Abstract
Reference/Citation: Rome K, Handoll HH, Ashford R. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 20052:CD000450. Update from Gillespie WJ, Grant I. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 20002: CD000450.
Clinical Question: Do evidence-based interventions exist for the prevention and treatment of stress reactions and stress fractures in young active adults?
Data Sources: This systematic review is an update of the original article, which was published in 2000. The authors conducted a literature review of computerized databases that included the Cochrane Musculoskeletal Injuries Group Specialized Register (April 2004), the Cochrane Central Register of Controlled Trials, MEDLINE (1966 to September 2004), EMBASE (1988 to 2004, week 36), CINAHL (1982 to 2004, September, week 1), Index to Theses (1990 to 2004), and Dissertation Abstracts (1990 to 2004). In addition, the authors searched the Current Controlled Trials at http://www.controlled-trials.com (June 2004, week 1) and the United Kingdom National Research Registrar at http://www.update-software.com/national/ (to issue 1, 2004) for current or recently completed studies. They also reviewed the British Journal of Podiatry, International Journal of Podiatric Biomechanics, Physiotherapy, and the Australian Journal of Podiatric Medicine for relevant studies. Furthermore, they contacted the Medical Departments of Defense Forces in Europe and North America to identify unpublished or unlisted military studies. Reference lists of all identified studies and Cochrane reviews were also investigated. The computer search strategy included 61 separate entries and included such terms as stress fractures, stress reactions, shin splints, overuse, athletic injuries, cumulative trauma disorders, running, and randomized controlled trial. The 3 authors of this updated review independently selected new articles for inclusion. Furthermore, the 12 articles that were included in the original systematic review were also reevaluated to ensure they met the defined inclusion criteria.
Study Selection: To qualify for inclusion, studies had to be randomized or quasirandomized control trials, involve interventions to prevent or treat lower extremity stress reactions and fractures, and include physically active adults (adolescence to middle age) who were involved in athletics or military training. Clinical and radiographic (bone scan or x-ray) evidence of a lower extremity stress reaction or stress fracture was also required for inclusion of treatment-based studies. Specifically, skeletal overuse injuries are considered the result of a cumulative and repetitive process that produces initial microstructural changes or stress reactions that are identified by bone scans or magnetic resonance imaging but not conventional radiographs. If cumulative stresses continue, structural changes are visualized on radiographs and are referred to as stress fractures. In addition, research studies involving the treatment of medial tibial stress syndrome or shin splints were excluded. Desired outcome measures for treatment studies included return to training time, return to normal physical activity, functional performance, quality of life measures, resource management (eg, costs, health care visits, diagnostic procedures), adverse effects, and compliance.
The inclusion criteria for stress fracture prevention studies were similar, except that the authors did not have to provide radiographic evidence of a stress fracture or stress reaction. Prevention studies included a combination of the following outcome measures: occurrence and location of stress fracture, stratification of diagnosis, incidence of other lower limb injuries, complications and adverse effects of prevention techniques, resource management, and compliance with the prevention strategy.
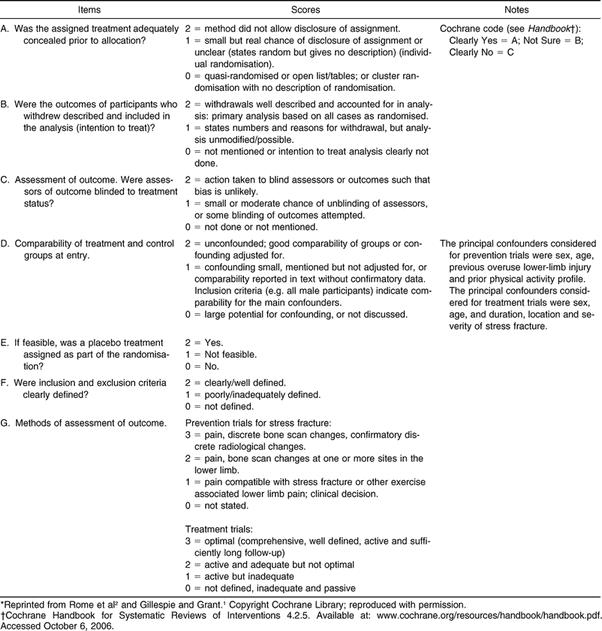
Data Extraction: At least 2 reviewers independently extracted the demographic and outcome data from the newly identified studies, and 1 author verified the data and results from the 12 studies included in the 2000 Cochrane review. Inconsistencies from the original review and data from all new studies were also checked by an additional reviewer. All 3 reviewers then independently evaluated the quality of inclusion studies using a quality scoring scheme ( Table). The categories considered included randomization or group allocation (A), intention-to-treat analysis (B), examiner blinding (C), comparison of experimental and control groups at baseline (D), use of a placebo treatment (E), clearly defined subject inclusion and exclusion criteria (F), and methods of outcome assessments (G). Items A through F were scored from 0 to 2 and item G from 0 to 3, for a total “best” quality assessment score (QAS) of 15. Inconsistencies among reviewers' QAS scores were resolved by discussion and with the aid of a discrepancies form.
