Full Text
The Full Text of this article is available as a PDF (466.1 KB).
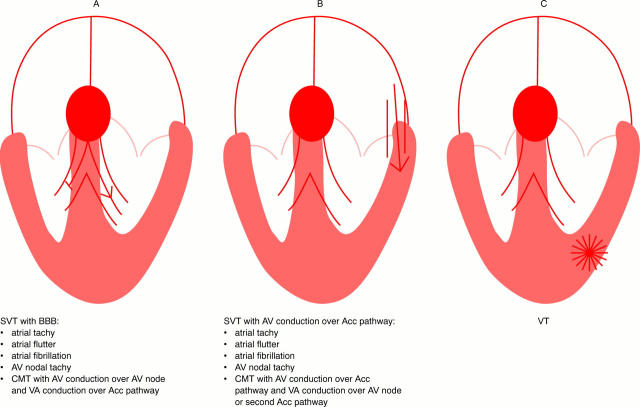
Figure 1: .
Different types of SVT with BBB (diagram A), SVT with AV conduction over an accessory pathway (diagram B), and VT (diagram C) resulting in a broad QRS tachycardia. Acc, accessory; AV, atrioventricular; BBB, bundle branch block; CMT, circus movement tachycardia; SVT, supraventricular tachycardia; VA, ventriculo-atrial; VT, ventricular tachycardia.
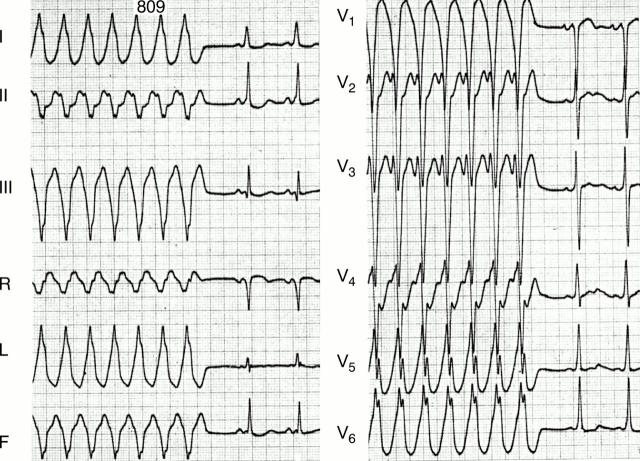
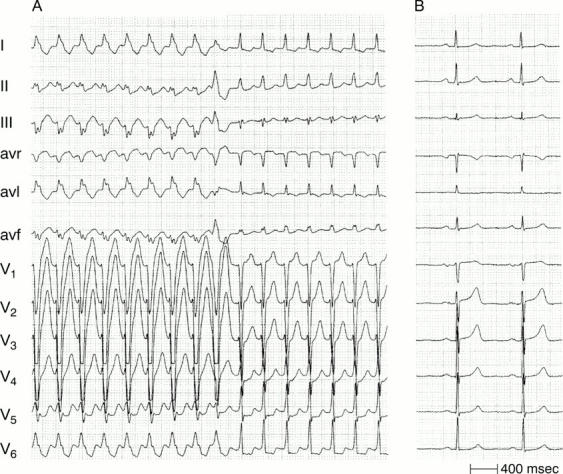
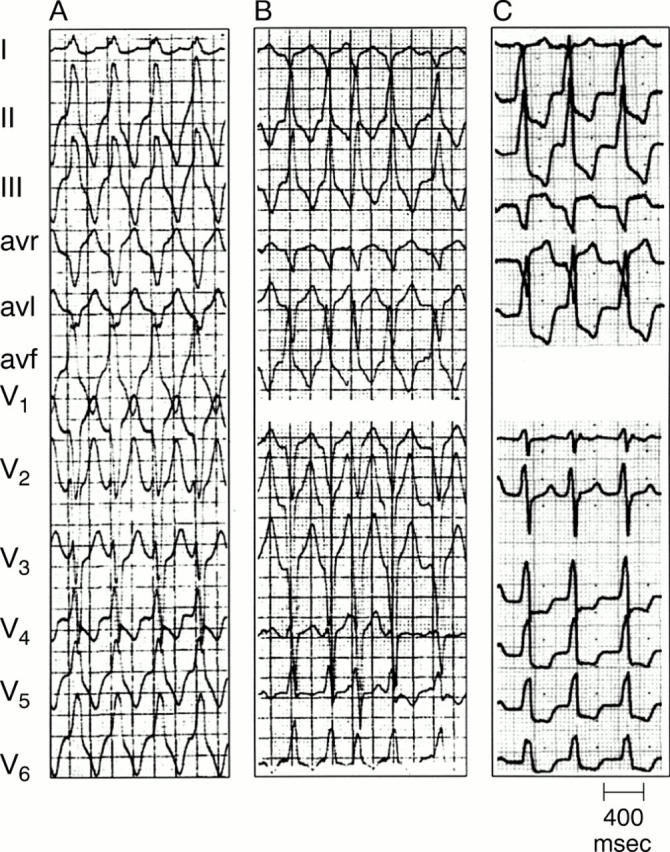
Figure 2: .
