Abstract
Aims—To evaluate the usefulness of the devR based polymerase chain reaction (PCR) in the detection of Mycobacterium tuberculosis in lymph node aspirates and tissues of lymphadenitis and to compare PCR with conventional diagnostic techniques.
Subjects and methods—Coded specimens of fine needle aspirates and biopsies from 22 patients with tuberculous lymphadenitis, 14 patients with non-tubercular lymphadenitis, and nine patients with granulomatous lymphadenitis were processed and subjected to analysis by PCR, smear microscopy, M tuberculosis culture, histology, and cytology.
Results—Tuberculous lymphadenitis was correctly diagnosed by PCR in 18 patients, by culture in five patients, by histology in 13 patients, and by cytology in seven patients. PCR gave two false positive results in 14 patients with non-tubercular lymphadenitis. The sensitivity of the conventional techniques was significantly higher with biopsies (17 of 22 specimens; 77%) than with fine needle aspirates (nine of 22 specimens; 41%). However, the sensitivity of PCR was not significantly higher with biopsies (68%) in comparison with fine needle aspirates (55%). The sensitivity of either biopsy PCR or fine needle aspirate PCR was not significantly different from that of either histology combined with culture or cytology combined with culture. The overall combined specificity of PCR was 86%. Mycobacterium tuberculosis DNA was detected in six of nine patients with granulomatous lymphadenitis.
Conclusion—PCR is the most sensitive single technique available to date for the demonstration of M tuberculosis in specimens derived from patients with a clinical suspicion of tuberculous lymphadenitis. The value of PCR lies in its use as an adjunct test in the diagnosis of tuberculous lymphadenitis, particularly in those patients where conventional methods fail. Because fine needle aspiration is not an invasive procedure, it is the procedure of choice, and PCR should be performed initially on these samples. Excisional biopsy histology and PCR should be recommended only for patients in whom fine needle aspirate PCR is negative or when there is discrepancy with the clinical impression.
Key Words: Mycobacterium tuberculosis • devR polymerase chain reaction • tuberculous lymphadenitis
Full Text
The Full Text of this article is available as a PDF (156.2 KB).
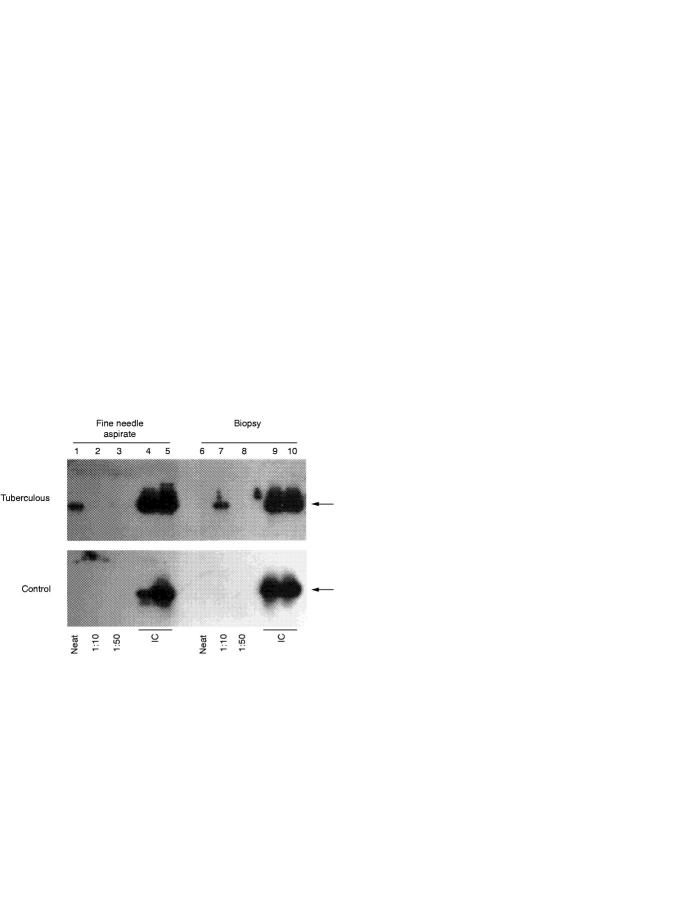
Figure 1 Polymerase chain reaction (PCR) test and inhibitor check reactions on fine needle aspirates and biopsies. PCR assays were set up with DNA from fine needle aspirate and biopsy specimens of a patient with tuberculous lymphadenitis (tuberculous panel) and a patient with non-tubercular lymphadenitis (control panel). The products of the amplification reactions were electrophoresed, transferred to a nylon membrane, and detected by hybridisation to a γ32P ATP end labelled oligonucleotide, devR1,20 followed by autoradiography. Lanes 1 and 6, neat test DNA sample (5 µl); lanes 2 and 7, 1/10 dilution of test DNA (5 µl); lanes 3 and 8, 1/50 dilution of test DNA (5 µl); lanes 4 and 9, inhibitor check reactions containing neat test DNA (5 µl) spiked with Mycobacterium tuberculosis DNA (10 ng); lanes 5 and 10, inhibitor check reactions containing 1/50 dilution of test DNA (5 µl) spiked with M tuberculosis DNA (10 ng). The arrows indicate the amplification product of the devR gene.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Appling D., Miller R. H. Mycobacterium cervical lymphadenopathy: 1981 update. Laryngoscope. 1981 Aug;91(8):1259–1266. doi: 10.1288/00005537-198108000-00006. [DOI] [PubMed] [Google Scholar]
