Abstract
Context: Improving postural stability through balance training may prevent ankle sprains. Exercise Sandals may increase the demands placed on ankle muscles during rehabilitation, which could improve postural stability.
Objective: To examine the effects of functional balance training, with and without the use of Exercise Sandals, on postural stability in subjects with stable or unstable ankles.
Design: Prospective, nonrandomized clinical trial.
Setting: Sports medicine research laboratory.
Patients or Other Participants: Sixteen subjects with functional ankle instability and 16 subjects with no history of ankle sprains.
Intervention(s): Subjects were assigned to an Exercise Sandal functional balance training group or a shoe functional balance training group. Subjects trained 3 times per week for 8 weeks and then performed a single-limb stance posttest.
Main Outcome Measure(s): Subjects were required to remain as motionless as possible during a single-limb stance pretest. Anterior-posterior and medial-lateral center-of-pressure excursions were measured.
Results: Exercise Sandal balance training improved anterior-posterior postural stability in both ankle groups ( P < .05). Both training interventions improved medial-lateral postural stability in stable and unstable ankles ( P < .05).
Conclusions: Postural stability improved after subjects performed functional balance training programs, both with and without Exercise Sandals. Training with Exercise Sandals might not be any more effective in improving postural stability than performing functional balance training without Exercise Sandals. However, Exercise Sandals did not impair postural stability and, consequently, might serve as an alternative therapy to improve postural stability.
Keywords: balance shoes, chronic ankle instability, functional ankle instability
Participation in athletics often leads to increased susceptibility to ankle sprains, and injuries that persist can lead to repeated ankle sprains. 1–5 One such chronic injury is known as functional ankle instability (FAI), which is characterized by sensations of “giving way” at the ankle and recurrent ankle sprains. 2 Researchers 2, 6–16 have speculated that neuromuscular deficits associated with FAI might be responsible for impairing postural stability. Poor postural stability has also been reported to predispose physically active individuals to ankle sprains. 17, 18 As a result of this association between postural stability and incidence of ankle sprain, rehabilitation focused on improving postural stability in physically active individuals with and without FAI might be important in preventing ankle sprains.
Rehabilitation programs emphasizing coordination, balance, and strength training have been recommended for improving ankle stability and postural stability in subjects with both stable and unstable ankles. * Ankle rehabilitation exercises are typically performed in a static position rather than a dynamic balance position. † Proprioceptive and postural stability exercises, for example, are performed in a single-limb stance position, and strengthening exercises are usually performed in an open chain mode. Other coordination and balance training programs have included functional exercises in addition to the more traditional exercises performed in a static position. 4, 6, 8, 19, 24, 27 Although most coordination and balance training programs have effectively improved postural stability ‡ and decreased the incidence of ankle sprains, 4, 8, 25, 27, 29 our research group has recently recommended using Exercise Sandals (Orthopedic Physical Therapy Products, Minneapolis, MN) to increase the difficulty of balance exercises and to improve ankle muscle activation. 30
Exercise Sandals are corked, rubber-soled sandals with a hemisphere attached to the midsole ( Figure 1). The design of the sandal creates a perturbation device, allowing individuals to perform exercises on wobble board platforms. Exercise Sandals essentially transform static balance exercises into dynamic balance exercises and increase the difficulty of dynamic balance exercises that are typically performed on a stable surface. 30 In addition, training in Exercise Sandals requires athletes to perform the short-foot maneuver, which allows the intrinsic foot flexors to contract in the absence of toe flexion. 30 Performing ankle rehabilitation exercises with the use of Exercise Sandals has been reported to increase ankle muscle activity compared with performing rehabilitation exercises without the use of Exercise Sandals. 30
Figure 1. Exercise Sandals. Exercise Sandals are corked sandals with rubber soles and perturbation devices attached to the bottom.
Although Exercise Sandals might increase the difficulty of exercises, the effects of these sandals on postural stability have not been studied. In theory, Exercise Sandals might increase the demands placed on ankle muscles with balance exercises, which could lead to postural stability improvements. Improving postural stability with the use of Exercise Sandals during rehabilitation might have implications for preventing ankle sprains in healthy individuals and in individuals with FAI. Therefore, our purpose was to examine the potential effects of balance training with or without Exercise Sandals on anterior-posterior (A-P) and medial-lateral (M-L) center-of-pressure excursion (COPE) during single-limb stance in subjects with FAI and subjects with stable ankles.
