Abstract
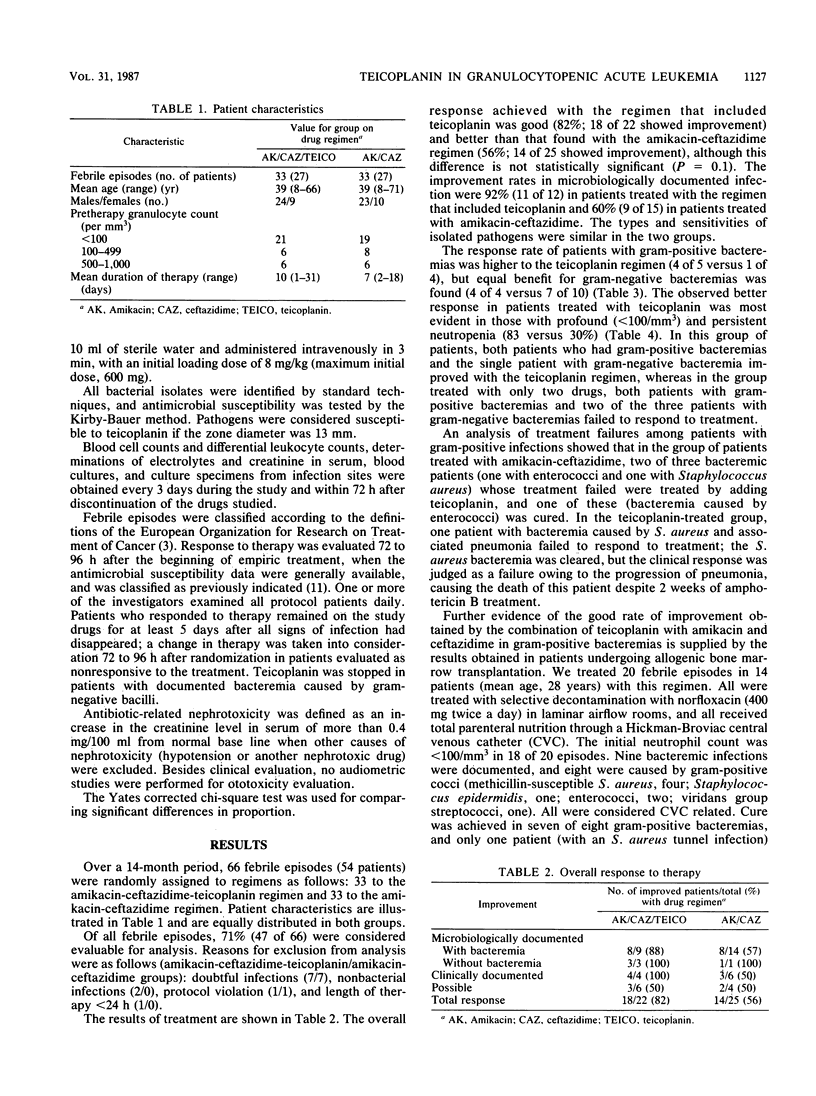
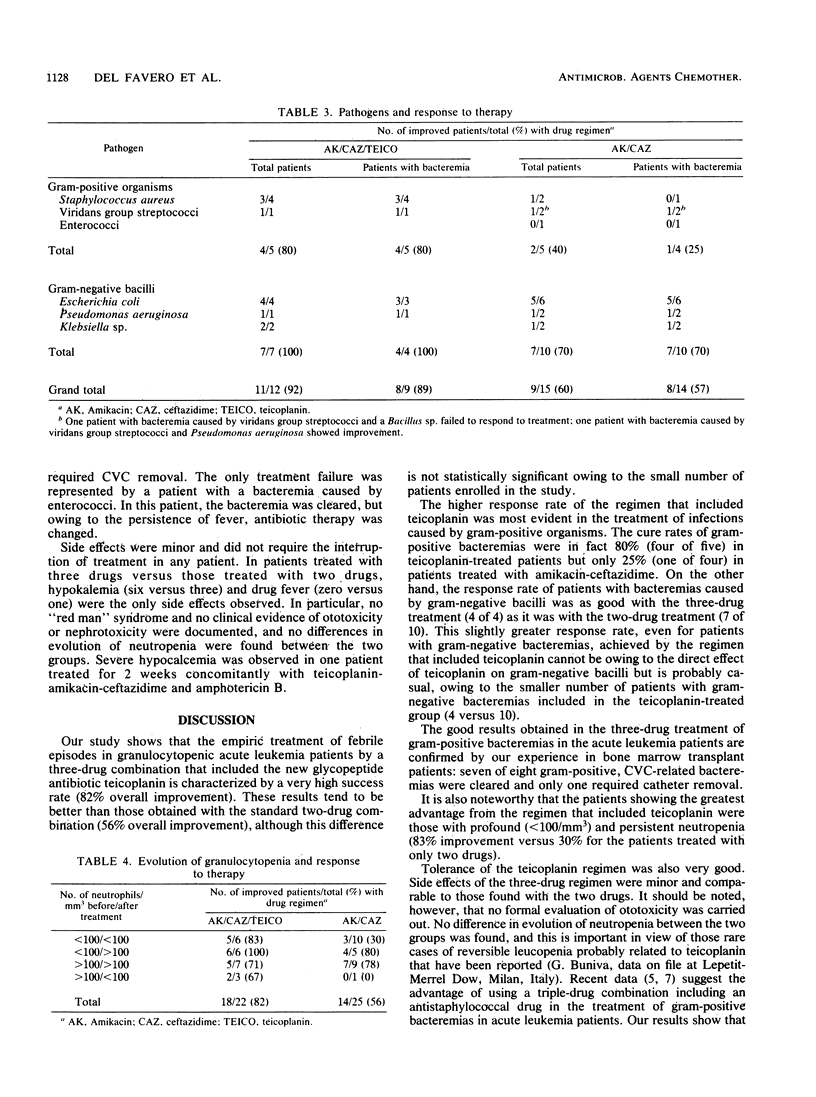
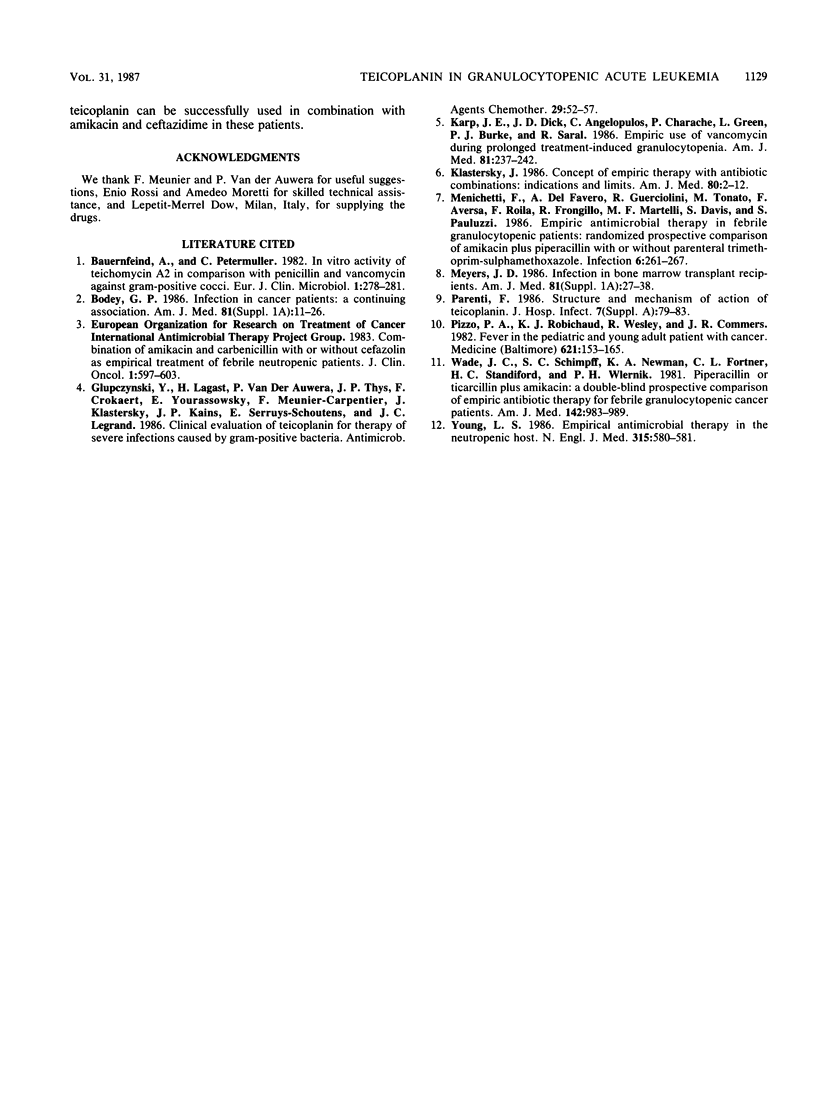
The increasing prevalence of bacteremia caused by gram-positive bacteria in granulocytopenic acute leukemia patients prompted us to evaluate, in a prospective randomized trial, the role of teicoplanin, a new glycopeptide antibiotic, when it was added to amikacin plus ceftazidime, as an empiric therapy of fever in these patients. Of 47 evaluable episodes, 22 were treated with the teicoplanin regimen and 25 were treated with the combination of amikacin and ceftazidime. The overall response to therapy of patients treated with teicoplanin was slightly better (82% improvement) than that obtained with amikacin plus ceftazidime (52%). The response rate of patients with gram-positive bacteremias was 80% (4 of 5) to the regimen that included teicoplanin; 25% (1 of 4) of the patients treated with amikacin plus ceftazidime responded to treatment; and for patients with gram-negative bacteremias, the response rates were, respectively, 100% (4 of 4) and 70% (7 of 10). The better results obtained with amikacin-ceftazidime-teicoplanin treatment were most evident in patients with profound (less than 100/mm3) and persistent neutropenia (83 versus 30% improvement). Furthermore, a good response rate of patients with gram-positive bacteremias (seven of eight; 87% improvement) was achieved in a small group of bone marrow transplant patients who were all treated with amikacin-ceftazidime-teicoplanin. No severe side effects were documented in any patient. Teicoplanin, as