Abstract
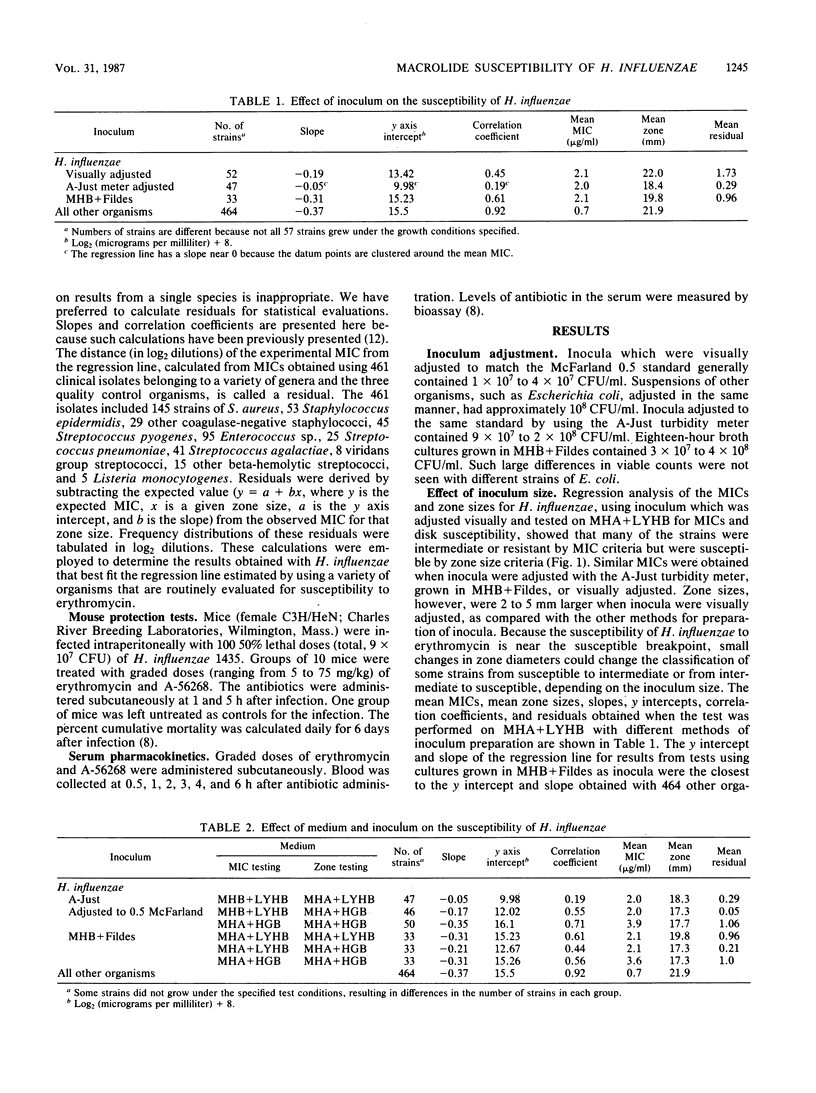
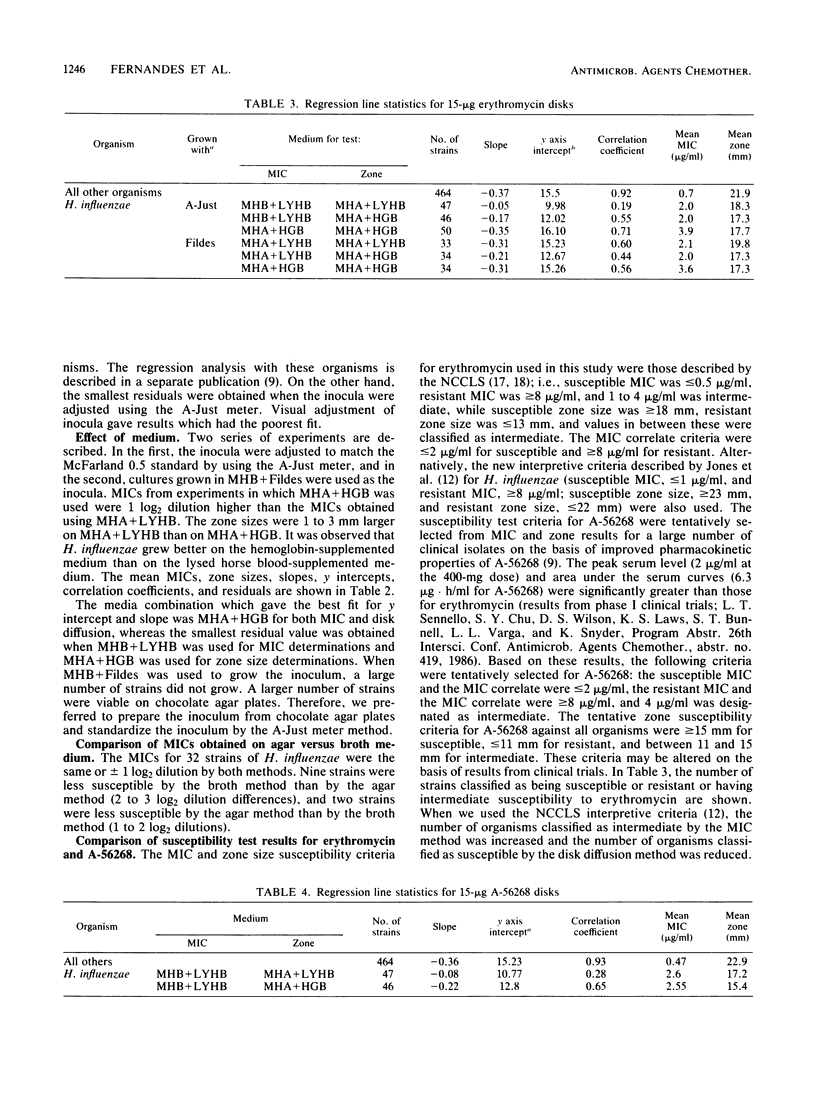
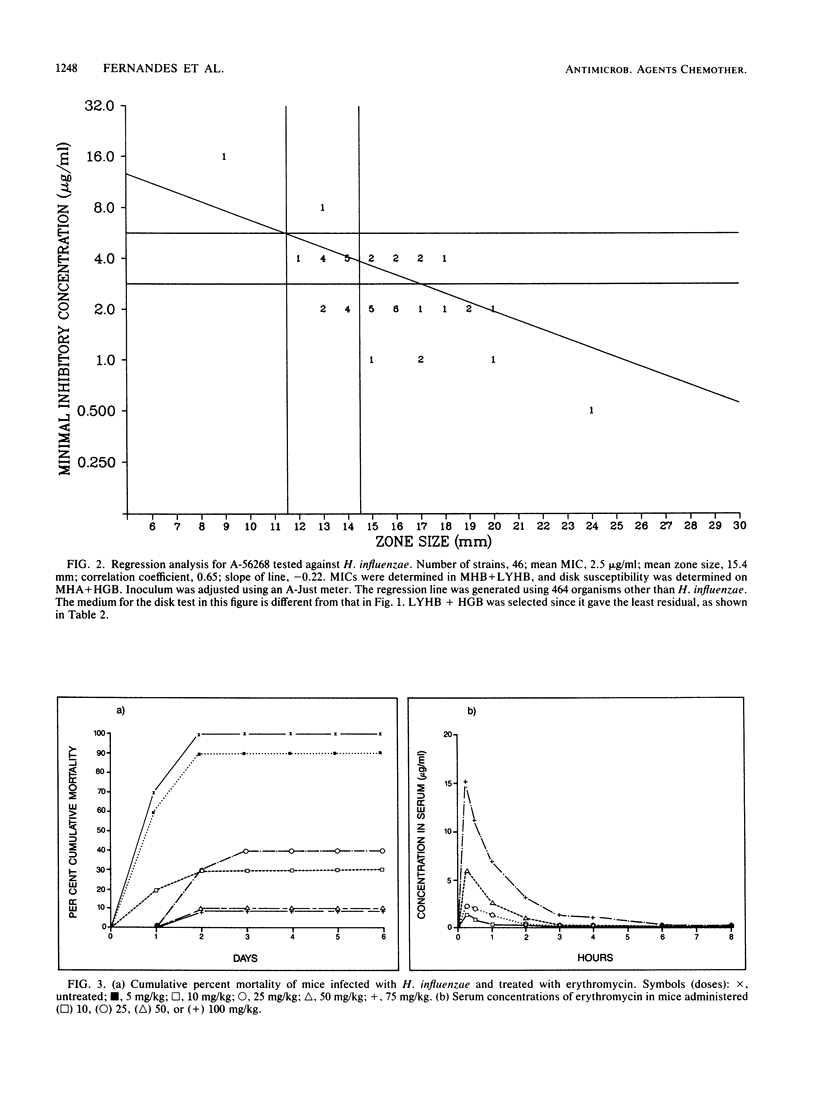
There is poor correlation between the MICs and zone sizes obtained for erythromycin against Haemophilus influenzae. The effect of two media, Mueller-Hinton medium supplemented with 3% lysed horse blood and 10 micrograms of NAD per ml (MHA + LYHB) and Mueller-Hinton agar supplemented with 1% bovine hemoglobin and 1% IsoVitaleX (MHA + HGB), on the MICs and zone sizes of erythromycin against H. influenzae was determined. The effect of three different methods for inoculum preparation on the susceptibility of H. influenzae was also determined. The MICs were independent of the method of inoculum preparation, but the zone sizes were smaller if the inoculum was carefully adjusted to contain approximately 10(8) CFU/ml. MICs were higher and zone sizes were smaller when MHA + HGB was used instead of MHA + LYHB. Good correlation was found when MHA + LYHB was used for determining the MIC and MHA + HGB was used for determining susceptibility by the disk method. When the inoculum was adjusted to match a McFarland 0.5 standard, the viable counts had to be approximately 10(8) CFU/ml for good correlation between MICs and zone sizes. A-56268, a new macrolide antibiotic, was tested against H. influenzae, and its MICs and tentative breakpoints against this organism were determined. The MICs