- Cegielski J. P., Devlin B. H., Morris A. J., Kitinya J. N., Pulipaka U. P., Lema L. E., Lwakatare J., Reller L. B. Comparison of PCR, culture, and histopathology for diagnosis of tuberculous pericarditis. J Clin Microbiol. 1997 Dec;35(12):3254–3257. doi: 10.1128/jcm.35.12.3254-3257.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarridge J. E., 3rd, Shawar R. M., Shinnick T. M., Plikaytis B. B. Large-scale use of polymerase chain reaction for detection of Mycobacterium tuberculosis in a routine mycobacteriology laboratory. J Clin Microbiol. 1993 Aug;31(8):2049–2056. doi: 10.1128/jcm.31.8.2049-2056.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dandapat M. C., Mishra B. M., Dash S. P., Kar P. K. Peripheral lymph node tuberculosis: a review of 80 cases. Br J Surg. 1990 Aug;77(8):911–912. doi: 10.1002/bjs.1800770823. [DOI] [PubMed] [Google Scholar]
- Ding S., Zhang N., Bu H. [Tuberculous lymphadenitis: a sarcoidosis-like variation]. Zhonghua Bing Li Xue Za Zhi. 1995 Apr;24(2):83–85. [PubMed] [Google Scholar]
- Ersöz C., Polat A., Serin M. S., Soylu L., Demircan O. Fine needle aspiration (FNA) cytology in tuberculous lymphadenitis. Cytopathology. 1998 Jun;9(3):201–207. doi: 10.1046/j.1365-2303.1998.00073.x. [DOI] [PubMed] [Google Scholar]
- Fidler H. M., Rook G. A., Johnson N. M., McFadden J. Mycobacterium tuberculosis DNA in tissue affected by sarcoidosis. BMJ. 1993 Feb 27;306(6877):546–549. doi: 10.1136/bmj.306.6877.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finfer M., Perchick A., Burstein D. E. Fine needle aspiration biopsy diagnosis of tuberculous lymphadenitis in patients with and without the acquired immune deficiency syndrome. Acta Cytol. 1991 May-Jun;35(3):325–332. [PubMed] [Google Scholar]
- Gupta A. K., Nayar M., Chandra M. Critical appraisal of fine needle aspiration cytology in tuberculous lymphadenitis. Acta Cytol. 1992 May-Jun;36(3):391–394. [PubMed] [Google Scholar]
- Gupta S. K., Chugh T. D., Sheikh Z. A., al-Rubah N. A. Cytodiagnosis of tuberculous lymphadenitis. A correlative study with microbiologic examination. Acta Cytol. 1993 May-Jun;37(3):329–332. [PubMed] [Google Scholar]
- Hooper A. A. Tuberculous peripheral lymphadenitis. Br J Surg. 1972 May;59(5):353–359. doi: 10.1002/bjs.1800590506. [DOI] [PubMed] [Google Scholar]
- Ieven M., Goossens H. Relevance of nucleic acid amplification techniques for diagnosis of respiratory tract infections in the clinical laboratory. Clin Microbiol Rev. 1997 Apr;10(2):242–256. doi: 10.1128/cmr.10.2.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S. S., Chung S. M., Kim J. N., Lee M. A., Ha E. H. Application of PCR from the fine needle aspirates for the diagnosis of cervical tuberculous lymphadenitis. J Korean Med Sci. 1996 Apr;11(2):127–132. doi: 10.3346/jkms.1996.11.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnaswami H., Koshi G., Kulkarni K. G., Job C. K. Tuberculous lymphadenitis in South India--a histopathological and bacteriological study. Tubercle. 1972 Sep;53(3):215–220. doi: 10.1016/0041-3879(72)90019-0. [DOI] [PubMed] [Google Scholar]
- Kuwano K., Minamide W., Kusunoki S., Igimi H., Fujiki T., Matsuba K., Hara N. Evaluation of nested polymerase chain reaction for detecting mycobacterial DNA in pleural fluid. Kansenshogaku Zasshi. 1995 Feb;69(2):175–180. doi: 10.11150/kansenshogakuzasshi1970.69.175. [DOI] [PubMed] [Google Scholar]