a drug administered as a single daily dose, seems to be a safe and useful anti-gram-positive agent when used in combination with amikacin-ceftazidime as an empiric therapy of febrile episodes in granulocytopenic acute leukemia patients.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bauernfeind A., Petermüller C. In vitro activity of teichomycin A 2 in comparison with penicillin and vancomycin against gram-positive cocci. Eur J Clin Microbiol. 1982 Oct;1(5):278–281. doi: 10.1007/BF02019971. [DOI] [PubMed] [Google Scholar]
- Bodey G. P. Infection in cancer patients. A continuing association. Am J Med. 1986 Jul 28;81(1A):11–26. doi: 10.1016/0002-9343(86)90510-3. [DOI] [PubMed] [Google Scholar]
- Glupczynski Y., Lagast H., Van der Auwera P., Thys J. P., Crokaert F., Yourassowsky E., Meunier-Carpentier F., Klastersky J., Kains J. P., Serruys-Schoutens E. Clinical evaluation of teicoplanin for therapy of severe infections caused by gram-positive bacteria. Antimicrob Agents Chemother. 1986 Jan;29(1):52–57. doi: 10.1128/aac.29.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karp J. E., Dick J. D., Angelopulos C., Charache P., Green L., Burke P. J., Saral R. Empiric use of vancomycin during prolonged treatment-induced granulocytopenia. Randomized, double-blind, placebo-controlled clinical trial in patients with acute leukemia. Am J Med. 1986 Aug;81(2):237–242. doi: 10.1016/0002-9343(86)90257-3. [DOI] [PubMed] [Google Scholar]
- Klastersky J. Concept of empiric therapy with antibiotic combinations. Indications and limits. Am J Med. 1986 May 30;80(5C):2–12. [PubMed] [Google Scholar]