obtained by various methods were correlated with in vivo efficacy by using a mouse septicemia model. MICs obtained on MHA + HGB or MHA + LYHB incubated without a 5% CO2 atmosphere showed the best correlation with in vivo efficacy.
Full text
PDF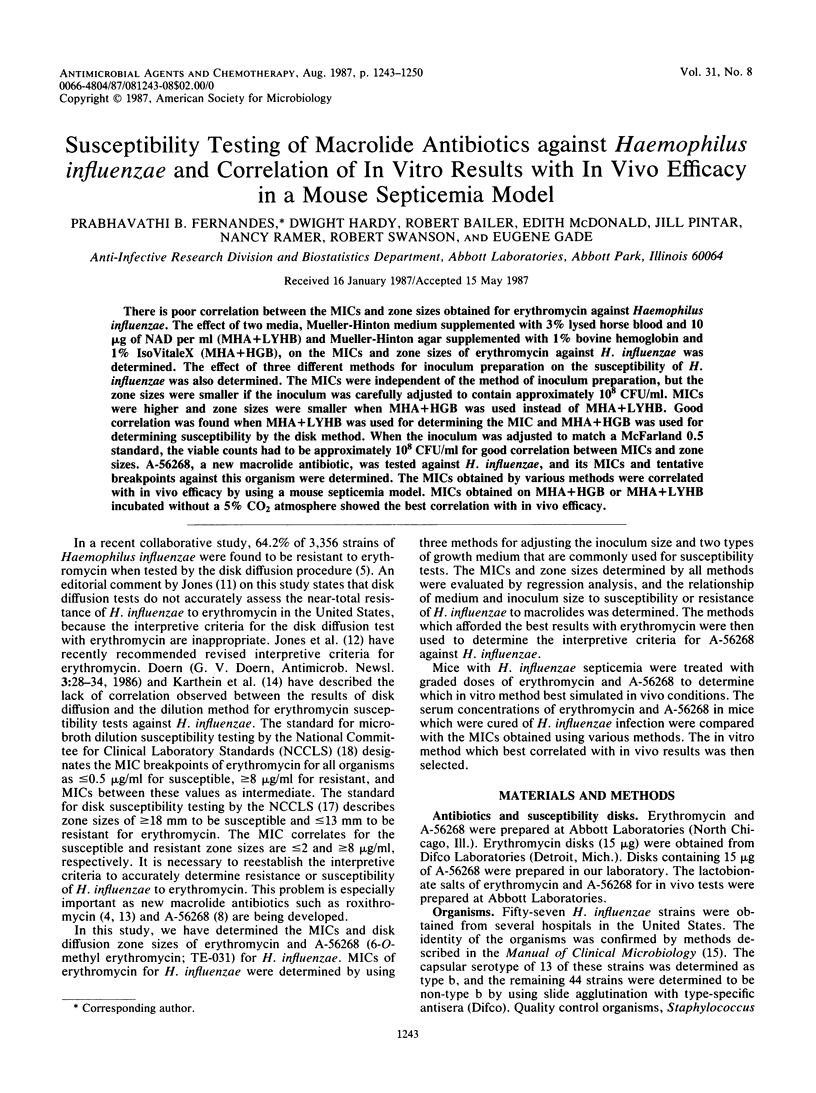


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barlam T., Neu H. C. In vitro comparison of the activity of RU 28965, a new macrolide, with that of erythromycin against aerobic and anaerobic bacteria. Antimicrob Agents Chemother. 1984 Apr;25(4):529–531. doi: 10.1128/aac.25.4.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass J. W., Steele R. W., Wiebe R. A., Dierdorff E. P. Erythromycin concentrations in middle ear exudates. Pediatrics. 1971 Sep;48(3):417–422. [PubMed] [Google Scholar]
- Chantot J. F., Bryskier A., Gasc J. C. Antibacterial activity of roxithromycin: a laboratory evaluation. J Antibiot (Tokyo) 1986 May;39(5):660–668. doi: 10.7164/antibiotics.39.660. [DOI] [PubMed] [Google Scholar]
- Doern G. V., Chapin K. C. Susceptibility of Haemophilus influenzae to amoxicillin/clavulanic acid, erythromycin, cefaclor, and trimethoprim/sulfamethoxazole. Diagn Microbiol Infect Dis. 1986 Jan;4(1):37–41. doi: 10.1016/0732-8893(86)90054-4. [DOI] [PubMed] [Google Scholar]
- Doern G. V., Jorgensen J. H., Thornsberry C., Preston D. A. Prevalence of antimicrobial resistance among clinical isolates of Haemophilus influenzae: a collaborative study. Diagn Microbiol Infect Dis. 1986 Feb;4(2):95–107. doi: 10.1016/0732-8893(86)90143-4. [DOI] [PubMed] [Google Scholar]
