Abstract
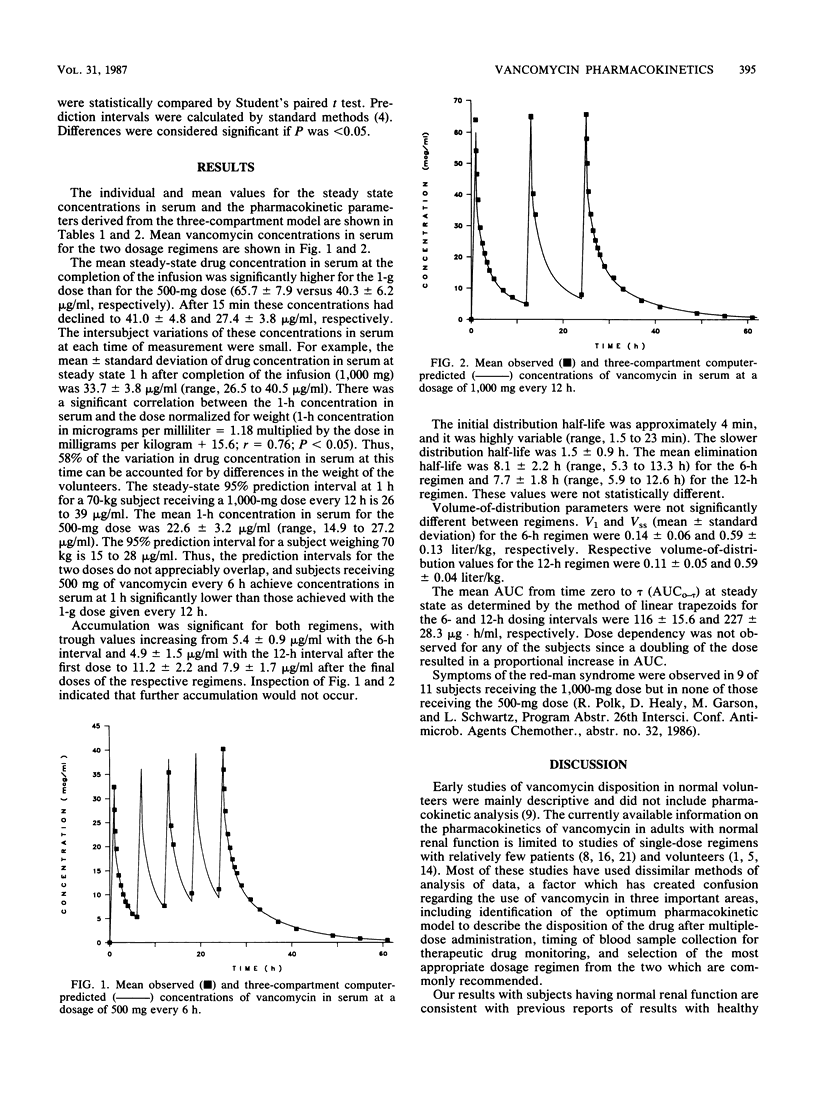
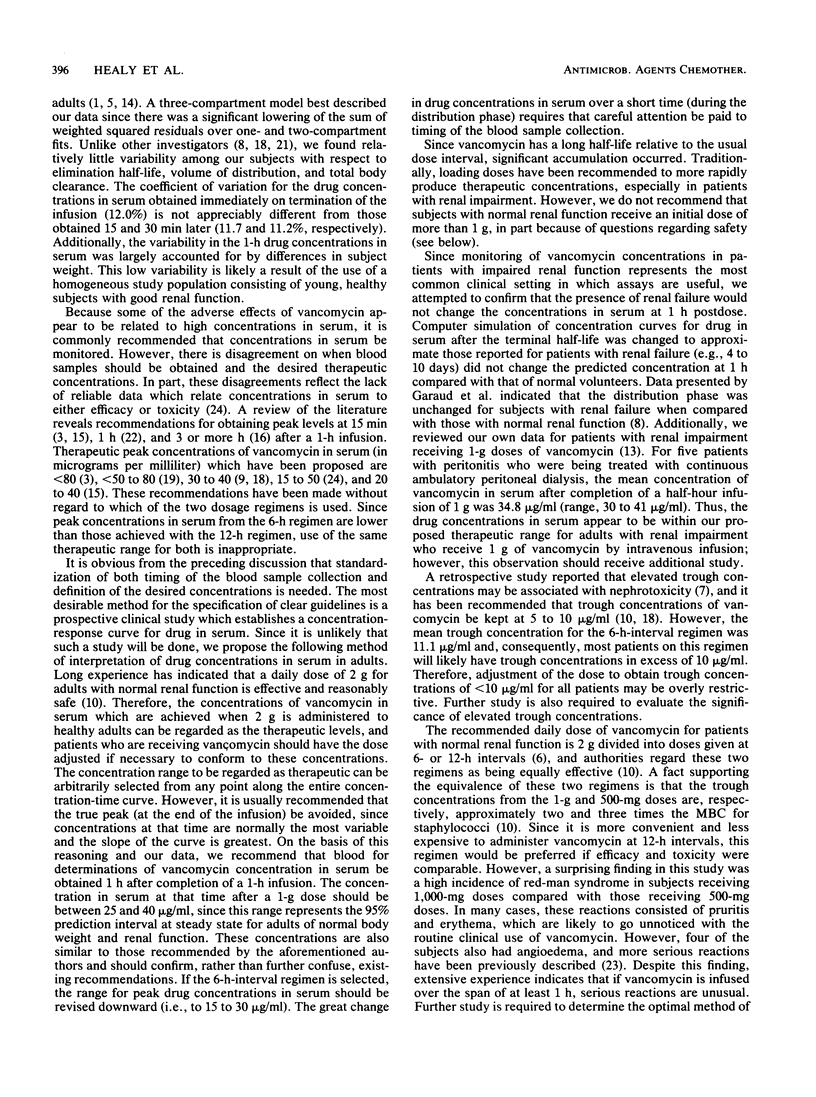
A pharmacokinetic comparison of the two recommended dosages of vancomycin given as multiple doses has not been previously performed. Eleven adult subjects with normal renal function randomly received 500 mg every 6 h (five doses) and, later, 1,000 mg every 12 h (three doses). Each dose was infused over 1 h, and regimens were separated by 1 week. Compared with the two-compartment fit, a three-compartment fit significantly reduced the residual weighted sums of squares. Accumulation occurred for both regimens after repeated dosing and was independent of dose. At steady state, concentrations in serum at 1 h showed little variation for the 1,000- or the 500-mg dose regimen (33.7 +/- 3.8 versus 22.6 +/- 3.2 micrograms/ml); trough concentrations were 7.9 +/- 1.7 versus 11.2 +/- 2.2 micrograms/ml, respectively. With the 1,000-mg dose, the terminal half-life was 7.7 +/- 1.8 h, steady-state area under the curve for the dose interval was 227 +/- 28.3 micrograms X h/ml, and total body clearance was 86.1 +/- 8.9 ml/min per 1.73 m2. The red-man syndrome occurred in 9 of 11 volunteers who received 1,000-mg doses and in none of those who received 500-mg doses. We concluded that vancomycin disposition in healthy adults with normal renal function is best described by a three-compartment model, there is relatively little variation in vancomycin disposition in normal volunteers, significant accumulation occurs with multiple dosing, it is inappropriate to use the same therapeutic window for both regimens, and the pharmacokinetics of vancomycin justify a 12-h dose interval; however, a 1-g dose is associated with a significantly greater incidence of the red-man syndrome.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blouin R. A., Bauer L. A., Miller D. D., Record K. E., Griffen W. O., Jr Vancomycin pharmacokinetics in normal and morbidly obese subjects. Antimicrob Agents Chemother. 1982 Apr;21(4):575–580. doi: 10.1128/aac.21.4.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R. D., Manno J. E. ESTRIP, a BASIC computer program for obtaining initial polyexponential parameter estimates. J Pharm Sci. 1978 Dec;67(12):1687–1691. doi: 10.1002/jps.2600671214. [DOI] [PubMed] [Google Scholar]