- Menichetti F., Del Favero A., Guerciolini R., Tonato M., Aversa F., Roila F., Frongillo R. F., Martelli M. F., Davis S., Pauluzzi S. Empiric antimicrobial therapy in febrile granulocytopenic patients. Randomized prospective comparison of amikacin plus piperacillin with or without parenteral trimethoprim/sulphamethoxazole. Infection. 1986 Nov-Dec;14(6):261–267. doi: 10.1007/BF01643959. [DOI] [PubMed] [Google Scholar]
- Meyers J. D. Infection in bone marrow transplant recipients. Am J Med. 1986 Jul 28;81(1A):27–38. doi: 10.1016/0002-9343(86)90511-5. [DOI] [PubMed] [Google Scholar]
- Parenti F. Structure and mechanism of action of teicoplanin. J Hosp Infect. 1986 Mar;7 (Suppl A):79–83. doi: 10.1016/0195-6701(86)90011-3. [DOI] [PubMed] [Google Scholar]
- Pizzo P. A., Robichaud K. J., Wesley R., Commers J. R. Fever in the pediatric and young adult patient with cancer. A prospective study of 1001 episodes. Medicine (Baltimore) 1982 May;61(3):153–165. doi: 10.1097/00005792-198205000-00003. [DOI] [PubMed] [Google Scholar]
- Wade J. C., Schimpff S. C., Newman K. A., Fortner C. L., Standiford H. C., Wiernik P. H. Piperacillin or ticarcillin plus amikacin. A double-blind prospective comparison of empiric antibiotic therapy for febrile granulocytopenic cancer patients. Am J Med. 1981 Dec;71(6):983–990. doi: 10.1016/0002-9343(81)90324-7. [DOI] [PubMed] [Google Scholar]
- Young L. S. Empirical antimicrobial therapy in the neutropenic host. N Engl J Med. 1986 Aug 28;315(9):580–581. doi: 10.1056/NEJM198608283150910. [DOI] [PubMed] [Google Scholar]