- Fernandes P. B., Bailer R., Swanson R., Hanson C. W., McDonald E., Ramer N., Hardy D., Shipkowitz N., Bower R. R., Gade E. In vitro and in vivo evaluation of A-56268 (TE-031), a new macrolide. Antimicrob Agents Chemother. 1986 Dec;30(6):865–873. doi: 10.1128/aac.30.6.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson C. W., Bailer R., Gade E., Rode R. A., Fernandes P. B. Regression analysis, proposed interpretative zone size standards, and quality control guidelines for a new macrolide antimicrobial agent, A-56268 (TE-031). J Clin Microbiol. 1987 Jun;25(6):1079–1082. doi: 10.1128/jcm.25.6.1079-1082.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard J. E., Nelson J. D., Clahsen J., Jackson L. H. Otitis media of infancy and early childhood. A double-blind study of four treatment regimens. Am J Dis Child. 1976 Sep;130(9):965–970. doi: 10.1001/archpedi.1976.02120100055008. [DOI] [PubMed] [Google Scholar]
- Jones R. N., Barry A. L., Fuchs P. C., Thornsberry C. Disk diffusion susceptibility testing of two macrolide antimicrobial agents: revised interpretive criteria for erythromycin and preliminary guidelines for roxithromycin (RU 965). J Clin Microbiol. 1986 Aug;24(2):233–239. doi: 10.1128/jcm.24.2.233-239.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R. N. Susceptibility testing of Haemophilus influenzae. Diagn Microbiol Infect Dis. 1986 Feb;4(2):93–94. doi: 10.1016/0732-8893(86)90142-2. [DOI] [PubMed] [Google Scholar]
