Abstract
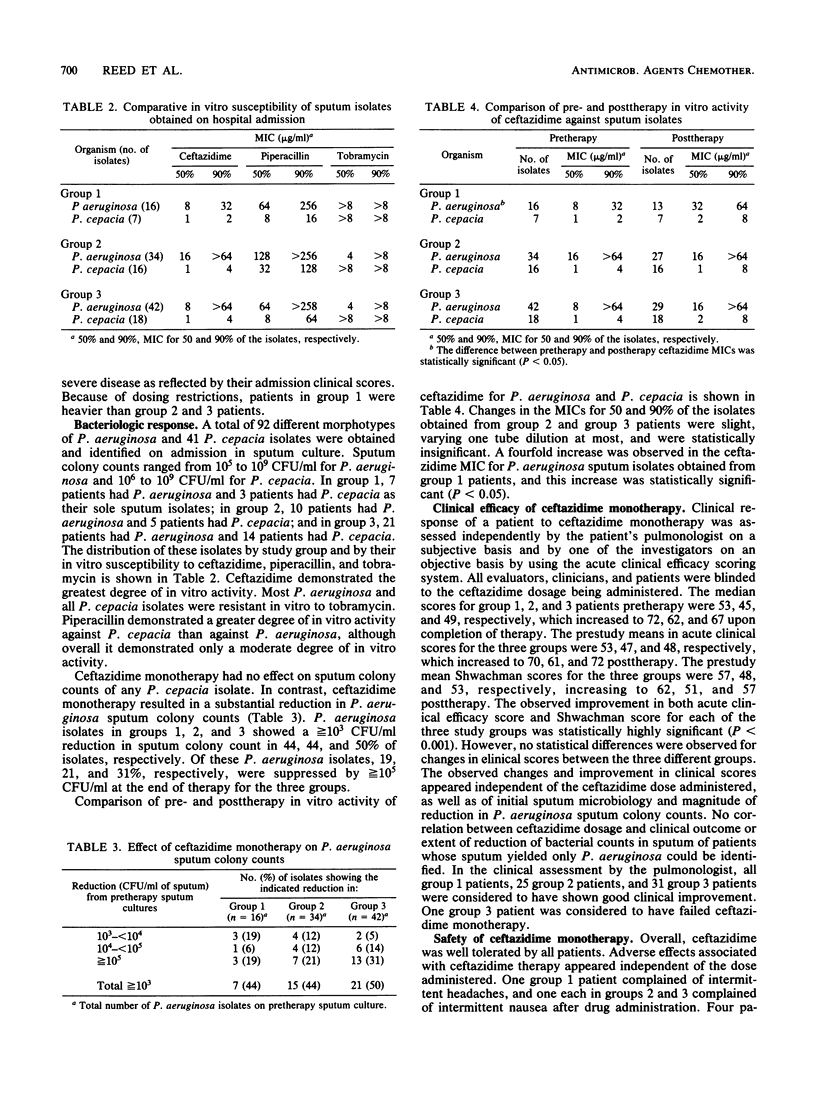
Eighty-five patients with cystic fibrosis who were experiencing an acute infectious exacerbation of their disease were randomized in double-blind fashion to receive either 50 or 75 mg of ceftazidime per kg (body weight) per dose administered intravenously every 8 h for 14 days. Three patients were dropped from the study within 4 days of enrollment for reasons unrelated to drug administration. The total daily dose of ceftazidime administered was restricted by protocol design and was independent of the body weight of the patient. Thus, for datum analysis, patients were separated into three ceftazidime dosage groups (denoted as range of milligrams per kilogram per dose): group 1, 22 to 44.5; group 2, 46.3 to 56.6; and group 3, 66.7 to 80.6. Ceftazidime monotherapy had no effect on sputum colony counts for any Pseudomonas cepacia isolate. In contrast, a substantial reduction in Pseudomonas aeruginosa sputum colony counts was observed, and from 19 to 31% of isolates were suppressed greater than or equal to 10(5) CFU/ml after 14 days of therapy. Bacterial resistance in vitro was not observed, although a trend for increasing ceftazidime MICs was observed for group 1 patients (P less than 0.05). Overall, clinical response appeared independent of drug dose, and no relationship could be identified between the reduction in P. aeruginosa sputum colony counts and clinical outcome. Adverse effects of ceftazidime were mild and transient, necessitating drug discontinuation in one patient. These data suggest that the clinical response to ceftazidime in patients with cystic fibrosis may be maximal with 50 mg/kg per dose (150 mg/kg per day) up to a total daily dose of 6 g.