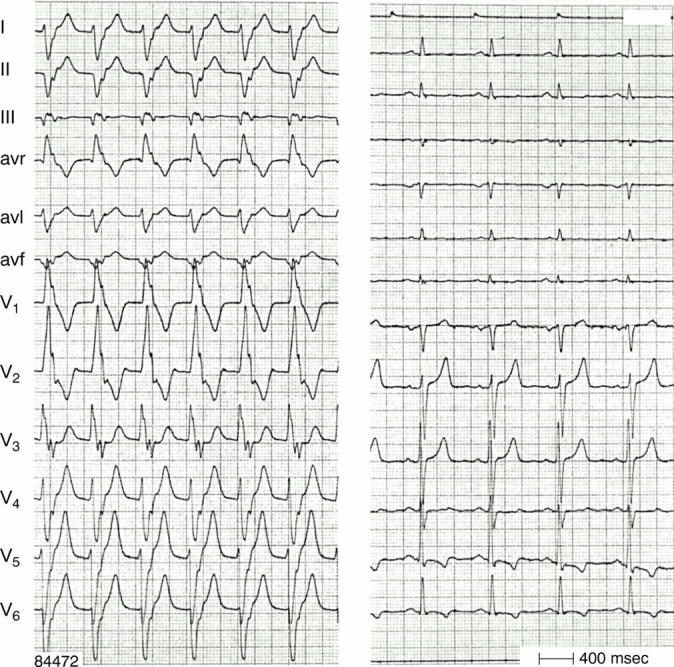
Two types of VT (panel A and B) in the same patient (panel C during sinus rhythm). Atrioventricular dissociation is present during both VTs. Note the effect of the frontal plane axis on the R:S ratio in lead V6 in RBBB shaped VT. R:S < 1 is present in case of a superior axis (panel B), but R:S > 1 with an inferior axis (panel A). Figure 3: One to one ventriculo-atrial conduction during VT. The p waves are negative in leads II, III, and avf and follow each QRS complex. Left panel—VT; right panel—same patient during sinus rhythm.
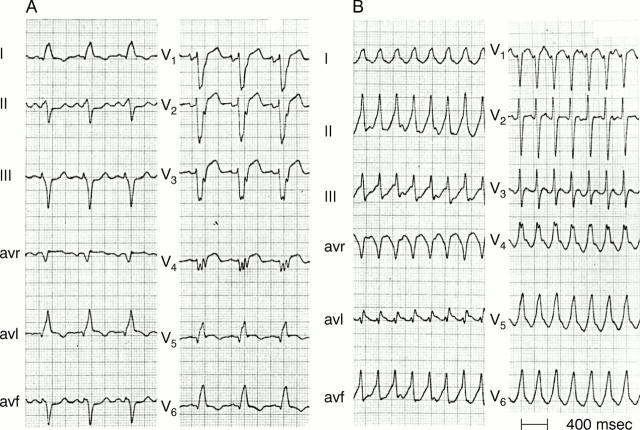
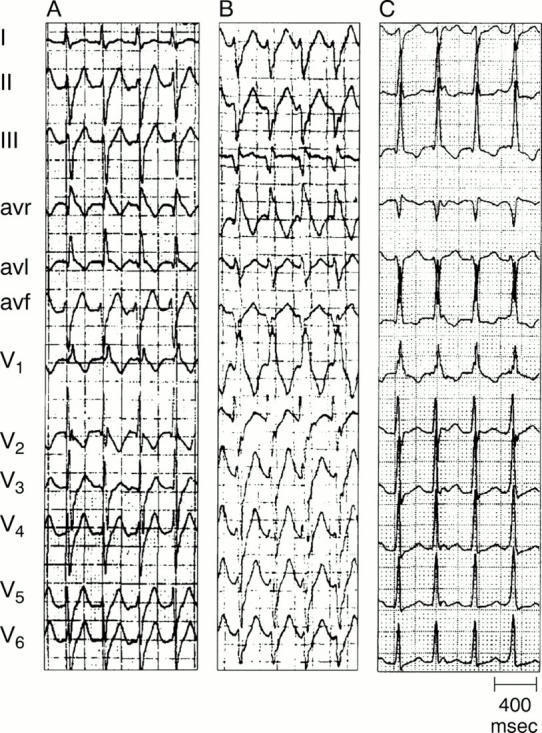
Figure 4: .