- Cheung R. P., DiPiro J. T. Vancomycin: an update. Pharmacotherapy. 1986 Jul-Aug;6(4):153–169. doi: 10.1002/j.1875-9114.1986.tb03471.x. [DOI] [PubMed] [Google Scholar]
- Cutler N. R., Narang P. K., Lesko L. J., Ninos M., Power M. Vancomycin disposition: the importance of age. Clin Pharmacol Ther. 1984 Dec;36(6):803–810. doi: 10.1038/clpt.1984.260. [DOI] [PubMed] [Google Scholar]
- Farber B. F., Moellering R. C., Jr Retrospective study of the toxicity of preparations of vancomycin from 1974 to 1981. Antimicrob Agents Chemother. 1983 Jan;23(1):138–141. doi: 10.1128/aac.23.1.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GERACI J. E., HEILMAN F. R., NICHOLS D. R., ROSS G. T., WELLMAN W. E. Some laboratory and clinical experiences with a new antibiotic, vancomycin. Proc Staff Meet Mayo Clin. 1956 Oct 17;31(21):564–582. [PubMed] [Google Scholar]
- Garaud J. J., Regnier B., Inglebert F., Faurisson F., Bauchet J., Vachon F. Vancomycin pharmacokinetics in critically ill patients. J Antimicrob Chemother. 1984 Dec;14 (Suppl 500):53–57. doi: 10.1093/jac/14.suppl_d.53. [DOI] [PubMed] [Google Scholar]
- Geraci J. E., Hermans P. E. Vancomycin. Mayo Clin Proc. 1983 Feb;58(2):88–91. [PubMed] [Google Scholar]
- Harford A. M., Sica D. A., Tartaglione T., Polk R. E., Dalton H. P., Poynor W. Vancomycin pharmacokinetics in continuous ambulatory peritoneal dialysis patients with peritonitis. Nephron. 1986;43(3):217–222. doi: 10.1159/000183833. [DOI] [PubMed] [Google Scholar]
- Krogstad D. J., Moellering R. C., Jr, Greenblatt D. J. Single-dose kinetics of intravenous vancomycin. J Clin Pharmacol. 1980 Apr;20(4 Pt 1):197–201. doi: 10.1002/j.1552-4604.1980.tb01696.x. [DOI] [PubMed] [Google Scholar]
- Lake K. D., Peterson C. D. A simplified dosing method for initiating vancomycin therapy. Pharmacotherapy. 1985 Nov-Dec;5(6):340–344. doi: 10.1002/j.1875-9114.1985.tb03441.x. [DOI] [PubMed] [Google Scholar]
