Abstract
OBJECTIVE—To assess the cost effectiveness of ramipril treatment in patients at low, medium, and high risk of cardiovascular death. DESIGN—Population based cost effectiveness analysis from the perspective of the health care provider in the UK. Effectiveness was modelled using data from the HOPE (heart outcome prevention evaluation) trial. The life table method was used to predict mortality in a medium risk cohort, as in the HOPE trial (2.44% annual mortality), and in low and high risk groups (1% and 4.5% annual mortality, respectively). SETTING—UK population using 1998 government actuary department data. MAIN OUTCOME MEASURE—Cost per life year gained at five years and lifetime treatment with ramipril. RESULTS—Cost effectiveness was £36 600, £13 600, and £4000 per life year gained at five years and £5300, £1900, and £100 per life year gained at 20 years (lifetime treatment) in low, medium, and high risk groups, respectively. Cost effectiveness at 20 years remained well below that of haemodialysis (£25 000 per life year gained) over a range of potential drug costs and savings. Treatment of the HOPE population would cost the UK National Health Service (NHS) an additional £360 million but would prevent 12 000 deaths per annum. CONCLUSIONS—Ramipril is cost effective treatment for cardiovascular risk reduction in patients at medium, high, and low pretreatment risk, with a cost effectiveness comparable with the use of statins. Implementation of ramipril treatment in a medium risk population would result in a major reduction in cardiovascular deaths but would increase annual NHS spending by £360 million. Keywords: angiotensin converting enzyme inhibitor; cardiovascular risk; cost effectiveness; ramipril
Full Text
The Full Text of this article is available as a PDF (134.8 KB).
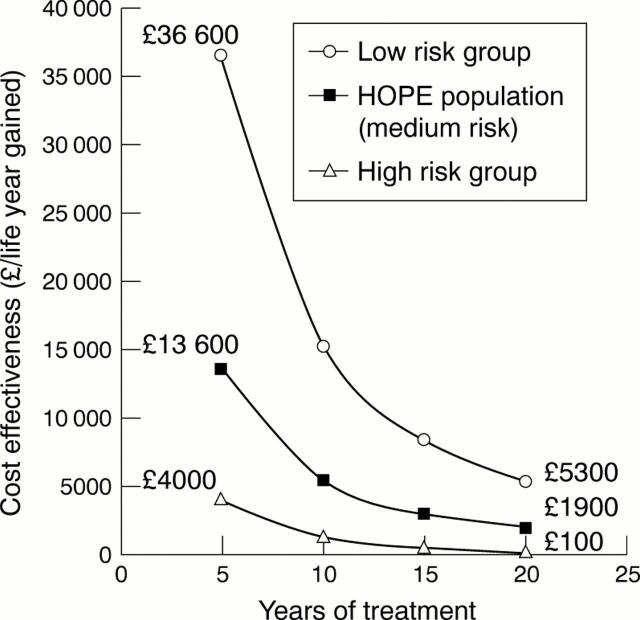
Figure 1 .
Cost effectiveness of ramipril treatment at 5, 10, 15, and 20 years in patients with low (1.0%), medium (2.44%), and high (4.5%) annual mortality rates. Haemodialysis has a cost effectiveness of £25 000 per life year gained. For additional data see eHeart.
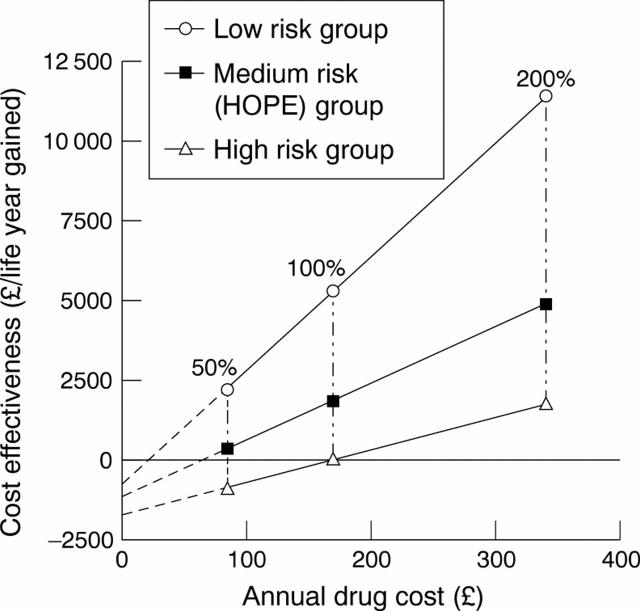
Figure 2 .