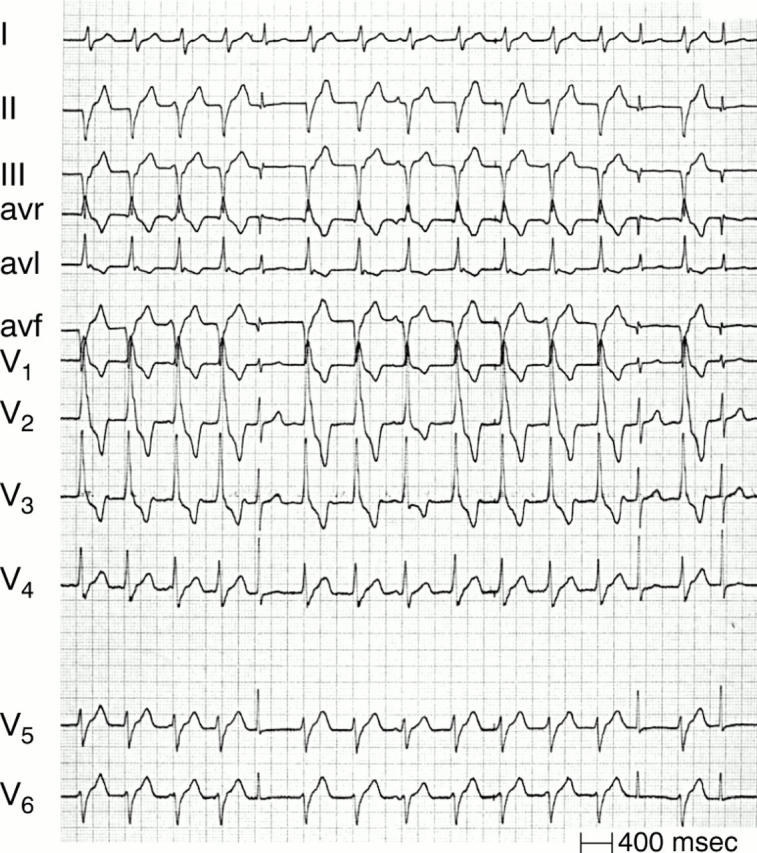
"Capture" (QRS complexes: 5, 13, and 15) and "fusion" beats (QRS complex number 8) during VT.
Figure 5: .
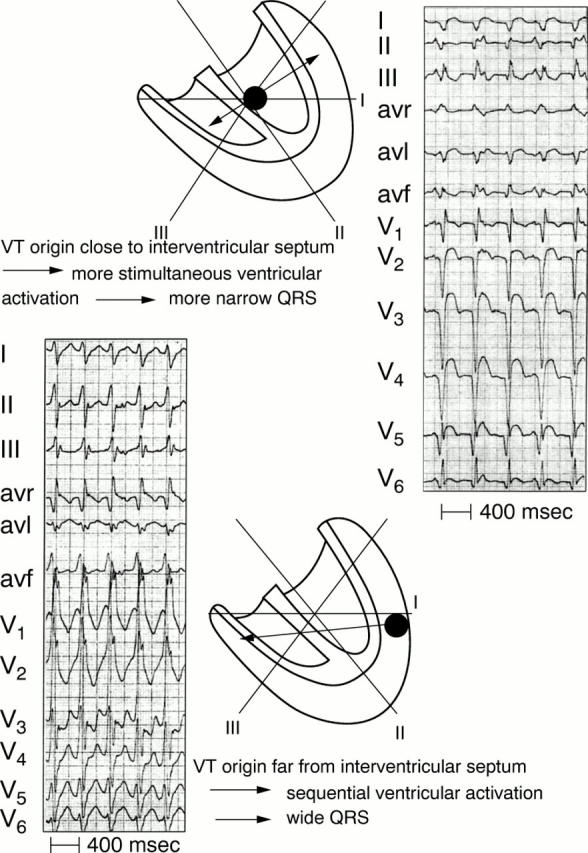
VT origin and QRS width. Upper panel: an origin close to the interventricular septum results in more simultaneous right and left ventricular activation and therefore a more narrow QRS complex. In contrast (lower panel) a VT origin in the lateral ventricular wall results in sequential ventricular activation and a wider QRS complex.
