Abstract
Despite improvements in cancer detection, prostate biopsy still lacks the ability to accurately map locations of cancer within the prostate. Improvements in prostate imaging may allow more accurate mapping of overall disease volume. Magnetic resonance (MR) spectroscopy allows improved specificity in detecting even small foci of disease within the peripheral zone. Improvements in MR-guided biopsy techniques may allow this technology to be adapted to therapeutics as well. Computer modeling of individual prostates serves as a means of designing optimized plans for prostate biopsy. The use of novel targeted biopsy schemes may allow an integration of available technologies in detection and localization of prostate cancer. Computer-directed needle biopsies based on anatomic landmarks within the prostate and computerized three-dimensional reconstruction of the gland may allow a highly reproducible means of identifying small foci of cancer, targeting them for therapy, and monitoring for recurrence. The TargetScan® system (Envisioneering Medical Technologies, St. Louis, MO) is the first technology to integrate available targeting methodologies in a systematic fashion.
Key words: Prostate cancer, Biopsy, Transrectal ultrasound, 3D mapping, TargetScan®
Since the clinical description of prostate-specific antigen (PSA), transrectal ultrasound (TRUS)-guided prostate biopsy has become of paramount importance in urologic practice. The technique of biopsy has evolved as the nature of diagnosed prostate cancers has migrated toward earlier-stage, smaller-volume disease. Maximizing biopsy outcomes implies improving detection, improving localization, improving negative predictive value, and avoiding oversampling, thus reducing the detection of clinically insignificant cancers.
Downward stage migration of prostate cancer secondary to the clinical use of PSA has resulted in the predominant detection of impalpable cancers. Over time, the number of cancers detected by ultrasonographic abnormalities has declined as well. As a result, the importance of accurate mapping of the gland through systematic biopsy has increased in contemporary practice. Systematic biopsy has been modified to increase cancer detection through increased sampling of the peripheral zone. Although detection on first biopsy has improved greatly, the negative predictive value remains a concern in the clinical management of men with elevated PSA values.
Secondary benefits of such increased sampling have included improved staging based on biopsy outcome, improved prediction of final pathologic grade, and perhaps an improvement in the ability to localize small unilateral cancers. Despite such modifications, the inability to stage and accurately localize cancers remains a major shortcoming of current biopsy techniques. Improved detection and localization offers the potential to implement strategies for focal therapy and more accurate follow-up of men who opt for active surveillance of early disease.
The increased likelihood of cancer detection at the time of biopsy reported in many recent series can be attributed to improved biopsy techniques. Several investigators have demonstrated the importance of adequate sampling to improve not only sensitivity but also negative predictive value. As such, current biopsy technique focuses on optimizing the number and location of cores at the time of biopsy.
Optimizing Cancer Diagnosis
Optimizing cancer diagnosis in clinical practice translates into increasing detection, minimizing the number of biopsies performed, and attempting to selectively identify those cancers deemed to pose a threat to the patient during his natural longevity. The combination of lowering PSA cutoff values, using extended biopsy cores, and the frequency of repeat biopsy has resulted in the detection of extremely small cancers that often may never pose a threat to the patient. As such, although objective data allow us to maximize detection, it remains of paramount importance for the practicing urologist to be judicious in aggressively pursuing small cancers, depending on the age and predicted longevity of the patient.
Number of Cores
Since the routine use of sextant biopsy in men with elevated PSA levels, it has been recognized that the negative predictive value of a 6-core biopsy alone is relatively poor.1–5 Roehl and colleagues reported on the results of serial sextant biopsies in a prostate cancer screening population.1 Among 962 men with cancer diagnosed on biopsy for elevated PSA level, 73% of cancers were detected by first biopsy, 91% by the second, 97% by the third, and 99% by the fourth. Likelihood of cancer declined with each serial biopsy but never reached zero. This experience is consistent with older reports stating that up to 96% of cancers are diagnosed within the first 2 sets of sextant biopsies.6
On the basis of the relatively poor negative predictive value of a sextant biopsy alone, investigators have used various techniques of increased sampling at the time of first biopsy. Levine and colleagues first evaluated the use of a 12-core biopsy, using 2 consecutive sets of sextant biopsy at 1 sitting.3 They demonstrated an increase in cancer detection to 31% overall, with only 21% being detected on the first sextant alone. These findings are consistent with the sextant data, and one could conclude that the negative predictive value of a 12-core biopsy is high, on the basis of previous sextant biopsy series demonstrating low cancer detection rates on third and fourth biopsy.