Cost effectiveness of lifelong (20 year) treatment with ramipril in low, medium, and high risk populations related drug cost at 50%, 100%, and 200% of present prices. For additional data see eHeart.
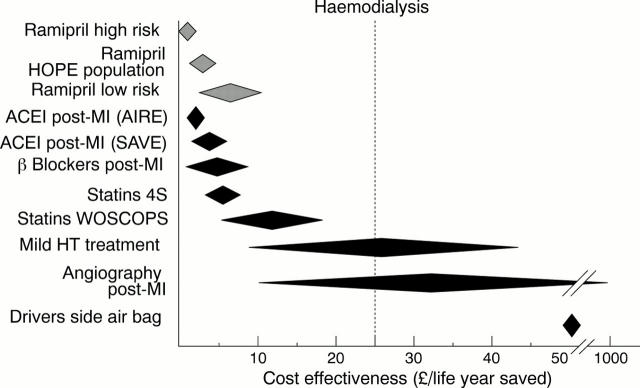
Figure 3 .
Cost effectiveness of ramipril treatment continued for 5, 10, 15, and 20 years in a low risk population. Cost effectiveness of haemodialysis is £25 000 per life year gained (shown as dotted line). (A) The effect of varying drug costs. (B) The effect of varying potential savings. For additional data see eHeart.
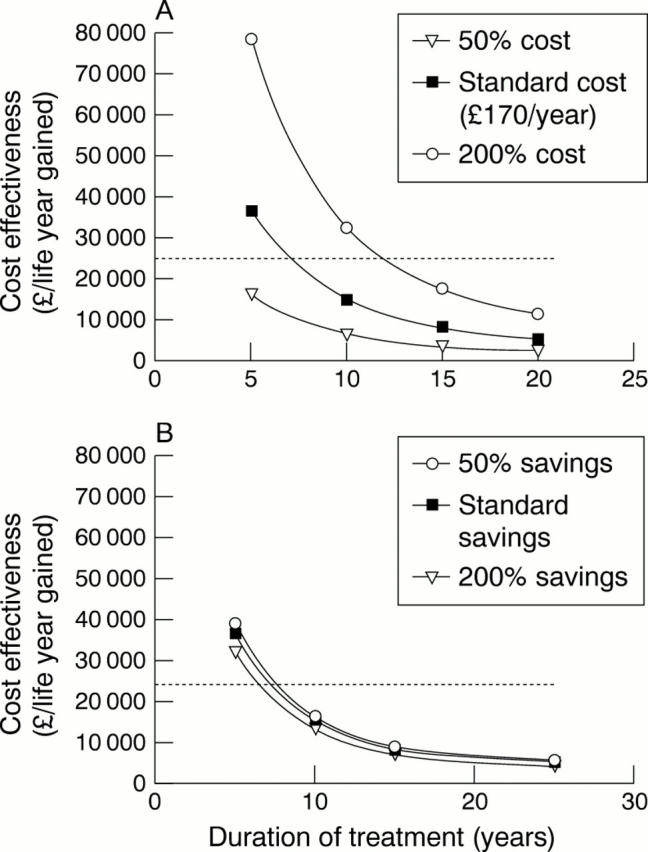
Figure 4 .
