Abstract
Aims—Classic erythroleukaemia (acute myeloid leukaemia M6, or M6 AML) is defined as an excess of myeloblasts in an erythroid predominant background. Leukaemia variants in which the primitive blast cells are demonstrably erythroid are extremely rare and poorly characterised. Variably referred to as "true erythroleukaemia" or "acute erythremic myelosis", they are often included within the M6 AML category even though they do not meet strict criteria for this type of AML.
Methods— Two cases of acute erythroid neoplasia are presented with clinical, morphological, immunophenotypic, and cytogenetic analysis.
Results—Both patients presented with profound anaemia, one in a setting of long standing myelodysplasia. Bone marrow examination revealed a predominant population of highly dysplastic erythroid cells in both cases. In one case, the liver was infiltrated by neoplastic erythroid cells. Both patients died within four months of diagnosis.
Conclusions—This report illustrates that cases of acute leukaemia occur in which the dominant neoplastic cell is a primitive erythroid cell without an accompanying increase in myeloblasts. This does not preclude the neoplastic clone originating in a multipotent haemopoietic stem cell, as suggested by cases arising in patients with myelodysplasia. Acute erythremic myelosis should be recognised as a distinct variant of M6 AML.
Key Words: erythroleukaemia • erythremic myelosis • Di Guglielmo • acute leukaemia
Full Text
The Full Text of this article is available as a PDF (211.2 KB).
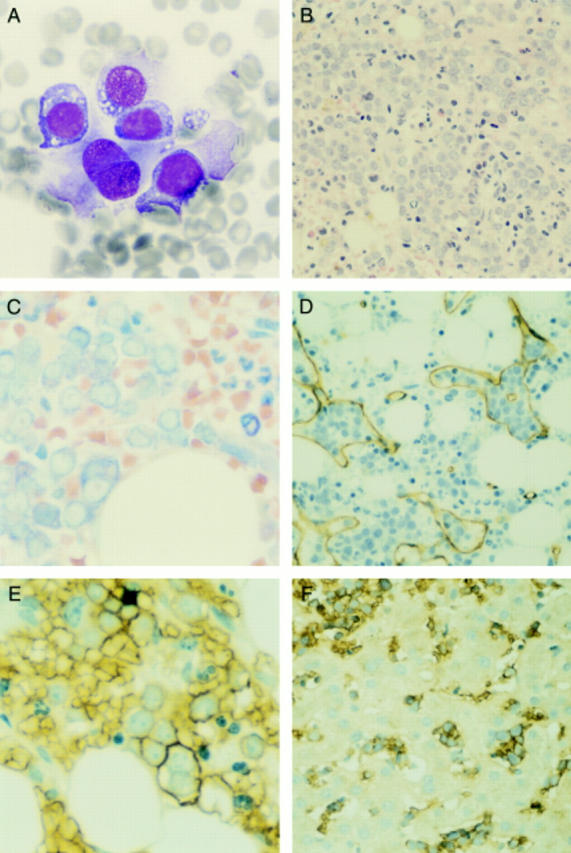
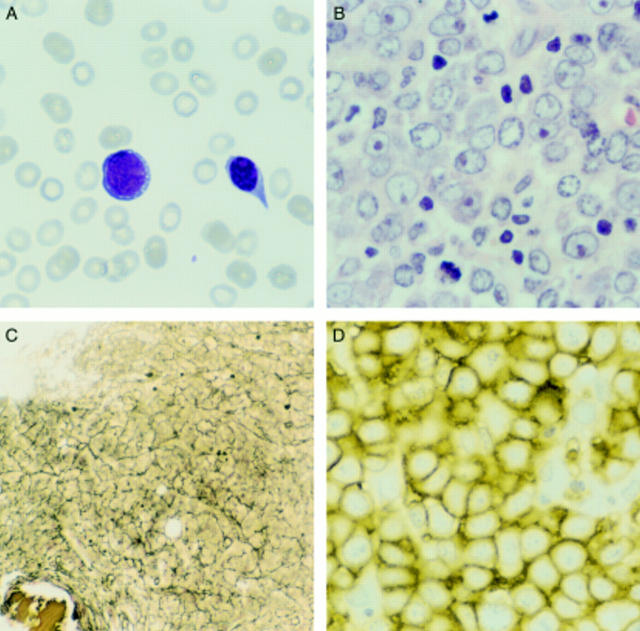
Figure 1 Case 1. (A) Bone marrow aspirate smear showing large primitive cells with vacuolated cytoplasm. (B) The primitive cells comprise about 80% of the cells of the bone marrow biopsy section, but interspersed maturing myeloid forms are also present (haematoxylin and eosin stained). (C) The primitive cells have basophilic, vacuolated cytoplasm on Giemsa stain; note the maturing myeloid forms in the upper right section. (D) The primitive forms cluster within bone marrow sinuses, as shown by the CD34 immunohistochemical stain highlighting endothelial cells. (E) The immature cells are immunoreactive for ß-sialoglycoprotein; note one binucleate erythroblast. (F) A liver biopsy shows similar cells, immunoreactive for ß-sialoglycoprotein, within hepatic sinusoids.