Other investigators have demonstrated that subsequently increased core biopsy is well tolerated,7 has no increase in complications relative to a sextant biopsy,7 and seems to identify clinically significant cancers.3–5 Pathologic analysis demonstrates that cancers diagnosed on increased core biopsy are smaller, on average, than those diagnosed on sextant biopsy, and to this end, earlier detection of cancer may be facilitated by increased sampling of the gland.8,9
The necessary number of cores may vary with the size of the prostate. Uzzo and colleagues previously have demonstrated a 38% cancer detection rate in glands larger than 50 cm3, compared with 23% in glands smaller than 50 cm3, at the time of sextant biopsy.10 As such, one could argue that a strategy of increasing core number relative to increasing prostate size may be a means of optimizing cancer detection. However, Chen and coworkers demonstrated through simulated biopsy of prostatectomy specimens that increasing the number of biopsies in larger glands is likely to increase the detection of clinically insignificant tumors.11
Location of Cores
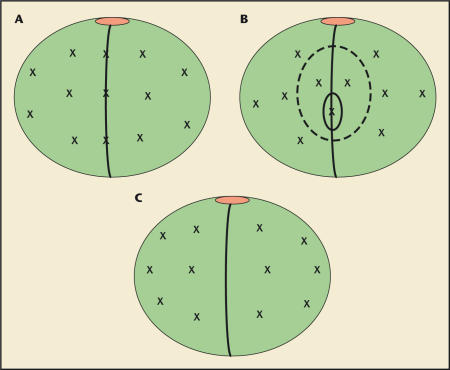
In addition to increased sampling of the prostate, improved cancer detection may be achieved through sampling of additional locations in the prostate (Figure 1).5,9,12–15 Original descriptions of the technique of ultrasound guided biopsy included sextant core sampling in the parasagittal location.16,17 Terris and associates postulated that the high rate of false negatives after sextant biopsy might be reduced by sampling more laterally to achieve better sampling of the peripheral zone.18 Laterally directed biopsies identified additional cancers in 14.6% of patients, but if lateral biopsies alone were performed, cancer would have been missed in 7.3% of patients.18
Figure 1.
Several extended biopsy templates have been proposed over the past years. All attempt to incorporate increased core number and sampling of the far-lateral region of the peripheral zone. (A) The 13-core, “5-region” biopsy12,13 incorporates 4 far-lateral cores. (B) The 11-core, multisite-directed biopsy14 includes several midsagittal cores. (C) The current 12-core biopsy used at New York University incorporates a far-lateral sextant sampling.