Full text
PDF



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aronoff S. C., Klinger J. D. Comparison of cefpiramide (HR-810) and four anti-pseudomonal beta-lactam agents against pseudomonas isolates from children with cystic fibrosis. J Antimicrob Chemother. 1985 May;15(5):545–549. doi: 10.1093/jac/15.5.545. [DOI] [PubMed] [Google Scholar]
- Blumer J. L., Stern R. C., Klinger J. D., Yamashita T. S., Meyers C. M., Blum A., Reed M. D. Ceftazidime therapy in patients with cystic fibrosis and multiply-drug-resistant pseudomonas. Am J Med. 1985 Aug 9;79(2A):37–46. doi: 10.1016/0002-9343(85)90259-1. [DOI] [PubMed] [Google Scholar]
- Gold R., Overmeyer A., Knie B., Fleming P. C., Levison H. Controlled trial of ceftazidime vs. ticarcillin and tobramycin in the treatment of acute respiratory exacerbations in patients with cystic fibrosis. Pediatr Infect Dis. 1985 Mar-Apr;4(2):172–177. doi: 10.1097/00006454-198503000-00012. [DOI] [PubMed] [Google Scholar]
- Goldmann D. A., Klinger J. D. Pseudomonas cepacia: biology, mechanisms of virulence, epidemiology. J Pediatr. 1986 May;108(5 Pt 2):806–812. doi: 10.1016/s0022-3476(86)80749-1. [DOI] [PubMed] [Google Scholar]
- Kercsmar C. M., Stern R. C., Reed M. D., Myers C. M., Murdell D., Blumer J. L. Ceftazidime in cystic fibrosis: pharmacokinetics and therapeutic response. J Antimicrob Chemother. 1983 Jul;12 (Suppl A):289–295. doi: 10.1093/jac/12.suppl_a.289. [DOI] [PubMed] [Google Scholar]
- Klinger J. D., Thomassen M. J. Occurrence and antimicrobial susceptibility of gram-negative nonfermentative bacilli in cystic fibrosis patients. Diagn Microbiol Infect Dis. 1985 Mar;3(2):149–158. doi: 10.1016/0732-8893(85)90025-2. [DOI] [PubMed] [Google Scholar]
- Leeder J. S., Spino M., Isles A. F., Tesoro A. M., Gold R., MacLeod S. M. Ceftazidime disposition in acute and stable cystic fibrosis. Clin Pharmacol Ther. 1984 Sep;36(3):355–362. doi: 10.1038/clpt.1984.187. [DOI] [PubMed] [Google Scholar]
- Levy J., Smith A. L., Koup J. R., Williams-Warren J., Ramsey B. Disposition of tobramycin in patients with cystic fibrosis: a prospective controlled study. J Pediatr. 1984 Jul;105(1):117–124. doi: 10.1016/s0022-3476(84)80375-3. [DOI] [PubMed] [Google Scholar]
- McLaughlin F. J., Matthews W. J., Jr, Strieder D. J., Sullivan B., Taneja A., Murphy P., Goldmann D. A. Clinical and bacteriological responses to three antibiotic regimens for acute exacerbations of cystic fibrosis: ticarcillin-tobramycin, azlocillin-tobramycin, and azlocillin-placebo. J Infect Dis. 1983 Mar;147(3):559–567. doi: 10.1093/infdis/147.3.559. [DOI] [PubMed] [Google Scholar]
- Padoan R., Brienza A., Crossignani R. M., Lodi G., Giunta A., Assael B. M., Granata F., Passarella E., Vallaperta P. A., Xerri L. Ceftazidime in treatment of acute pulmonary exacerbations in patients with cystic fibrosis. J Pediatr. 1983 Aug;103(2):320–324. doi: 10.1016/s0022-3476(83)80377-1. [DOI] [PubMed] [Google Scholar]
- Reed M. D., Stern R. C., Bertino J. S., Jr, Myers C. M., Yamashita T. S., Blumer J. L. Dosing implications of rapid elimination of trimethoprim-sulfamethoxazole in patients with cystic fibrosis. J Pediatr. 1984 Feb;104(2):303–307. doi: 10.1016/s0022-3476(84)81019-7. [DOI] [PubMed] [Google Scholar]
- SHWACHMAN H., KULCZYCKI L. L. Long-term study of one hundred five patients with cystic fibrosis; studies made over a five- to fourteen-year period. AMA J Dis Child. 1958 Jul;96(1):6–15. doi: 10.1001/archpedi.1958.02060060008002. [DOI] [PubMed] [Google Scholar]
- Stephens D., Garey N., Isles A., Levison H., Gold R. Efficacy of inhaled tobramycin in the treatment of pulmonary exacerbations in children with cystic fibrosis. Pediatr Infect Dis. 1983 May-Jun;2(3):209–211. doi: 10.1097/00006454-198305000-00007. [DOI] [PubMed] [Google Scholar]
- Tablan O. C., Chorba T. L., Schidlow D. V., White J. W., Hardy K. A., Gilligan P. H., Morgan W. M., Carson L. A., Martone W. J., Jason J. M. Pseudomonas cepacia colonization in patients with cystic fibrosis: risk factors and clinical outcome. J Pediatr. 1985 Sep;107(3):382–387. doi: 10.1016/s0022-3476(85)80511-4. [DOI] [PubMed] [Google Scholar]
- Yaffe S. J., Gerbracht L. M., Mosovich L. L., Mattar M. E., Danish M., Jusko W. J. Pharmacokinetics of methicillin in patients with cystic fibrosis. J Infect Dis. 1977 May;135(5):828–831. doi: 10.1093/infdis/135.5.828. [DOI] [PubMed] [Google Scholar]