Comparison of cost effectiveness of ramipril treatment with other cardiovascular and non-cardiovascular interventions. Estimates from previous studies are in 1994-1995 UK pounds.7 9 23 24 35 ACEI, angiotensin converting enzyme inhibitor; HT, hypertension; MI, myocardial infarction. See text for explanation of trial acronyms.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baigent C., Collins R., Appleby P., Parish S., Sleight P., Peto R. ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. The ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. BMJ. 1998 May 2;316(7141):1337–1343. doi: 10.1136/bmj.316.7141.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erhardt L., Ball S., Andersson F., Bergentoft P., Martinez C. Cost effectiveness in the treatment of heart failure with ramipril. A Swedish substudy of the AIRE study. Acute Infarction Ramipril Efficacy. Pharmacoeconomics. 1997 Aug;12(2 Pt 2):256–266. doi: 10.2165/00019053-199712020-00016. [DOI] [PubMed] [Google Scholar]
- Freemantle N., Cleland J., Young P., Mason J., Harrison J. beta Blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999 Jun 26;318(7200):1730–1737. doi: 10.1136/bmj.318.7200.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman L., Sia S. T., Cook E. F., Rutherford J. D., Weinstein M. C. Costs and effectiveness of routine therapy with long-term beta-adrenergic antagonists after acute myocardial infarction. N Engl J Med. 1988 Jul 21;319(3):152–157. doi: 10.1056/NEJM198807213190306. [DOI] [PubMed] [Google Scholar]
- Hall A. S., Murray G. D., Ball S. G. Follow-up study of patients randomly allocated ramipril or placebo for heart failure after acute myocardial infarction: AIRE Extension (AIREX) Study. Acute Infarction Ramipril Efficacy. Lancet. 1997 May 24;349(9064):1493–1497. doi: 10.1016/s0140-6736(97)04442-5. [DOI] [PubMed] [Google Scholar]
- Jönsson B., Johannesson M., Kjekshus J., Olsson A. G., Pedersen T. R., Wedel H. Cost-effectiveness of cholesterol lowering. Results from the Scandinavian Simvastatin Survival Study (4S) Eur Heart J. 1996 Jul;17(7):1001–1007. doi: 10.1093/oxfordjournals.eurheartj.a014994. [DOI] [PubMed] [Google Scholar]
- Mason J., Drummond M., Torrance G. Some guidelines on the use of cost effectiveness league tables. BMJ. 1993 Feb 27;306(6877):570–572. doi: 10.1136/bmj.306.6877.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menkes D. B. Hazardous drugs in developing countries. BMJ. 1997 Dec 13;315(7122):1557–1558. doi: 10.1136/bmj.315.7122.1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickin D. M., McCabe C. J., Ramsay L. E., Payne N., Haq I. U., Yeo W. W., Jackson P. R. Cost effectiveness of HMG-CoA reductase inhibitor (statin) treatment related to the risk of coronary heart disease and cost of drug treatment. Heart. 1999 Sep;82(3):325–332. doi: 10.1136/hrt.82.3.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutherford J. D., Pfeffer M. A., Moyé L. A., Davis B. R., Flaker G. C., Kowey P. R., Lamas G. A., Miller H. S., Packer M., Rouleau J. L. Effects of captopril on ischemic events after myocardial infarction. Results of the Survival and Ventricular Enlargement trial. SAVE Investigators. Circulation. 1994 Oct;90(4):1731–1738. doi: 10.1161/01.cir.90.4.1731. [DOI] [PubMed] [Google Scholar]
- Sacks F. M., Pfeffer M. A., Moye L. A., Rouleau J. L., Rutherford J. D., Cole T. G., Brown L., Warnica J. W., Arnold J. M., Wun C. C. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996 Oct 3;335(14):1001–1009. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- Schädlich P. K., Huppertz E., Brecht J. G. Cost-effectiveness analysis of ramipril in heart failure after myocardial infarction. Economic evaluation of the Acute Infarction Ramipril Efficacy (AIRE) study for Germany from the perspective of Statutory Health Insurance. Pharmacoeconomics. 1998 Dec;14(6):653–669. doi: 10.2165/00019053-199814060-00006. [DOI] [PubMed] [Google Scholar]
- Shepherd J., Cobbe S. M., Ford I., Isles C. G., Lorimer A. R., MacFarlane P. W., McKillop J. H., Packard C. J. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995 Nov 16;333(20):1301–1307. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- Swedberg K., Kjekshus J., Snapinn S. Long-term survival in severe heart failure in patients treated with enalapril. Ten year follow-up of CONSENSUS I. Eur Heart J. 1999 Jan;20(2):136–139. doi: 10.1053/euhj.1998.1098. [DOI] [PubMed] [Google Scholar]
- Ul Haq I., Ramsay L. E., Pickin D. M., Yeo W. W., Jackson P. R., Payne J. N. Lipid-lowering for prevention of coronary heart disease: what policy now? Clin Sci (Lond) 1996 Oct;91(4):399–413. doi: 10.1042/cs0910399. [DOI] [PubMed] [Google Scholar]
- Yusuf S., Sleight P., Pogue J., Bosch J., Davies R., Dagenais G. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med. 2000 Jan 20;342(3):145–153. doi: 10.1056/NEJM200001203420301. [DOI] [PubMed] [Google Scholar]
- Zuanetti G., Latini R., Maggioni A. P., Franzosi M., Santoro L., Tognoni G. Effect of the ACE inhibitor lisinopril on mortality in diabetic patients with acute myocardial infarction: data from the GISSI-3 study. Circulation. 1997 Dec 16;96(12):4239–4245. doi: 10.1161/01.cir.96.12.4239. [DOI] [PubMed] [Google Scholar]