Eskew and colleagues reported on the incorporation of far-lateral biopsy cores when sampling the gland by a 5-region technique.13 Forty percent of patients were found to have cancer, and approximately one third of patients were found to have cancer in the additional regions only. The additional cancers predominantly were located in the far-lateral regions. This experience has been reconfirmed by several others demonstrating increased cancer detection in the far-lateral region of the peripheral zone.5,19–22
Using 3-dimensional (3D) computer simulation, Bauer and colleagues mapped the location of cancer in 201 step-sectioned, whole-mount, radical prostatectomy specimens.23 The likelihood of cancer detection was predicted according to conventional biopsy schemes. It was demonstrated that lateral sampling aided greatly in diagnosis and that 10- to 12-core schemes likely identified the majority of cancers (99%), whereas traditional sextant biopsies did not (72.6%).23
Role of Transition Zone Sampling
Although it has been demonstrated that T1c cancers are present more frequently in the transition zone than T2 cancers, the yield of routine biopsy remains low.24–28 This is likely owing to the relative size of the transition zone and the difficulty of adequate sampling through a transrectal approach. In the setting of a primary biopsy, cancer detection rates upon transition zone sampling have ranged from 1.8% to 4.3%, suggesting a limited role for routine use of transition zone biopsy.24–27 Because others have reported higher rates of detection on transition zone sampling at the time of repeat biopsy, this may be a reasonable approach.29 In fact, it has been demonstrated that the majority of cancers identified on repeat or serial biopsy are either in the far-lateral or anterior (transition zone) samples.30
Recent reports of systematic transperineal sampling have demonstrated higher rates of cancer detection on repeat biopsy.31 This is likely owing to a more effective sampling of the transition zone. Such approaches generally use a systematic sampling of the anterior base, midzone, and apex on either side. Several investigators have demonstrated cancer detection within the transition zone using a transurethral sampling strategy.32,33 Routine transurethral resection of the prostate (TURP) is generally carried out anterolaterally within the prostatic urethra. Often, because of the risk of postoperative retention, and to maximize sampling, a complete TURP is performed. Although reported detection rates with TURP are quite variable, our experience at New York University has been generally poor, and we have found that cancers are rarely detected in this manner. Given the relative morbidity of the procedure, we advocate that it should be avoided if possible.
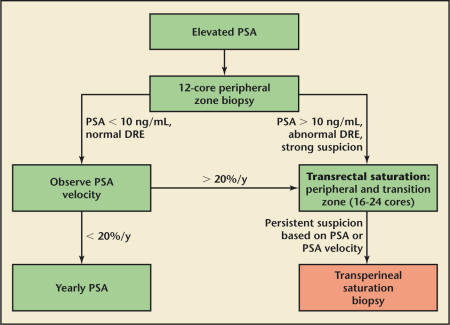
In patients strongly suspected of prostate cancer despite negative 12-core sampling, we generally proceed with repeat transrectal sampling inclusive of 12 peripheral zone cores and 6 to 8 transition zone samples. If the results from these are negative, magnetic resonance imaging (MRI) with spectroscopic evaluation is carried out to identify any suspicious regions of the prostate that might have been missed on original biopsy. In the case that such imaging is noninformative, we proceed with transperineal saturation biopsy inclusive of 24 transition zone samples. In rare circumstances, TURP is considered, particularly if the patient has underlying obstructive symptoms (Figure 2).
Figure 2.
The current New York University approach to men with negative prostate biopsy. PSA, prostate-specific antigen; DRE, digital rectal examination.
Cancer Localization
Localization of cancer at the time of biopsy has several potential clinical applications. Historically, the greatest value has been in predicting the risk of extracapsular disease at the time of planned treatment. This prediction is not made from the location of the cancer alone but rather from the combination of location, volume, and grade of disease in conjunction. It has been shown previously that location of positive core does not predict the location of extracapsular extension and that the negative predictive value of a single core is poor.34 Increase in sampling, through modifications in systematic biopsy technique, has improved the accuracy of estimating disease volume.
Recently there has been a strong interest in focal therapies for prostate cancer. Progressive downward stage migration of prostate cancer due to PSA screening, in combination with emerging technologies, such as radioactive seed implantation, cryoablation, and high-intensity focal ultrasound, have made focal therapy feasible in theory. To date, attempts to accurately localize the cancer using biopsy or a combination of biopsy and imaging have fallen short, with relatively poor accuracy. Clearly, the ability to better localize cancer with systematic biopsy may open the door to a number of emerging therapeutic strategies.
The historic problems with cancer localization are likely related, for the most part, to the multifocal, microscopic nature of contemporary prostate cancer. In cases of unilateral cancer on biopsy, bilateral disease is frequently noted at the time of radical prostatectomy. As such, the negative predictive value of biopsy becomes of paramount importance when contemplating focal therapy for the disease. An additional major problem with prostate biopsy is the interpretation of location. Clearly, the placement of needles at the lateral, parasagittal, base, midzone, or apex region is highly operator dependent. During biopsy, operators may slightly move the probe inadvertently, patient motion may occur, or visual interpretation of the image may be incorrect. Such errors may lead to misplaced needles, making true localization of the cancer impossible.
