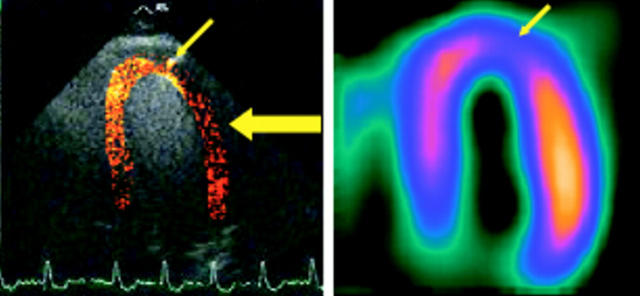
Figure 4 .
Apical defect shown by both single photon emission computed tomography (SPECT) and contrast echo (arrow), with unmatched lateral wall defect by contrast echocardiography (large arrow). This artefact is caused by overlying lung.
Figure 5 .
Apparently normal image with digital subtraction and colour coding in a patient with a mild perfusion defect in the basal septum on the SPECT and power Doppler images (arrows). This false negative contrast pattern with digital subtraction and colour coding reflects difficulties in alignment and superimposition of the images.
Figure 6 .
Discordance between single photon emission computed tomography (SPECT) with all echo techniques. The large septal perfusion defect by SPECT (arrow) is probably the result of left bundle branch block in a patient without a history of coronary artery disease.
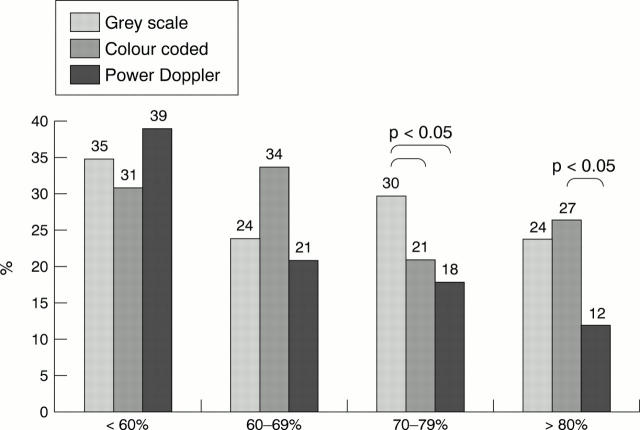
Figure 7 .
Proportion of abnormal segments by myocardial contrast echo (defined by any defect), compared with quantitative SPECT activity (as per cent of maximum).
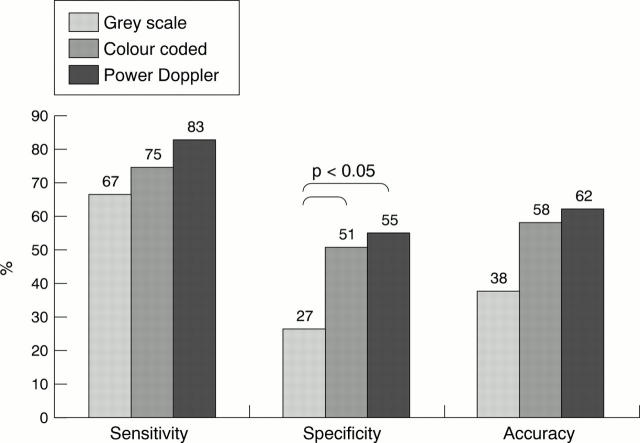
Figure 8 .
Sensitivity, specificity, and accuracy of grey scale, colour coded, and power Doppler techniques for contrast echocardiography.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Agrawal Dipak I., Malhotra Sanjay, Nanda Navin C., Carvalho Truffa Claudia, Agrawal Gopal, Thakur Abhash C., Jamil Farrukh, Taylor Gregg W., Becher Harald. Harmonic Power Doppler Contrast Echocardiography: Preliminary Experimental Results. Echocardiography. 1997 Nov;14(6 Pt 1):631–636. doi: 10.1111/j.1540-8175.1997.tb00773.x. [DOI] [PubMed] [Google Scholar]
- Alazraki N. P., Krawczynska E. G., Kosinski A. S., DePuey E. G., 3rd, Ziffer J. A., Taylor A. T., Jr, Pettigrew R. I., Vansant J. P., Shaw L. J., Weintraub W. S. Prognostic value of thallium-201 single-photon emission computed tomography for patients with multivessel coronary artery disease after revascularization (the Emory Angioplasty versus Surgery Trial [EAST]). Am J Cardiol. 1999 Dec 15;84(12):1369–1374. doi: 10.1016/s0002-9149(99)00578-0. [DOI] [PubMed] [Google Scholar]
- DeMaria A. N., Cotter B., Ohmori K. Myocardial contrast echocardiography: too much, too soon? J Am Coll Cardiol. 1998 Nov;32(5):1270–1271. doi: 10.1016/s0735-1097(98)00415-x. [DOI] [PubMed] [Google Scholar]
- Go R. T., Marwick T. H., MacIntyre W. J., Saha G. B., Neumann D. R., Underwood D. A., Simpfendorfer C. C. A prospective comparison of rubidium-82 PET and thallium-201 SPECT myocardial perfusion imaging utilizing a single dipyridamole stress in the diagnosis of coronary artery disease. J Nucl Med. 1990 Dec;31(12):1899–1905. [PubMed] [Google Scholar]
- Gould K. L. Noninvasive assessment of coronary stenoses by myocardial perfusion imaging during pharmacologic coronary vasodilatation. I. Physiologic basis and experimental validation. Am J Cardiol. 1978 Feb;41(2):267–278. doi: 10.1016/0002-9149(78)90165-0. [DOI] [PubMed] [Google Scholar]
- Hachamovitch R., Berman D. S., Shaw L. J., Kiat H., Cohen I., Cabico J. A., Friedman J., Diamond G. A. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998 Feb 17;97(6):535–543. doi: 10.1161/01.cir.97.6.535. [DOI] [PubMed] [Google Scholar]
- Hansen C. L., Crabbe D., Rubin S. Lower diagnostic accuracy of thallium-201 SPECT myocardial perfusion imaging in women: an effect of smaller chamber size. J Am Coll Cardiol. 1996 Nov 1;28(5):1214–1219. doi: 10.1016/S0735-1097(96)00304-X. [DOI] [PubMed] [Google Scholar]
- Heinle S. K., Noblin J., Goree-Best P., Mello A., Ravad G., Mull S., Mammen P., Grayburn P. A. Assessment of myocardial perfusion by harmonic power Doppler imaging at rest and during adenosine stress: comparison with (99m)Tc-sestamibi SPECT imaging. Circulation. 2000 Jul 4;102(1):55–60. doi: 10.1161/01.cir.102.1.55. [DOI] [PubMed] [Google Scholar]
