Abstract
Aim—The World Health Organisation (WHO) haemoglobin colour scale has been developed as a simple, inexpensive clinical device for diagnosing anaemia when laboratory based haemoglobinometry is not available. In an initial validation study at several health centres, scale readings were compared with measurements of haemoglobin by the laboratory. This showed the scale to have 90% sensitivity and 70% specificity in identifying whether anaemia was present or not. In addition, when present, the degree of anaemia was correctly classified in clinical terms as moderate, pronounced, or severe, with an overall sensitivity of 60% and specificity of 88%. Errors were mainly marginal—that is, between two adjacent categories—but there were also some major discrepancies, such as a blood with a haemoglobin of 6–7 g/dl being read as normal or vice versa. Because this would compromise the scale's reliability in practice, this study was undertaken to identify the causes of the discrepancies and to reassess the performance of the scale.
Methods—Venous blood samples were collected into potassium EDTA from patients attending selected clinics at three South African hospitals with good laboratory facilities. A prototype of the device was used unsupervised by nursing staff, doctors, and phlebotomists, who were told to follow the printed instructions. The blood specimens were then immediately sent to the laboratory where haemoglobin was measured by standardised automated blood cell counters. Any discrepancies > 1 g/dl were recorded and the tests were repeated by the same operators under supervision of the investigators.
Results—Almost all the errors that occurred resulted from the incorrect use of the device, namely: inadequate or excessive blood, reading the results too soon or too late (beyond the limit of two minutes), poor lighting, or holding the scale at the wrong angle. The accuracy improved dramatically when the tests were repeated under supervision and these faults were avoided: 95% of readings were within 1 g/dl of the reference measurements, and 97% within 1.5 g/dl. Anaemia screening showed 96% sensitivity and 86% specificity. Clinical judgement of pallor was frequently wrong, whereas the scale gave the correct diagnosis in more than 97% of cases.
Conclusion—The study confirmed the usefulness and reliability of the scale and its advantage over clinical signs for the diagnosis of anaemia, thus providing a clinically reliable near patient method in the absence of a laboratory. The instructions are easy to follow but must be strictly adhered to.
Key Words: diagnosis of anaemia • haemoglobinometry • haemoglobin colour scale • clinical assessment of anaemia
Full Text
The Full Text of this article is available as a PDF (150.2 KB).
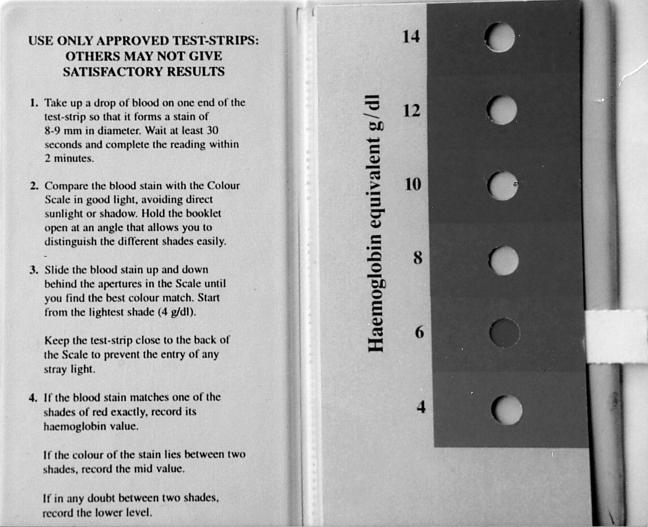
Figure 1 The World Health Organisation haemoglobin colour scale.