Main Results: Search criteria identified 24 new studies since the previous review, 8 of which fulfilled the inclusion criteria. In addition, 4 of the 12 studies included in the original 2000 review were excluded. Three were excluded as a result of insufficient indication of subject or group randomization or quasirandomization, and the fourth excluded study included subjects with the diagnosis of medial tibial stress syndrome. Overall, 16 studies were included.
The authors of 13 studies focused on prevention, and 3 groups evaluated the treatment of stress fractures and reactions. The average number of subjects for prevention and treatment studies, respectively, was 1091 (range = 206 to 3025) and 34 (range = 21 to 60). All 13 prevention studies involved military personnel who performed physical training over a 9-to-14–week period. Quality assessment scores for prevention studies ranged from 4 to 10 (mean score = 7). In 9 prevention studies, the effectiveness of insoles or orthoses was evaluated, and the QAS for these studies ranged from 4 to 9 (mean = 6.2). The investigators in 4 studies assessed “shock-absorbing” insoles or orthoses in shoes or boots versus a control (shoes or boots alone), and an additional 5 groups compared insoles and orthoses against one another. One study's authors also evaluated military training in a modified high-top shoe versus standard military boots (QAS = 8). Two groups assessed the influence of pre-exercise stretching (QAS = 8 and 9, respectively), and one investigated the effects of calcium supplementation (QAS = 10).
In none of the prevention studies were adequate randomization and concealment of treatment before group allocation (item A) accomplished, and the researchers in 3 studies randomized groups (team or platoon) instead of individual participants. Attrition rates exceeded 50% in 2 studies, and missing subjects' data were unaccounted for in the final analysis of 3 studies (item B, intention-to-treat analysis). Also, in only 2 of 13 studies were examiners blinded to group assignment (item C). Radiographic (bone scan or x-ray) evidence for diagnostic confirmation of a stress reaction or fracture was used in 12 studies. The method of diagnosis (item G) was based solely on clinical examination or a self-report questionnaire in 2 studies, and diagnostic methods were not described in 2 studies.
Overall fewer osseous stress injuries were reported in the experimental groups for all 4 studies comparing military personnel in “shock absorbing insoles” with controls (no insoles). However, none of these 4 studies demonstrated a statistically significant reduction in lower extremity overuse osseous injuries. In addition, statistically significant results were reported in only 1 of 5 studies that compared various orthoses and insoles. The authors reported a significant reduction in tibial stress fractures for soldiers wearing custom-made semirigid or soft-foot orthoses versus those wearing standard insoles (relative risk = 0.46, 95% confidence interval = 0.22 to 0.93). In a follow-up study, no significant difference in stress fracture rates was seen between subjects who wore custom-made semirigid orthoses and those who wore biomechanical soft orthoses, thus precluding the ability to identify one best design for stress fracture reduction. No significant stress fracture or lower extremity injury rate differences were seen between the control and experimental groups involved in lower extremity stretching studies. Participants taking calcium supplements did not demonstrate a significant reduction in stress fractures (tibial only) versus controls. The differences among the prevention studies prohibited pooling of the data and subsequent meta-analysis. Authors of all 3 treatment studies investigated the effects of a pneumatic ankle foot orthosis (Aircast Corp, Summit, NJ). Follow-up for outcome measures ranged from 78 days to 6 months. Two studies were conducted with military recruits, and the other was conducted with competitive and recreational athletes (n = 18, age range = 18 to 45 years). Treatment QASs ranged from 7/15 to 11/ 15, with an average score of 9.3/15. Proper randomization (item A) and evaluator blinding (item C) were confirmed in 1 of the 3 treatment studies. Data pooled from all 3 studies reached statistical significance for mean number of days until returning to full activities (weighted mean difference with brace versus without brace = −33.39 days, 95% confidence interval = −44.18 to −22.59 days).