- Matzke G. R., McGory R. W., Halstenson C. E., Keane W. F. Pharmacokinetics of vancomycin in patients with various degrees of renal function. Antimicrob Agents Chemother. 1984 Apr;25(4):433–437. doi: 10.1128/aac.25.4.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moellering R. C., Jr, Krogstad D. J., Greenblatt D. J. Vancomycin therapy in patients with impaired renal function: a nomogram for dosage. Ann Intern Med. 1981 Mar;94(3):343–346. doi: 10.7326/0003-4819-94-3-343. [DOI] [PubMed] [Google Scholar]
- Moellering R. C., Jr Pharmacokinetics of vancomycin. J Antimicrob Chemother. 1984 Dec;14 (Suppl 500):43–52. doi: 10.1093/jac/14.suppl_d.43. [DOI] [PubMed] [Google Scholar]
- Pfaller M. A., Krogstad D. J., Granich G. G., Murray P. R. Laboratory evaluation of five assay methods for vancomycin: bioassay, high-pressure liquid chromatography, fluorescence polarization immunoassay, radioimmunoassay, and fluorescence immunoassay. J Clin Microbiol. 1984 Sep;20(3):311–316. doi: 10.1128/jcm.20.3.311-316.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotschafer J. C., Crossley K., Zaske D. E., Mead K., Sawchuk R. J., Solem L. D. Pharmacokinetics of vancomycin: observations in 28 patients and dosage recommendations. Antimicrob Agents Chemother. 1982 Sep;22(3):391–394. doi: 10.1128/aac.22.3.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rybak M. J., Boike S. C. Monitoring vancomycin therapy. Drug Intell Clin Pharm. 1986 Oct;20(10):757–761. doi: 10.1177/106002808602001003. [DOI] [PubMed] [Google Scholar]
- Southorn P. A., Plevak D. J., Wright A. J., Wilson W. R. Adverse effects of vancomycin administered in the perioperative period. Mayo Clin Proc. 1986 Sep;61(9):721–724. doi: 10.1016/s0025-6196(12)62773-6. [DOI] [PubMed] [Google Scholar]
- Wenk M., Vozeh S., Follath F. Serum level monitoring of antibacterial drugs. A review. Clin Pharmacokinet. 1984 Nov-Dec;9(6):475–492. doi: 10.2165/00003088-198409060-00001. [DOI] [PubMed] [Google Scholar]