Figure 6: .
An antidromic circus movement tachycardia with AV conduction over a right sided accessory pathway. The insertion of the accessory pathway in the free wall of the right ventricle results in sequential (right to left) ventricular activation and a wide QRS complex.
Figure 7: .
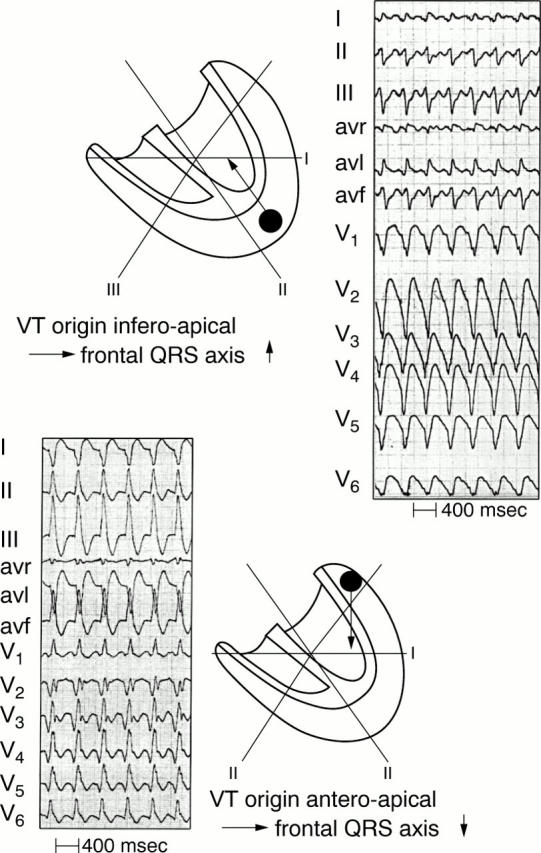
VT origin and QRS axis. An apical origin results in a superiorly directed axis in the frontal plane. In contrast, a basal origin leads to an inferior QRS axis (lower panel).
Figure 8: .
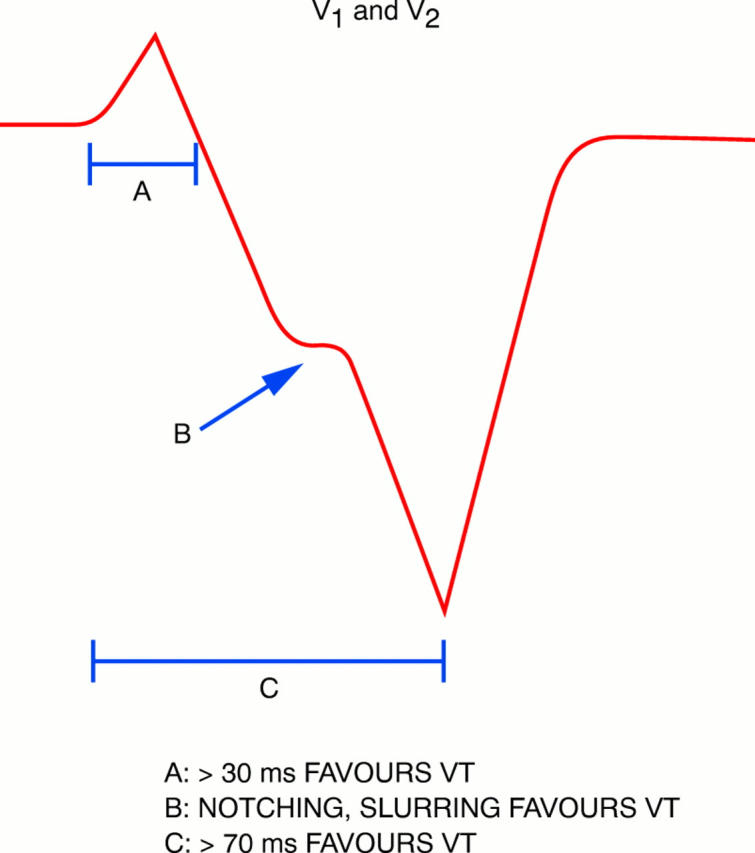
Findings in lead V1 and V2 during LBBB shaped tachycardia pointing to a ventricular origin (see text).