METHODS
Subjects
Subject characteristics are reported in Table 1. Thirty-two individuals (16 females and 16 males) who participated in a minimum of 2 hours of physical activity per week served as subjects. Sixteen subjects with FAI reported multiple “giving way” sensations at the ankle with physical activity, and they had sustained at least 2 ankle sprains in the year before the study. We did not quantify mechanical instability in our subjects. Ankle stability of subjects with FAI, however, was quantified with the Ankle Joint Functional Assessment Tool. This questionnaire has been used previously to quantify self-reported ankle stability. 14, 28, 31 However, the validity and reliability of this questionnaire have not been established. Subjects with FAI all scored less than 20 points out of a maximum 48 points (higher scores indicate greater stability). Previous authors 14, 28, 31 indicated that subjects with FAI scored less than 20 on the tool. Potential subjects with FAI were excluded if they scored more than 20 points on the tool. Potential subjects were also excluded if they had experienced an ankle sprain within the 6 months prior to this study. However, subjects participating in this study still experienced “giving way” sensations after the 6-month cutoff period for ankle sprains.
Table 1. Subject Characteristics (Mean ± SD).
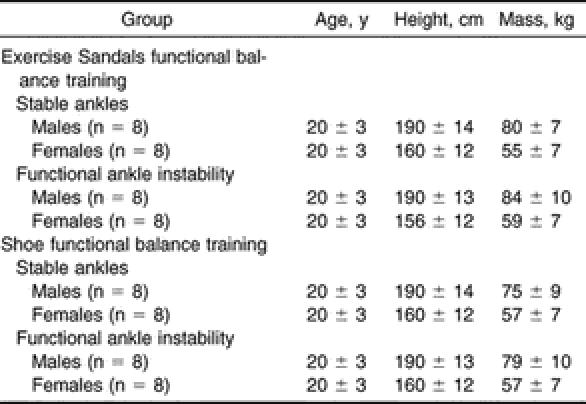
Subjects with stable ankles were matched with 16 subjects with FAI by age, height, weight, sex, and test limb. The test limb was defined as the limb with FAI for subjects in the FAI group. In the case of bilateral FAI, the ankle scoring lower on the Ankle Joint Functional Assessment Tool was used for testing. Subjects' test limbs were then defined as dominant (preferred limb used to kick a ball) or nondominant (preferred limb used to stand on while kicking a ball). The same limb (dominant or nondominant) was tested in subjects with stable ankles and in their matched counterparts. Our 16 subjects with stable ankles did not have a history of ankle sprain injury, and they did not report “giving way” sensations at their ankle joints. Additional exclusion criteria for all subjects included a history of lower extremity fracture, knee injury, or hip injury; visual impairment that affected balance; vestibular deficit; or neurologic dysfunction. Subjects received a test protocol orientation, and they read and signed a consent form that was approved by The Committee for the Protection of the Rights of Human Subjects, which also approved the study.
Subjects with FAI were randomly assigned to an Exercise Sandal functional balance training (EFBT) group or shoe functional balance training (SFBT) group. However, subjects with stable ankles were not randomly assigned to a training group but rather to the same group as their matched counterparts with FAI. Sixteen subjects were in the EFBT group (8 subjects with stable ankles and 8 subjects with FAI) and wore Exercise Sandals during the 8-week functional balance training program. Sixteen subjects were in the SFBT group (8 subjects with stable ankles and 8 subjects with FAI), and they also participated in 8 weeks of functional balance training. However, they wore athletic shoes.
Functional Balance Training
During the 8 weeks of functional balance training, subjects were required to perform exercises in an athletic training facility under the supervision of the principal investigator, a certified athletic trainer (T.B.M.). Subjects trained both extremities 3 times per week for 8 weeks using functional exercises developed from an ankle rehabilitation protocol that we used in our athletic training facility. The protocol was similar, in terms of the number of training sessions and weeks of training, to those reported in the literature. 2, 4, 6, 8, 10–15, 19–26 All subjects performed a short-foot maneuver during training sessions. This position has been described by Janda and Va'Vrova, 32 and it essentially requires a shortening of the A-P plane of the foot and a narrowing of the M-L plane of the foot. The SFBT and EFBT groups performed the short-foot maneuver in athletic shoes and Exercise Sandals with functional balance exercises, respectively. The principal investigator corrected subjects when exercises were not performed correctly. In addition, subjects reported that they could feel their muscles working to shorten and narrow the foot during all exercises.