- Jayaweera A. R., Matthew T. L., Sklenar J., Spotnitz W. D., Watson D. D., Kaul S. Method for the quantitation of myocardial perfusion during myocardial contrast two-dimensional echocardiography. J Am Soc Echocardiogr. 1990 Mar-Apr;3(2):91–98. doi: 10.1016/s0894-7317(14)80501-4. [DOI] [PubMed] [Google Scholar]
- Kaul S. Myocardial contrast echocardiography: 15 years of research and development. Circulation. 1997 Nov 18;96(10):3745–3760. doi: 10.1161/01.cir.96.10.3745. [DOI] [PubMed] [Google Scholar]
- Krishnan R., Lu J., Zhu Y. Y., Dae M. W., Botvinick E. H. Myocardial perfusion scintigraphy in left bundle branch block: a perspective on the issue from image analysis in a clinical context. Am Heart J. 1993 Sep;126(3 Pt 1):578–586. doi: 10.1016/0002-8703(93)90407-z. [DOI] [PubMed] [Google Scholar]
- Marwick T. H., Brunken R., Meland N., Brochet E., Baer F. M., Binder T., Flachskampf F., Kamp O., Nienaber C., Nihoyannopoulos P. Accuracy and feasibility of contrast echocardiography for detection of perfusion defects in routine practice: comparison with wall motion and technetium-99m sestamibi single-photon emission computed tomography. The Nycomed NC100100 Investigators. J Am Coll Cardiol. 1998 Nov;32(5):1260–1269. doi: 10.1016/s0735-1097(98)00373-8. [DOI] [PubMed] [Google Scholar]
- Monaghan M. J., Quigley P. J., Metcalfe J. M., Thomas S. D., Jewitt D. E. Digital subtraction contrast echocardiography: a new method for the evaluation of regional myocardial perfusion. Br Heart J. 1988 Jan;59(1):12–19. doi: 10.1136/hrt.59.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasquet A., Greenberg N., Brunken R., Thomas J. D., Marwick T. H. Effect of color coding and subtraction on the accuracy of contrast echocardiography. Int J Cardiol. 1999 Aug 31;70(3):223–231. doi: 10.1016/s0167-5273(99)00070-4. [DOI] [PubMed] [Google Scholar]
- Porter T. R., Xie F., Kricsfeld A., Kilzer K. Noninvasive identification of acute myocardial ischemia and reperfusion with contrast ultrasound using intravenous perfluoropropane-exposed sonicated dextrose albumin. J Am Coll Cardiol. 1995 Jul;26(1):33–40. doi: 10.1016/0735-1097(95)00132-j. [DOI] [PubMed] [Google Scholar]
- Tiemann Klaus, Becher Harald, Bimmel Dieter, Schlief Reinhard, Nanda Navin C. Stimulated Acoustic Emission Nonbackscatter Contrast Effect of Microbubbles Seen with Harmonic Power Doppler Imaging. Echocardiography. 1997 Jan;14(1):65–70. doi: 10.1111/j.1540-8175.1997.tb00692.x. [DOI] [PubMed] [Google Scholar]
- Vanzetto G., Ormezzano O., Fagret D., Comet M., Denis B., Machecourt J. Long-term additive prognostic value of thallium-201 myocardial perfusion imaging over clinical and exercise stress test in low to intermediate risk patients : study in 1137 patients with 6-year follow-up. Circulation. 1999 Oct 5;100(14):1521–1527. doi: 10.1161/01.cir.100.14.1521. [DOI] [PubMed] [Google Scholar]
- Villanueva F. S., Glasheen W. P., Sklenar J., Jayaweera A. R., Kaul S. Successful and reproducible myocardial opacification during two-dimensional echocardiography from right heart injection of contrast. Circulation. 1992 Apr;85(4):1557–1564. doi: 10.1161/01.cir.85.4.1557. [DOI] [PubMed] [Google Scholar]
- Wei K., Skyba D. M., Firschke C., Jayaweera A. R., Lindner J. R., Kaul S. Interactions between microbubbles and ultrasound: in vitro and in vivo observations. J Am Coll Cardiol. 1997 Apr;29(5):1081–1088. doi: 10.1016/s0735-1097(97)00029-6. [DOI] [PubMed] [Google Scholar]
- Widding A., Hesse B., Gadsboll N. Technetium-99m sestamibi and tetrofosmin myocardial single-photon emission tomography: can we use the same reference data base? Eur J Nucl Med. 1997 Jan;24(1):42–45. doi: 10.1007/BF01728307. [DOI] [PubMed] [Google Scholar]