Figure 9: .
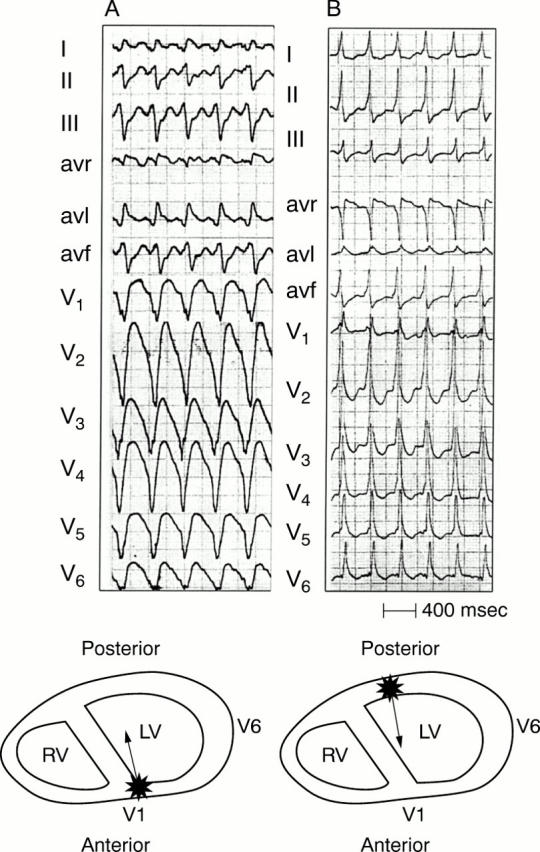
SVT with LBBB. In panel A LBBB changes during tachycardia into a narrow QRS following a ventricular premature beat. As described in the text, lead V1 during LBBB clearly shows signs pointing to a supraventricular origin of the tachycardia. Figure 10: Concordant pattern. The left panel shows a VT arising in the apical area of the left ventricle resulting in negative concordancy of all precordial leads. In the right panel ventricular activation starts in the left posterior area, resulting in positive concordancy of all precordial leads. The latter can be found in left posterior VT but also in SVT with AV conduction over a left posterior accessory pathway.
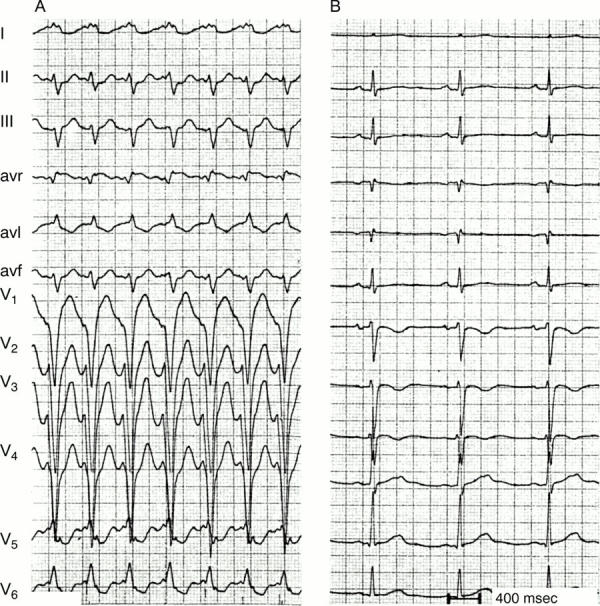
Figure 11: .
Tachycardia QRS smaller than QRS during sinus rhythm. On the left sinus rhythm is present with a very wide QRS because of anterolateral myocardial infarction and pronounced delay in left ventricular activation. On the right a VT arising on the right side of the interventricular septum results in more simultaneous activation of the right and left ventricle than during sinus rhythm and therefore a smaller QRS complex.