- Jorgensen J. H., Redding J. S., Howell A. W. In vitro activity of the new macrolide antibiotic roxithromycin (RU 28965) against clinical isolates of Haemophilus influenzae. Antimicrob Agents Chemother. 1986 May;29(5):921–922. doi: 10.1128/aac.29.5.921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karthein J., Spohr M., Traub W. H. Josamycin: interpretation of inhibition zones with the Bauer-Kirby agar disk diffusion test as compared with erythromycin. Chemotherapy. 1986;32(4):336–343. doi: 10.1159/000238432. [DOI] [PubMed] [Google Scholar]
- Lorian V., Sabath L. D. Effect of pH on the activity of erythromycin against 500 isolates of gram-negative bacilli. Appl Microbiol. 1970 Nov;20(5):754–756. doi: 10.1128/am.20.5.754-756.1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renkonen O. V. Antibacterial activity of nine oral antibiotics against Streptococcus pneumoniae, Haemophilus influenzae and Branhamella catarrhalis. Scand J Infect Dis Suppl. 1983;39:106–108. [PubMed] [Google Scholar]
- Washington J. A., 2nd, Wilson W. R. Erythromycin: a microbial and clinical perspective after 30 years of clinical use (1). Mayo Clin Proc. 1985 Mar;60(3):189–203. doi: 10.1016/s0025-6196(12)60219-5. [DOI] [PubMed] [Google Scholar]