Exercises performed in our functional balance training program by both training groups included the following: (1) Achilles stretching, (2) short-foot concept contractions, (3) high knee walking, (4) lateral side step, (5) walking exercises (forward and backward), (6) lunges, and (7) squats. Subjects performed 3 sets with 5 repetitions for each limb for high knee walking, lateral side steps, walking exercises, lunges, and squats during the first training session. Thereafter, subjects performed 5 sets with 8 repetitions for all training sessions. All training sessions began and ended with Achilles stretching. This stretching required subjects to place the foot on a 30° slant board and stretch the Achilles with the knee straight for 3 sets × 20 seconds and then stretch with the knee bent for 3 sets × 20 seconds. The stretching protocol did not change throughout the 8 weeks of training. Subjects did not wear sandals or shoes during Achilles stretching. Subjects then practiced the short-foot maneuver before performing functional balance training exercises. The short-foot position was achieved 3 times, and each contraction was held for 60 seconds. During these contractions, subjects were instructed to pull the arch of the foot up by shortening the length and narrowing the width of the foot without flexing the toes. Functional balance training exercises were then performed in the order presented in this report.
High Knee Walking
High knee walking exercises required subjects to flex the limb to approximately 70° of hip flexion and 90° of knee flexion, while simultaneously standing on the contralateral limb. After flexing, subjects returned the limb to a straightened position by taking a step out in front of the body. No restrictions were placed on subjects' stride length. Subjects then took a step forward with the stance limb, so that the limbs were shoulder width apart and parallel.
Lateral Side Steps
Lateral side step exercises required subjects to step laterally while staying in a defensive stance. Subjects lifted the foot slightly off the ground and quickly moved the limb laterally. No restrictions were placed on subjects' stride length. The contralateral limb was then moved medially to bring the limbs shoulder width apart.
Walking Exercises
Walking exercises required subjects to step forward while maintaining a defensive stance position. No restrictions were placed on subjects' stride length. Walking exercises were different than high knee exercises, as subjects did not flex their hips and knees to 70° and 90°, respectively. After stepping, subjects took a step forward with the contralateral limb so that the limbs were shoulder width apart and parallel. Subjects then repeated this exercise for each limb by walking backward.
Lunges
Lunges required subjects to perform a lateral side step while maintaining a defensive stance, as previously described. Subjects then flexed the limb that moved laterally to 70° of knee flexion and straightened the contralateral limb. The knee of the limb that moved laterally was then extended back to the original defensive-stance knee position as the contralateral limb was moved medially. The contralateral limb was moved medially to bring the limbs shoulder width apart and parallel.
Squats
The squat exercise again required subjects to perform a lateral side step and to maintain a defensive stance, as previously described. After stepping laterally, the contralateral limb was moved medially so that the limbs were approximately shoulder width apart and parallel. Subjects then performed a squat by flexing their knees to 70° of knee flexion. Knees were then extended back to the original defensive-stance knee positions.
Single-Limb Stance Test
All subjects wore gym clothing and were shoeless during the single-limb stance test. Subjects were instructed to remain as motionless as possible when standing with the test limb on the forceplate. Subjects kept their eyes open, their hands on their hips, and the non–weight-bearing limb in approximately 20° of hip flexion and 45° of knee flexion during the test. 31 The weight-bearing limb was in approximately 5° of knee flexion, and subjects placed the foot in a comfortable position. 31 One 10-second practice trial was followed by three 20-second testing trials. 31 Subjects repeated trials if they hopped on the weight-bearing limb or touched down with the non–weight-bearing limb. Subjects were instructed not to perform the short-foot maneuver during this single-limb stance test. Subjects performed single-limb pretests and then posttests after their 8 weeks of functional balance training. All subjects were tested within 72 hours of their final training session.