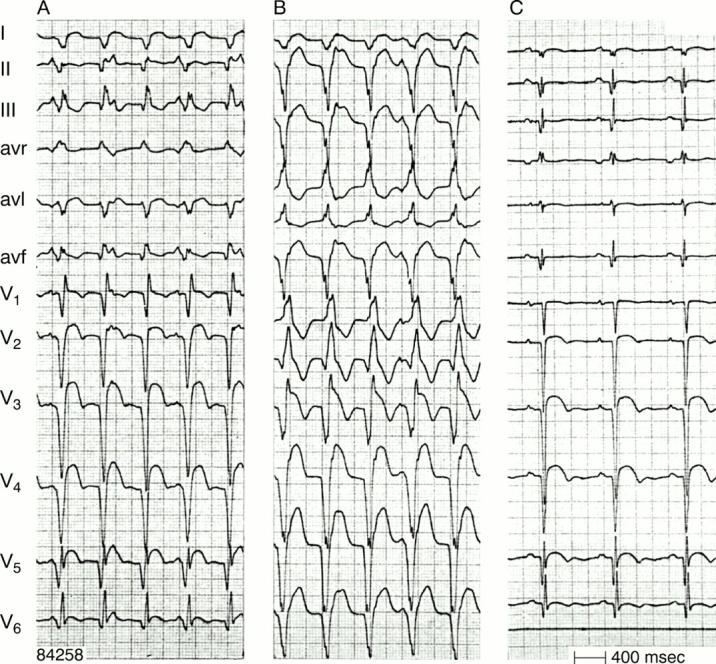
Figure 12: .
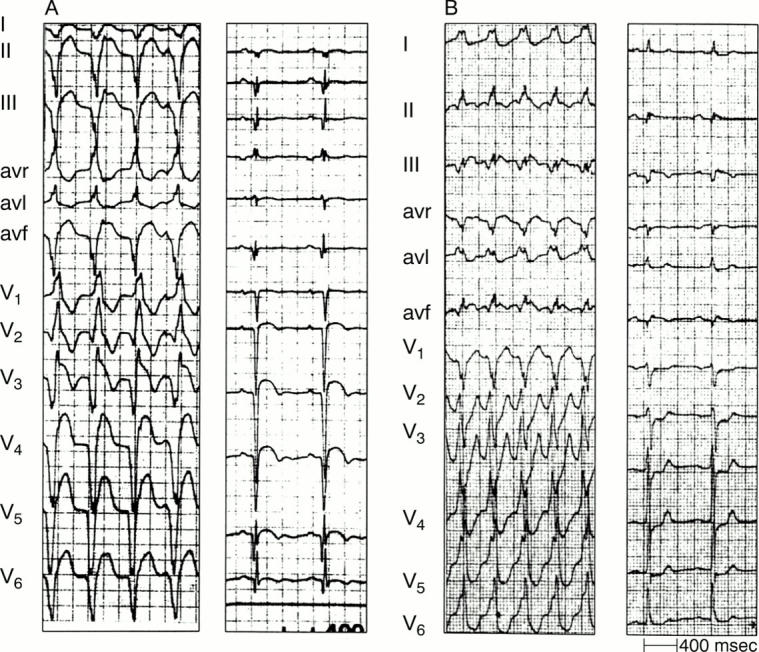
QRS complexes during VT indicating a myocardial scar. As shown by the accompanying tracing, during sinus rhythm anterior wall myocardial infarction is present in the left panel and inferior wall myocardial infarction in the right one.
Figure 13: .
Three types of idiopathic VT arising in or close to the outflow tract of the right ventricle (see text).
Figure 14: .
Three types of left ventricular idiopathic VT (see text).
Figure 15: .
VT in arrhythmogenic right ventricular dysplasia (ARVD). VT shows LBBB shape and left axis deviation indicating an origin in the apex of the right ventricle. Note also the negative T waves in V1-V3 during sinus rhythm, which is often found in ARVD.
Figure 16: .