Conclusions: Currently, no solid evidence-based interventions to prevent lower extremity stress reactions or fractures exist. Limited evidence suggests that “shock absorbing” insoles may reduce the overall incidence of lower extremity osseous injuries in military personnel. Unfortunately, research does not support the best design for inserts or footwear modifications. There is also insufficient evidence to determine if pre-performance stretching or calcium supplementation offers added protection from lower extremity osseous overuse injuries. Initial evidence supports the use of a pneumatic brace and early mobilization for the treatment of tibal stress reactions and fractures, but additional studies are required to validate these findings. Further investigation concerning the prevention and treatment of lower extremity stress fractures is needed and would assist researchers in establishing and clarifying evidence-based intervention guidelines. Future randomized control trials that clearly define (ie, provide clinical and radiographic evidence for) the diagnosis of a stress fracture or reaction, implement appropriate randomization, and use intervention and outcome measures (functional and performance measurements) that are appropriate for active adults would assist this ongoing and necessary process.
Keywords: athletic injuries, outcomes assessment
COMMENTARY
Lower extremity stress fractures and stress reactions result in moderate to severe functional limitations that often preclude participation in sports and recreational and occupational activities. The Cochrane Library systematic reviews on stress fractures and stress reactions emphasize the continued need for quality research that critically evaluates strategies for the prevention and treatment of lower extremity osseous overuse injuries in athletes. 1, 2 Specifically, Rome et al 2 identified relatively few prevention and treatment studies that warranted review, and those they included had various methodologic limitations. For example, they emphasized that authors of future randomized control trials must include and clarify their clinical and radiographic criteria for the diagnosis and classification of stress reactions and fractures. 2 In addition, all but one of the groups studied military personnel, thus limiting the generalization of findings to civilians, who may demonstrate greater diversity in terms of age, activity levels, and footwear.
Cochrane Collaboration Methodological Quality Assessment Scoring Scheme*.
Despite these limitations, the updated review provides some contributions to current athletic training practice and future directions for research. The primary finding was the pooled evidence indicating that pneumatic bracing of tibial stress reactions and fractures and early mobilization reduce the time for return to full activity. The quality of bracing studies ranged from quality assessment scores (QASs) of 7/15 to 11/15, 3–5 and a significant reduction in return to activity outcome measures was demonstrated in 2 of the 3 studies. 4, 5 In fact, 1 of the 2 groups who reported a significant benefit (weighted mean difference = 53.25 fewer days to return to full activity versus controls, 95% confidence interval = −80.96 to −25.54 days) with bracing studied competitive and recreational athletes. 5 However, neither group disclosed if the evaluators recording outcomes were blinded to each patient's treatment status. 4, 5 In addition, neither group used functional outcome measures (eg, half-mile run, hop test) to operationally define the criteria required for return to full participation. Interestingly, the one set of authors who clearly described return-to-activity criteria and used blinding techniques did not identify a significant treatment effect for soldiers wearing the pneumatic brace. 3 Although this study was adequately powered to discern a significant difference in return to duty (power = .92, P > .24), the authors proposed that lack of a treatment effect may have been confounded by the subjects' drop-out rate (35%), compliance with brace wear, motivation, and the acuity of the injury. 3 Future randomized trials that control for the confounding variables listed above and that involve athletic populations are required before the widespread use of pneumatic bracing for athletes with tibial stress fractures/reactions can be recommended.
Based on the current literature, 2 no clear evidence-based strategy exists to prevent lower extremity osseous overuse injuries. Presently, only shock-absorbing insoles/orthoses, alternative footwear, lower extremity stretching, and calcium supplementation interventions have been critically analyzed. According to this review, the methods used in these studies were generally poor to fair (QAS range = 4/15 to 11/15, mean = 7/15). 2 In addition, a statistically significant reduction in stress fractures/reactions was noted in only 1 of the 9 orthoses/ insoles studies, and custom-made semirigid or soft-foot orthoses were superior to standard insoles. 6 These results need to be viewed with caution, considering that 51% of participants dropped out before the end of the study and that an intention-to-treat analysis was not conducted. Intention-to-treat analysis is an important feature of quality outcomes research because it preserves the randomization process by including all subjects in the data analysis, whether they completed the intervention or not. 7 The lack of a significant effect for insoles/ orthoses was also recently reported in a systematic review by Yeung and Yeung, 8 who evaluated prevention strategies for lower extremity soft tissue injuries in runners. Therefore, whether insoles/orthoses truly play a role in preventing lower extremity osseous and soft tissue injuries remains to be determined.