Figure 2 Case 2. (A) Peripheral blood smear showing an immature cell with basophilic vacuolated cytoplasm and a nucleated erythroid cell. (B) Bone marrow biopsy section showing sheets of large cells with vesicular nuclei and prominent nucleoli (haematoxylin and eosin stained). (C) The marrow shows greatly increased reticulin deposition (Gordon and Sweet's silver stain). (D) The immature cells are uniformly immunoreactive for glycophorin C.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bennett J. M., Catovsky D., Daniel M. T., Flandrin G., Galton D. A., Gralnick H. R., Sultan C. Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med. 1985 Oct;103(4):620–625. doi: 10.7326/0003-4819-103-4-620. [DOI] [PubMed] [Google Scholar]
- Forni M., Meyer P. R., Levy N. B., Lukes R. J., Taylor C. R. An immunohistochemical study of hemoglobin A, hemoglobin F, muramidase, and transferrin in erythroid hyperplasia and neoplasia. Am J Clin Pathol. 1983 Aug;80(2):145–151. doi: 10.1093/ajcp/80.2.145. [DOI] [PubMed] [Google Scholar]
- Garand R., Duchayne E., Blanchard D., Robillard N., Kuhlein E., Fenneteau O., Salomon-Nguyen F., Grange M. J., Rousselot P., Demur C. Minimally differentiated erythroleukaemia (AML M6 'variant'): a rare subset of AML distinct from AML M6. Groupe Français d'Hématologie Cellulaire. Br J Haematol. 1995 Aug;90(4):868–875. doi: 10.1111/j.1365-2141.1995.tb05208.x. [DOI] [PubMed] [Google Scholar]
- Gatter K. C., Cordell J. L., Turley H., Heryet A., Kieffer N., Anstee D. J., Mason D. Y. The immunohistological detection of platelets, megakaryocytes and thrombi in routinely processed specimens. Histopathology. 1988 Sep;13(3):257–267. doi: 10.1111/j.1365-2559.1988.tb02037.x. [DOI] [PubMed] [Google Scholar]
- Griesser G. H., Horny H. P. Hematopathological features of acute erythremia (morbus Di Guglielmo). A contribution to the classification and differential diagnosis of erythroid neoplasias. Acta Haematol. 1987;77(4):193–197. doi: 10.1159/000205994. [DOI] [PubMed] [Google Scholar]
- Kass L. Cytochemical abnormalities of atypical erythroblasts in acute erythremic myelosis. Acta Haematol. 1975;54(6):321–327. doi: 10.1159/000208093. [DOI] [PubMed] [Google Scholar]
- Kowal-Vern A., Cotelingam J., Schumacher H. R. The prognostic significance of proerythroblasts in acute erythroleukemia. Am J Clin Pathol. 1992 Jul;98(1):34–40. doi: 10.1093/ajcp/98.1.34. [DOI] [PubMed] [Google Scholar]
- Mazzella F. M., Kowal-Vern A., Shrit M. A., Wibowo A. L., Rector J. T., Cotelingam J. D., Collier J., Mikhael A., Cualing H., Schumacher H. R. Acute erythroleukemia: evaluation of 48 cases with reference to classification, cell proliferation, cytogenetics, and prognosis. Am J Clin Pathol. 1998 Nov;110(5):590–598. doi: 10.1093/ajcp/110.5.590. [DOI] [PubMed] [Google Scholar]
- Michiels J. J. Erythroleukemia and myelodysplastic syndromes: an historical appraisal and a personal view. Leuk Lymphoma. 1993 Jan;9(1-2):27–34. doi: 10.3109/10428199309148500. [DOI] [PubMed] [Google Scholar]
- Mirchandani I., Palutke M., Dutcher T. F., Bishop C. R. The value of immunoperoxidase studies in the diagnosis of 2 cases of acute leukaemia. Scand J Haematol. 1983 Mar;30(3):207–210. doi: 10.1111/j.1600-0609.1983.tb01474.x. [DOI] [PubMed] [Google Scholar]
- Reiffers J., Bernard P., Larrue J., Dachary D., David B., Boisseau M., Broustet A. Acute erythroblastic leukemia presenting as acute undifferentiated leukemia: a report of two cases with ultrastructural features. Leuk Res. 1985;9(3):413–420. doi: 10.1016/0145-2126(85)90064-5. [DOI] [PubMed] [Google Scholar]
- Roggli V. L., Saleem A. Erythroleukemia: a study of 15 cases and literature review. Cancer. 1982 Jan 1;49(1):101–108. doi: 10.1002/1097-0142(19820101)49:1<101::aid-cncr2820490121>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Ruvidić R., Pavlović-Kentera V., Bosković D., Biljanović-Paunović L., Mijović A., Jovanović V. Acute erythremic myelosis (DiGuglielmo) following atypical aplastic anemia. Leuk Res. 1986;10(4):451–455. doi: 10.1016/0145-2126(86)90076-7. [DOI] [PubMed] [Google Scholar]
- SCHWARTZ S. O., CRITCHLOW J. Erythremic myelosis (Dl Guglielmo's disease); critical review with report of four cases, and comments on erythroleukemia. Blood. 1952 Aug;7(8):765–793. [PubMed] [Google Scholar]
- Tsuji M., Tamai M., Terada N., Tako H. Anerythremic form of acute erythremic myelosis (Di Guglielmo's syndrome) causing hepatosplenomegaly due to the infiltration of hemoglobin-bearing blast cells: an autopsy case. Pathol Int. 1995 Apr;45(4):310–314. doi: 10.1111/j.1440-1827.1995.tb03462.x. [DOI] [PubMed] [Google Scholar]