Data Collection
We used a Bertec forceplate (model 4060-08; Bertec Corp, Columbus, OH) amplifier (model AM-6701; Bertec Corp) and PEAK Performance Motus analog-to-digital interface unit (PEAK Performance Inc, Englewood, CO) to collect ground reaction force data. Forceplate analog signals were sampled at 180 Hz, amplified by a factor of 5, and converted to digital signals. 31 The MotionSoft MSFPLT computer program software package (version 2.0; MotionSoft, Inc, Chapel Hill, NC) converted digital signals to ground reaction force vectors, moments, and location of the center of pressure. Data were filtered using a Butterworth low-pass digital filter with an estimated optimum cutoff frequency of 12.53 Hz. 31 Anterior-posterior COPE and M-L COPE were calculated after filtering the data. Equations used to calculate center-of-pressure (COP) measures were as follows:
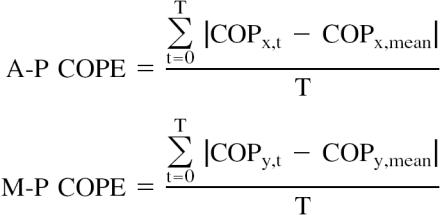 |
The COPE measures have been used previously to examine postural instabilities associated with ankle instabilities. 7, 9, 12, 24, 31 The type of COP measures used to quantify postural stability varies throughout the literature, 4, 6, 8, 10–15, 21, 24, 26 and we chose COPE to provide an overall analysis of stability. 7, 9, 12, 24, 31 Our pilot data collected on 18 subjects with FAI and 19 subjects with stable ankles indicated that COPE has moderate reliability (A-P COPE intraclass correlation coefficient [2,3] = 0.79; M-L COPE intraclass correlation coefficient [2,3] = 0.75) and high precision (A-P COPE SEM = 0.11 cm, M-L COPE SEM = 0.07 cm).
Statistical Analysis
We computed the average of 3 trials for the single-limb stance test for the pretest and posttest data. A series of 2 (test session: pretest, posttest) × 2 (training group: EFBT, SFBT) × 2 (ankle group: FAI, stable) repeated-measures analysis of variance tests were calculated for each dependent measure to detect significant differences between training groups. Post hoc analyses were performed using simple main effects. Effect size calculations were analyzed using the Cohen 33 effect size index (f) for 3-way interactions and significant 2-way interactions. Effect size calculations were analyzed using the Cohen 33 effect size index (d) for significant main effects related to our research questions and simple main effects post hoc analyses. Effect size index d was used for analyses that compared 2 means. Observed power (OP) was calculated for nonsignificant findings related to our research questions. All statistical analyses were performed using SPSS (version 13.0 for Windows; SPSS Inc, Chicago, IL). The alpha level was set a priori at .05 to indicate significance for all statistical tests.
RESULTS
Anterior-Posterior Center-of-Pressure Excursion
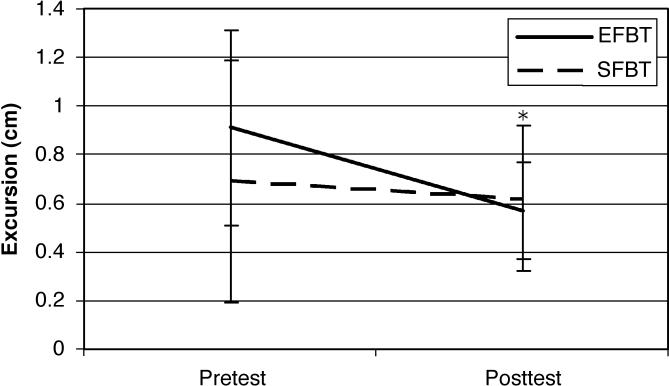
The means and standard deviations for A-P COPE are reported in Table 2. No significant test session × training group × ankle group interaction was found (F 1,28 = 3.20, P = .085, f = 0.40, OP = 0.40). A significant training group × test session interaction was noted (F 1,28 = 4.22, P = .049, f = 0.30; Figure 2). Posttest A-P COPE for the EFBT group was lower than the pretest score (F 1,28 = 13.25, P = .001; d = 0.74). No significant difference was present between pretest and posttest scores for the SFBT group (F 1,28 = 0.54, P = .469, d = 0.20, OP = 0.14). No differences between the groups' pretest scores (F 1,28 = 3.09, P = .084, d = 0.50, OP = 0.40) or posttest scores (F 1,28 = 0.19, P = .664, d = 0.10, OP = 0.09) were seen. A significant main effect for test session was found (F 1,28 = 9.57, P = .004, d = 0.40). The remaining main effects and 2-way interactions were not statistically significant ( P > .05).