Interestingly, Yeung and Yeung 8 did report that modifications of training schedules prevented soft tissue injuries in the lower extremities of young adults. It is common for health care providers and coaches to advise their athletes to start slowly and to progressively build up training to avoid injury. Unfortunately, the authors of the present review were unable to evaluate if progressive exercise actually prevents stress reactions and fractures as a result of a void in this literature. Future research investigating preseason conditioning programs for the prevention of lower extremity osseous injuries is warranted.
Contrary to common practice, lower extremity stretching before training did not offer a protective effect from stress fractures or reactions. Neither study involving stretching (QAS 7/15, 8/15, respectively) showed a significant difference between the control and experimental groups for stress fracture prevention. In systematic reviews, Yeung and Yeung 8 and Herbert and Gabriel 9 also reported similar findings and concluded that pre-exercise stretching did not reduce the incidence of muscle soreness or lower extremity injuries in young active adults involved in running and marching. Collectively, these 3 reviews raise questions about the efficacy of pre-exercise stretching for the prevention of lower extremity injuries, including osseous overuse injuries. Further sport-specific (eg, running, basketball, gymnastics) research on physical performance, psychological benefits (eg, stress reduction), and injury prevention would allow for a broader view of the potential benefits that pre-exercise stretching may provide.
This systematic review confirms that the quality and number of studies involving interventional strategies for the prevention and treatment of lower extremity stress fractures are lacking. Evidence to indicate that young adults with a tibial stress fracture may benefit from pneumatic bracing is limited, and additional research involving specific populations (runners, jumping athletes, soldiers) is needed to confirm these results. Furthermore, it is clear that high-quality randomized control trials are needed to establish intervention strategies for preventing lower extremity stress fractures/reactions. Sport medicine providers are in an ideal position to conduct this meaningful research that will enhance the current level of evidence-based clinical practice.
Footnotes
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or the Department of Defense.
REFERENCES
- Gillespie WJ, Grant I. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 2000;2:CD000450. doi: 10.1002/14651858.CD000450. [DOI] [PubMed] [Google Scholar]
- Rome K, Handoll HH, Ashford R. Interventions for preventing and treating stress fractures and stress reactions of bone of the lower limbs in young adults. Cochrane Database Syst Rev. 2005;2:CD000450. doi: 10.1002/14651858.CD000450.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen CS, Flynn TW, Kardouni JR. The use of a pneumatic leg brace in soldiers with tibial stress fractures—a randomized clinical trial. Mil Med. 2004;169:880–884. doi: 10.7205/milmed.169.11.880. et al. [DOI] [PubMed] [Google Scholar]
- Slatyer M. Lower Limb Training in an Army Recruit Population: Newcastle. Newcastle, Australia: University of Newcastle; 1995.
- Swenson EJ, Jr, DeHaven KE, Sebastianelli WJ, Hanks G, Kalenak A, Lynch JM. The effect of a pneumatic leg brace on return to play in athletes with tibial stress fractures. Am J Sports Med. 1997;25:322–328. doi: 10.1177/036354659702500309. [DOI] [PubMed] [Google Scholar]
- Finestone A, Giladi M, Elad H. Prevention of stress fractures using custom biomechanical shoe orthoses. Clin Orthop Relat Res. 1999;360:182–190. doi: 10.1097/00003086-199903000-00022. et al. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Rennie R. Users' Guide to the Medical Literature. Essentials of Evidence-Based Clinical Practice. 3rd ed. Chicago, IL: American Medical Association; 2004.
- Yeung EW, Yeung SS. Interventions for preventing lower limb soft-tissue injuries in runners. Cochrane Database Syst Rev. 2001;3:CD001256. doi: 10.1002/14651858.CD001256. [DOI] [PubMed] [Google Scholar]
- Herbert RD, Gabriel M. Effects of stretching before and after exercising on muscle soreness and risk of injury: systematic review. BMJ. 2002;325:468. doi: 10.1136/bmj.325.7362.468. [DOI] [PMC free article] [PubMed] [Google Scholar]