- Lau S. K., Wei W. I., Hsu C., Engzell U. C. Efficacy of fine needle aspiration cytology in the diagnosis of tuberculous cervical lymphadenopathy. J Laryngol Otol. 1990 Jan;104(1):24–27. doi: 10.1017/s0022215100111697. [DOI] [PubMed] [Google Scholar]
- Nguyen L. N., Kox L. F., Pham L. D., Kuijper S., Kolk A. H. The potential contribution of the polymerase chain reaction to the diagnosis of tuberculous meningitis. Arch Neurol. 1996 Aug;53(8):771–776. doi: 10.1001/archneur.1996.00550080093017. [DOI] [PubMed] [Google Scholar]
- Pfyffer G. E., Kissling P., Jahn E. M., Welscher H. M., Salfinger M., Weber R. Diagnostic performance of amplified Mycobacterium tuberculosis direct test with cerebrospinal fluid, other nonrespiratory, and respiratory specimens. J Clin Microbiol. 1996 Apr;34(4):834–841. doi: 10.1128/jcm.34.4.834-841.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radhika S., Gupta S. K., Chakrabarti A., Rajwanshi A., Joshi K. Role of culture for mycobacteria in fine-needle aspiration diagnosis of tuberculous lymphadenitis. Diagn Cytopathol. 1989;5(3):260–262. doi: 10.1002/dc.2840050306. [DOI] [PubMed] [Google Scholar]
- Sahadevan R., Narayanan S., Paramasivan C. N., Prabhakar R., Narayanan P. R. Restriction fragment length polymorphism typing of clinical isolates of Mycobacterium tuberculosis from patients with pulmonary tuberculosis in Madras, India, by use of direct-repeat probe. J Clin Microbiol. 1995 Nov;33(11):3037–3039. doi: 10.1128/jcm.33.11.3037-3039.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh K. K., Nair M. D., Radhakrishnan K., Tyagi J. S. Utility of PCR assay in diagnosis of en-plaque tuberculoma of the brain. J Clin Microbiol. 1999 Feb;37(2):467–470. doi: 10.1128/jcm.37.2.467-470.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavik T., Wolfaardt M., van Zyl H., Simson I. W. HIV-1 infection in patients with tuberculous lymphadenitis. S Afr Med J. 1996 Jan;86(1):92–92. [PubMed] [Google Scholar]
- Tarng D. C., Su W. J., Huang T. P. PCR diagnosis on formalin-fixed, paraffin-embedded tissues with acid-fast stain and culture negativity in chronic dialysis patients of cervico-mediastinal tuberculous lymphadenitis. Nephrol Dial Transplant. 1998 Jun;13(6):1543–1546. doi: 10.1093/ndt/13.6.1543. [DOI] [PubMed] [Google Scholar]
- Thierry D., Cave M. D., Eisenach K. D., Crawford J. T., Bates J. H., Gicquel B., Guesdon J. L. IS6110, an IS-like element of Mycobacterium tuberculosis complex. Nucleic Acids Res. 1990 Jan 11;18(1):188–188. doi: 10.1093/nar/18.1.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tötsch M., Böcker W., Brömmelkamp E., Fille M., Kreczy A., Ofner D., Schmid K. W., Dockhorn-Dworniczak B. Diagnostic value of different PCR assays for the detection of mycobacterial DNA in granulomatous lymphadenopathy. J Pathol. 1996 Feb;178(2):221–226. doi: 10.1002/(SICI)1096-9896(199602)178:2<221::AID-PATH441>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- Wong C. F., Yew W. W., Wong P. C., Lee J. A case of concomitant tuberculosis and sarcoidosis with mycobacterial DNA present in the sarcoid lesion. Chest. 1998 Aug;114(2):626–629. [PubMed] [Google Scholar]
- Yuen K. Y., Yam W. C., Wong L. P., Seto W. H. Comparison of two automated DNA amplification systems with a manual one-tube nested PCR assay for diagnosis of pulmonary tuberculosis. J Clin Microbiol. 1997 Jun;35(6):1385–1389. doi: 10.1128/jcm.35.6.1385-1389.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang N. X., Ding S. L., Bu H. [Reactive histiocytosis variant of tuberculous lymphadenitis]. Zhonghua Bing Li Xue Za Zhi. 1994 Apr;23(2):104–106. [PubMed] [Google Scholar]