Table 2. Center-of-Pressure Excursion (cm) (Mean ± SD).
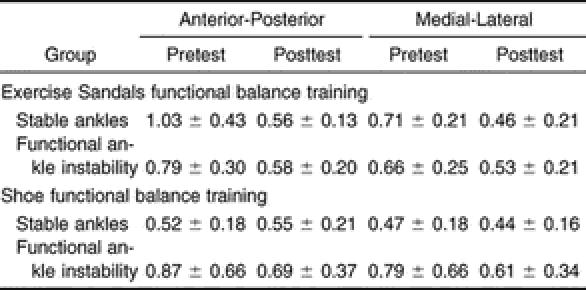
Figure 2. Anterior-posterior postural stability in subjects training with and without Exercise Sandals (training group × test session interaction). *Subjects training with Exercise Sandals decreased posttest anterior-posterior center-of-pressure excursion from their pretest values after 8 weeks of training. EFBT indicates Exercise Sandal functional balance group; SFBT, shoe functional balance training group.
Medial-Lateral Center-of-Pressure Excursion
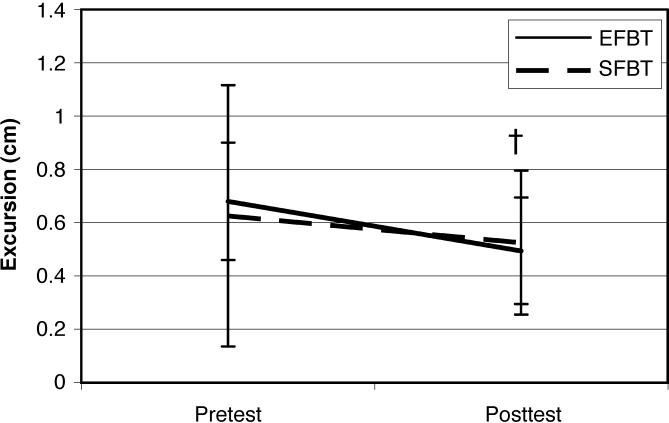
The means and standard deviations for M-L COPE are reported in Table 2. No test session × training group × ankle group interaction was found (F 1,28 = 1.90, P = .179, f = 0.35, OP = 0.31). Figure 3 displays the training group × test session interaction (F 1,28 = 0.76, P = .391, f = 0.25, OP = 0.28). A significant main effect for test session was noted (F 1,28 = 8.38, P = .007, d = 0.50), indicating that the posttest score was lower than the pretest score. The remaining main effects and 2-way interactions were not statistically significant ( P > .05).
Figure 3. Medial-lateral postural stability in subjects training with and without Exercise Sandals (training group × test session interaction). *Subjects training with or without Exercise Sandals decreased posttest medial-lateral center-of-pressure excursion from their pretest values after 8 weeks of training. EFBT indicates Exercise Sandal functional balance group; SFBT, shoe functional balance training group.
DISCUSSION
Our purpose was to examine the potential effects of functional balance training with and without Exercise Sandals on A-P and M-L COPE during single-limb stance in subjects with FAI and subjects with stable ankles. The most important finding of this study was that subjects training with or without Exercise Sandals improved postural stability after 8 weeks. Coordination and balance training have been reported to decrease ankle sprain incidence in individuals with and without FAI. 4, 8, 25, 27, 29 Therefore, our training protocol might have implications for decreasing ankle sprains in physically active individuals both with and without FAI.
Our results indicate that A-P COPE improved in subjects training with Exercise Sandals. However, low statistical power might have limited our ability to detect an additional statistically significant difference between the training groups at pretest. The effect size of the A-P COPE post hoc analysis indicates that the EFBT group had worse stability than the SFBT group at pretest. The effect size index d value for this analysis is considered moderate, and, consequently, significant F statistics might be expected with adequate statistical power. 33 In addition, the training groups' posttest A-P postural stability was not different, indicating that both groups completed training with similar A-P postural stability. Although Exercise Sandals were effective at improving A-P postural stability, 8 weeks of functional balance training with them did not result in improved performance compared with the same training without sandals. Furthermore, the difference between the groups at pretest is a potential limitation to the interpretation of our A-P postural stability results. Subjects with stable ankles were not randomly assigned to a training group, as they were assigned to the same group as their matched counterparts with FAI. This nonrandom assignment of subjects with stable ankles might have inadvertently assigned subjects with stable ankles and poor A-P postural stability to the EFBT group. Subjects training without Exercise Sandals might have reacted similarly to subjects training with Exercise Sandals if both training groups began the study with poor A-P postural stability.