In improving prostate biopsy to allow for more accurate localization of cancer, several concepts are critical: 1) improved image detection of small cancer deposits; 2) development of sampling templates that allow maximal sensitivity in detecting all foci of prostate cancer; 3) developing highly reproducible biopsy conditions; and 4) recording of biopsy sites to allow accurate targeting for therapy and resampling. Several efforts are underway to address each of these issues.
Prostate Imaging
The accuracy of prostate biopsy was revolutionized with the advent of TRUS guidance. Before this, transrectal or transperineal biopsies were largely randomly done, and most cancer detection was in the setting of palpable nodules. Upon the initial description of TRUS-guided biopsy, hypoechoic lesions were often seen, and imageguided biopsy was the standard means of detection.35 With the migration of cancer to smaller-volume disease, imaging often reveals no abnormality, and the only value of TRUS is to anatomically guide the biopsy to various locations in the prostate.36 Several have reported improvements in cancer detection through the use of color flow Doppler imaging, but high false-positive rates limit the utility of such modalities. Even in those cases in which color flow Doppler imaging improves the efficacy of detection, it is inadequate to localize all deposits of disease in the gland.37,38
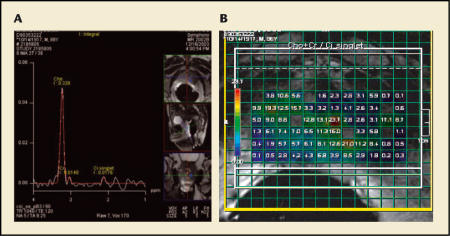
Cross-sectional imaging, such as computerized tomography (CT) and/or MRI lack the specificity to localize small amounts of cancer.39 Initially, pretreatment staging was thought to be improved through the use of such imaging, but once again stage migration has rendered conventional imaging relatively useless in detecting most diagnosed prostate cancers. Endorectal MRI provides greater resolution of the prostate, and its use has generally improved the specificity of detection.40,41 Decreased signal intensity of a T2-weighted image can be suggestive of prostate cancer (Figure 3), but it once again lacks specificity in that infection, infarction, and inflammation can all produce a similar appearance.
Figure 3.
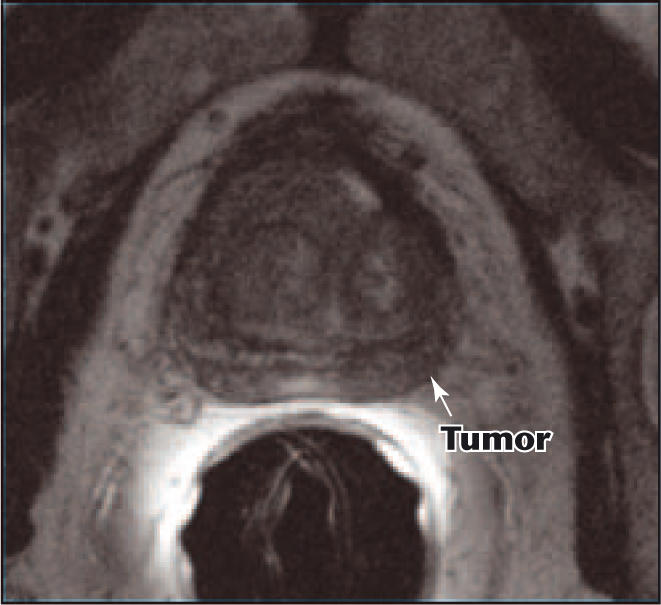
A T2-weighted endorectal magnetic resonance image demonstrates decreased signal intensity in the left peripheral zone (arrow), consistent with cancer. Follow-up biopsy failed to demonstrate cancer, suggesting the finding was a false positive.