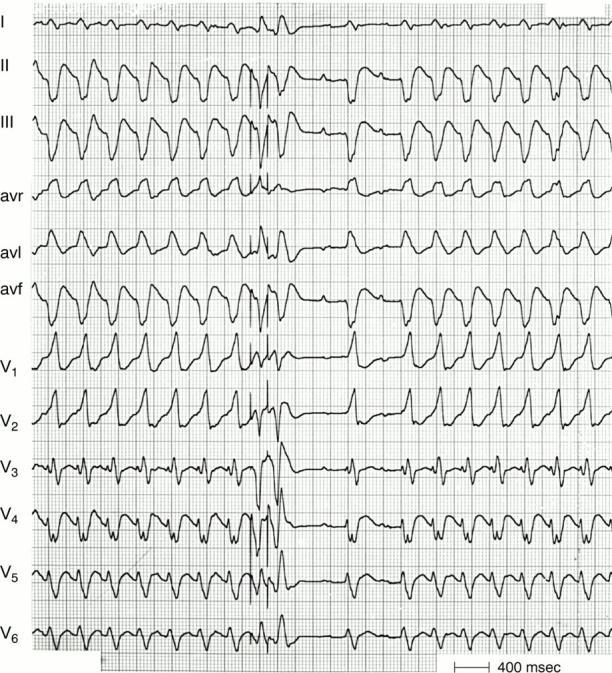
Bundle branch re-entry VT. Following two electrically induced premature beats the tachycardia terminates in the middle of the recording. However, tachycardia resumes after two conducted sinus beats. The QRS is identical during sinus rhythm and tachycardia. Note the presence of AV dissociation during tachycardia indicating a ventricular origin.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brugada P., Brugada J., Mont L., Smeets J., Andries E. W. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991 May;83(5):1649–1659. doi: 10.1161/01.cir.83.5.1649. [DOI] [PubMed] [Google Scholar]
- Buxton A. E., Marchlinski F. E., Doherty J. U., Flores B., Josephson M. E. Hazards of intravenous verapamil for sustained ventricular tachycardia. Am J Cardiol. 1987 May 1;59(12):1107–1110. doi: 10.1016/0002-9149(87)90857-5. [DOI] [PubMed] [Google Scholar]
- Coumel P., Leclercq J. F., Attuel P., Maisonblanche P. The QRS morphology in post-myocardial infarction ventricular tachycardia. A study of 100 tracings compared with 70 cases of idiopathic ventricular tachycardia. Eur Heart J. 1984 Oct;5(10):792–805. doi: 10.1093/oxfordjournals.eurheartj.a061568. [DOI] [PubMed] [Google Scholar]
- Dancy M., Camm A. J., Ward D. Misdiagnosis of chronic recurrent ventricular tachycardia. Lancet. 1985 Aug 10;2(8450):320–323. doi: 10.1016/s0140-6736(85)90363-0. [DOI] [PubMed] [Google Scholar]
- Harvey W. P., Ronan J. A., Jr Bedside diagnosis of arrhythmias. Prog Cardiovasc Dis. 1966 Mar;8(5):419–445. doi: 10.1016/s0033-0620(66)80030-0. [DOI] [PubMed] [Google Scholar]
- Kindwall K. E., Brown J., Josephson M. E. Electrocardiographic criteria for ventricular tachycardia in wide complex left bundle branch block morphology tachycardias. Am J Cardiol. 1988 Jun 1;61(15):1279–1283. doi: 10.1016/0002-9149(88)91169-1. [DOI] [PubMed] [Google Scholar]
- Leclercq J. F., Coumel P. Characteristics, prognosis and treatment of the ventricular arrhythmias of right ventricular dysplasia. Eur Heart J. 1989 Sep;10 (Suppl 500):61–67. doi: 10.1093/eurheartj/10.suppl_d.61. [DOI] [PubMed] [Google Scholar]
- Marriott H. J. Differential diagnosis of supraventricular and ventricular tachycardia. Geriatrics. 1970 Nov;25(11):91–101. [PubMed] [Google Scholar]
- Stewart R. B., Bardy G. H., Greene H. L. Wide complex tachycardia: misdiagnosis and outcome after emergent therapy. Ann Intern Med. 1986 Jun;104(6):766–771. doi: 10.7326/0003-4819-104-6-766. [DOI] [PubMed] [Google Scholar]
- Touboul P., Kirkorian G., Atallah G., Lavaud P., Moleur P., Lamaud M., Mathieu M. P. Bundle branch reentrant tachycardia treated by electrical ablation of the right bundle branch. J Am Coll Cardiol. 1986 Jun;7(6):1404–1409. doi: 10.1016/s0735-1097(86)80163-2. [DOI] [PubMed] [Google Scholar]
- Wellens H. J., Bär F. W., Lie K. I. The value of the electrocardiogram in the differential diagnosis of a tachycardia with a widened QRS complex. Am J Med. 1978 Jan;64(1):27–33. doi: 10.1016/0002-9343(78)90176-6. [DOI] [PubMed] [Google Scholar]