Exercise Sandals have been reported to increase muscle activity of the tibialis anterior, soleus, peroneus longus, and gastrocnemius muscles during a variety of static and dynamic exercises. 30 Based on this previous finding, we speculate that training with Exercise Sandals increased muscle activation of the tibialis anterior, soleus, peroneus longus, and gastrocnemius, which might have improved A-P postural stability. However, we are currently unaware of research indicating that muscle activity increases after subjects remove their sandals upon completion of their training.
Our M-L postural stability results indicate that EFBT and SFBT groups improved their posttest M-L stability over pretest values. Both groups began this study with approximately the same M-L postural stability, and they reacted similarly to the functional balance training by improving M-L postural stability at the end of this study. This finding indicates that functional balance exercises are responsible for improving M-L postural stability. Additionally, this finding indicates that training with Exercise Sandals might not be any more effective in improving postural stability than performing functional balance training without Exercise Sandals.
The extent to which the short-foot technique contributed to postural stability improvements in our study is not known. Rothermel et al 26 reported that 4 weeks (12 sessions) of single-limb balance training with the short-foot maneuver did not improve single-limb postural stability in healthy subjects, whereas training without the use of the short-foot position did improve single-limb postural stability in healthy subjects. Rothermel et al 26 speculated that the short-foot technique might have caused their subjects to focus on muscle contractions instead of remaining as motionless as possible during single-limb stance tests. We had our subjects perform functional balance exercises while using the short-foot position for 24 sessions over 8 weeks, which might have allowed our subjects more time to learn new muscle activation patterns associated with this technique. In addition, our subjects were instructed not to shorten and narrow the arch of the foot during single-limb stance tests, allowing them to concentrate on remaining as motionless as possible during the tests. The design of our study did not allow us to determine the effectiveness of the short-foot maneuver, as our results indicate that the functional balance exercises were responsible for postural stability improvements. Future researchers should examine the contributions of the short-foot concept with functional balance training to improving postural stability.
Our subjects might have developed new long-term muscle activation patterns after functional balance training. Muscle activity has improved after coordination training with static and semidynamic exercises. 8, 23 Osborne et al 23 reported decreased onset latency of the tibialis anterior muscle after ankle disk training in subjects with FAI. In addition, Eils and Rosenbaum 8 suggested that coactivation of ankle muscles increased in subjects with FAI after coordination training. This improved coactivation might have been responsible for improving postural stability in Eils and Rosenbaum's 8 subjects with FAI. Based on the results of these aforementioned studies, we contend that A-P and M-L postural stability improvements might have resulted from improved foot and ankle muscle activity after 8 weeks of training. This improved muscle activation likely occurred while subjects were performing the exercises with the short-foot technique, as well as while subjects performed single-limb testing without the use of the short-foot position. Subjects might have increased activation in muscles responsible for performing the short-foot maneuver without actually shortening the A-P plane of the foot and narrowing the M-L plane of the foot during single-limb stance tests. Future researchers should examine the effects of training with and without Exercise Sandals on muscle activation and postural stability to confirm our contentions.
Investigators * have reported that coordination training programs for stable and unstable ankles improved postural stability. Based on previous coordination training reports, we expected postural stability to improve after 8 weeks of functional balance training in subjects with FAI and subjects with stable ankles. Our functional balance training with and without Exercise Sandals likely introduced new movements and muscle activation patterns to subjects and might have provided enough stimulus to improve M-L postural stability in all subjects and A-P postural stability in subjects training with Exercise Sandals. In addition, neither subjects with stable ankles nor those with FAI had previous experience performing these exercises with the short-foot position while wearing shoes or Exercise Sandals. All subjects, regardless of ankle stability, might have responded to functional balance training similarly as a result of being introduced to these new movements and muscle activations for the first time.
Future authors should examine the effects of this functional balance training, with and without Exercise Sandals, on dynamic postural stability. Dynamic postural stability improved in subjects with FAI following a standard balance training protocol. 28 We speculate that dynamic postural stability would improve after our functional balance training program, as the dynamic movement associated with our program might challenge the postural control system more than a standard coordination training program would. Furthermore, dynamic postural stability might be more sensitive to detecting potential differences between subjects training functionally with or without Exercise Sandals.
Balance training in stable and functionally unstable ankles might have implications for preventing ankle sprains in physically active individuals. 4, 8, 25, 27, 29 Our findings indicate that postural stability improved after performing functional exercises with and without Exercise Sandals over 8 weeks of training. Performing functional balance training with Exercise Sandals might not be any more effective in improving postural stability than performing the same training without Exercise Sandals. However, Exercise Sandals do not impair postural stability and, therefore, might serve as an alternative rehabilitation tool for functional balance training. The results of this study have clinical relevance for clinicians, who might use our functional balance training protocol as a potential prophylactic program for both subjects with stable ankles and those with functionally unstable ankles.
Footnotes
* References 2, 4, 6, 8, 10, 11, 13–16, 19–28.
† References 2, 4, 6, 8, 10, 11, 13–15, 19–28.
‡ References 2, 6, 8, 10, 11, 13–15, 19, 21, 26, 28.
* References 2, 6, 8, 10, 11, 13–15, 19, 21, 26.
REFERENCES
- Bahr R, Karlsen R, Lian O, Ovrebo RV. Incidence and mechanisms of acute ankle inversion injuries in volleyball: a retrospective cohort story. Am J Sports Med. 1994;22:595–600. doi: 10.1177/036354659402200505. [DOI] [PubMed] [Google Scholar]
- Freeman MA, Dean MR, Hanham IW. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–685. [PubMed] [Google Scholar]
- McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35:103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhagen E, van der Beek A, Twisk J, Bouter L, Bahr R, van Mechelen W. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32:1385–1393. doi: 10.1177/0363546503262177. [DOI] [PubMed] [Google Scholar]
- Yeung MS, Chan KM, So CH, Yuan WY. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28:112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernier JN, Perrin DH. Effect of coordination training on proprioception of the functionally unstable ankle. J Orthop Sports Phys Ther. 1998;27:264–275. doi: 10.2519/jospt.1998.27.4.264. [DOI] [PubMed] [Google Scholar]
- Cornwall MW, Murrell P. Postural sway following inversion sprain of the ankle. J Am Podiatr Med Assoc. 1991;81:243–247. doi: 10.7547/87507315-81-5-243. [DOI] [PubMed] [Google Scholar]
- Eils E, Rosenbaum D. A multi-station proprioception exercise program in patients with ankle instability. Med Sci Sports Exerc. 2001;33:1991–1998. doi: 10.1097/00005768-200112000-00003. [DOI] [PubMed] [Google Scholar]
- Friden T, Zatterstrom R, Lindstrand A, Moritz U. A stabilometric technique for evaluation of lower limb instabilities. Am J Sports Med. 1989;17:118–122. doi: 10.1177/036354658901700120. [DOI] [PubMed] [Google Scholar]
- Gauffin H, Tropp H, Odenrick P. Effect of ankle disk training on postural control in patients with functional instability of the ankle joint. Int J Sports Med. 1988;9:141–144. doi: 10.1055/s-2007-1024996. [DOI] [PubMed] [Google Scholar]
- Goldie PA, Evans OM, Bach TM. Postural control following inversion injuries of the ankle. Arch Phys Med Rehabil. 1994;75:969–975. [PubMed] [Google Scholar]
- Konradsen L, Ravn JB. Prolonged peroneal reaction time in ankle instability. Int J Sports Med. 1991;12:290–292. doi: 10.1055/s-2007-1024683. [DOI] [PubMed] [Google Scholar]
- Matsusaka N, Yokoyama S, Tsurusaki T, Inokuchi S, Okita M. Effect of ankle disk training combined with tactile stimulation to the leg and foot on functional instability of the ankle. Am J Sports Med. 2001;29:25–30. doi: 10.1177/03635465010290010901. [DOI] [PubMed] [Google Scholar]
- Rozzi SL, Lephart SM, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29:478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- Tropp H, Ekstrand J, Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984;12:185–188. doi: 10.1177/036354658401200302. [DOI] [PubMed] [Google Scholar]
- Tropp H. Pronator muscle weakness in functional instability of the ankle joint. Int J Sports Med. 1986;7:291–294. doi: 10.1055/s-2008-1025777. [DOI] [PubMed] [Google Scholar]
- McGuine TA, Greene JJ, Best T, Leverson G. Balance as a predictor of ankle injuries in high school basketball players. Clin J Sport Med. 2000;10:239–244. doi: 10.1097/00042752-200010000-00003. [DOI] [PubMed] [Google Scholar]
- Tropp H, Ekstrand J, Gillquist J. Stabilometry in functional instability of the ankle and its value in predicting injury. Med Sci Sports Exerc. 1984;16:64–66. [PubMed] [Google Scholar]
- Blackburn T, Guskiewicz K, Petschauer M, Prentice W. Balance and joint stability: the relative contributions of proprioception and muscular strength. J Sport Rehabil. 2000;9:315–328. [Google Scholar]
- Docherty CL, Moore JH, Arnold BL. Effects of strength training on strength development and joint position sense in functionally unstable ankles. J Athl Train. 1998;33:310–314. [PMC free article] [PubMed] [Google Scholar]
- Hoffman M, Payne VG. The effects of proprioceptive ankle disk training on healthy subjects. J Orthop Sports Phys Ther. 1995;21:90–93. doi: 10.2519/jospt.1995.21.2.90. [DOI] [PubMed] [Google Scholar]
- Kaminiski TW, Buckley BD, Powers ME, Hubbard TJ, Ortiz C. Effect of strength and proprioception training on eversion to inversion strength ratios in subjects with unilateral functional ankle instability. Br J Sports Med. 2003;37:410–415. doi: 10.1136/bjsm.37.5.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne MD, Chou LS, Laskowski ER, Smith J, Kaufman KR. The effect of ankle disk training on muscle reaction time in subjects with a history of ankle sprain. Am J Sports Med. 2001;29:627–632. doi: 10.1177/03635465010290051601. [DOI] [PubMed] [Google Scholar]
- Verhagen E, Bobbert M, Inklaar M. The effect of a balance training programme on centre of pressure excursion in one-leg stance. Clin Biomech (Bristol, Avon) 2005;20:1094–1100. doi: 10.1016/j.clinbiomech.2005.07.001. et al. [DOI] [PubMed] [Google Scholar]
- Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996;23:332–336. doi: 10.2519/jospt.1996.23.5.332. [DOI] [PubMed] [Google Scholar]
- Rothermel S, Hale S, Hertel J, Denegar C. Effect of active foot positioning on the outcome of a balance training program. Phys Ther Sports. 2004;5:98–103. [Google Scholar]
- McGuine TA, Keene JS. The effect of a balance training program on the risk of ankle sprains in high school athletes. Am J Sports Med. 2006;34:1103–1111. doi: 10.1177/0363546505284191. [DOI] [PubMed] [Google Scholar]
- Ross SE, Guskiewicz KM. Effect of coordination training with and without stochastic resonance stimulation on dynamic postural stability of subjects with functional ankle instability and subjects with stable ankles. Clin J Sport Med. 2006;16:323–328. doi: 10.1097/00042752-200607000-00007. [DOI] [PubMed] [Google Scholar]
- Tropp H, Askling C, Gillquist J. Prevention of ankle sprains. Am J Sports Med. 1985;13:259–262. doi: 10.1177/036354658501300408. [DOI] [PubMed] [Google Scholar]
- Blackburn JT, Hirth CJ, Guskiewicz KM. Exercise Sandals increase lower extremity electromyographic activity during functional activities. J Athl Train. 2003;38:198–203. [PMC free article] [PubMed] [Google Scholar]
- Ross SE, Guskiewicz KM. Examination of static and dynamic postural stability in individuals with functionally stable and unstable ankles. Clin J Sport Med. 2004;14:332–338. doi: 10.1097/00042752-200411000-00002. [DOI] [PubMed] [Google Scholar]
- Janda V, Va'Vrova M. Sensory motor stimulation. In: Liebenson C, ed. Rehabilitation of the Spine: A Practitioner's Manual. New York, NY: Lippincott Williams & Wilkins; 1995:322–323 .
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Assoc; 1988:274–275.