The use of spectroscopy may allow further improvement in detection with MRI.42–44 The technique of spectroscopy allows evaluation of the relative content of tissue metabolites within subcentimeter regions of the prostate (voxels) (Figure 4). Those voxels with relative increase in choline and relative decrease in creatine and citrate are likely to contain cancer. Such imaging has dramatically improved the ability to identify cancers within the peripheral zone of the prostate. The major shortcoming of the technology remains the poor ability to discern deposits of cancer within the transition zone.45 Recently, investigators have determined that MR spectroscopy allows detection of approximately 50% of transition zone cancers but that the detection limits are greatly affected by disease volume and stage.46 Small cancers are hard to find. Additionally, because the image cannot be transferred to ultrasound, targeting of the lesions for biopsy or treatment requires MR guidance.
Figure 4.
Endorectal magnetic resonance spectroscopic imaging demonstrating the presence of extensive prostate cancer. (A) An illustration of the spectral display of metabolites within a single voxel (shown in the inset) of the prostate. In this case, the presence of high choline (large peak) and no citrate confirms the presence of prostate cancer. (B) Mapping of voxels over the whole prostate demonstrates diffuse cancer as evidenced by choline to citrate/creatine ratios > 0.8.
Computer Modeling
Several investigators have reported on the technique of 3D computer modeling of the prostate to determine the relative prevalence of prostate cancer within different regions of the gland. The value of such modeling would be in maximizing detection on biopsy, but also, secondarily, in the prediction of optimal biopsy templates to detect all of the cancer deposits (or as many as possible) within a gland.
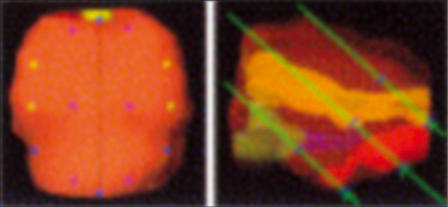
Bauer and colleagues evaluated whole-mount sections from 201 radical prostatectomy specimens to map the ideal locations for prostate biopsy.23 Digitized whole-mount sections were marked for areas of cancer and all anatomic structures and then stacked into 3D models inclusive of cancer locations (Figure 5). A biopsy interface was created to allow simulated biopsy of the 3D-modeled prostates. A total of 18 biopsies, of varying core number and distribution, were performed to determine the accuracy of cancer detection. A standard sextant biopsy detected only 72.6% of cancers, whereas 10-, 12-, and 14-core templates detected 99% of cancers. A 16-core sample, inclusive of transition zone cores, was 100% sensitive.
Figure 5.
Digitized whole-mount prostate sections are stacked to create a 3-dimensional prostate image incorporating locations of cancer. Simulated biopsy puncture lines predict the likelihood of cancer detection. Reprinted from Bauer JJ et al,23 with permission from Elsevier.
The Bauer study did not address the ability of the biopsies to detect all foci or individual quadrants/zones with cancer. In planning for focal therapy or effective disease monitoring, this is of paramount importance. Additionally, the practical shortcoming of any attempted computer modeling of the prostate is the inability to accurately place biopsy needles in the exact locations designated by the computer. This is due in part to the variability of prostate size and shape, and in part to the variability in operator interpretation of ultrasound imaging.
Targeted Biopsy
Using a combination of 3D mapping and knowledge of ideal biopsy templates, a targeted biopsy system should allow image-guided template biopsy with reliable sampling of the same locations in the prostate each time. In theory, such a biopsy would be based on biplanar anatomic landmarks, would take into account the variability in prostate volume and shape, and would allow reproducible sampling independent of the operator. Critical to the success of targeted biopsy is the ability of the guidance system to link the image to a computer model to a designated template for accurate needle placement. Additionally, through careful design of the template, such a biopsy should allow better negative accuracy through reproducible spatial sampling of all essential areas of the gland.
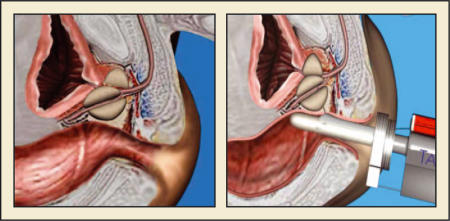
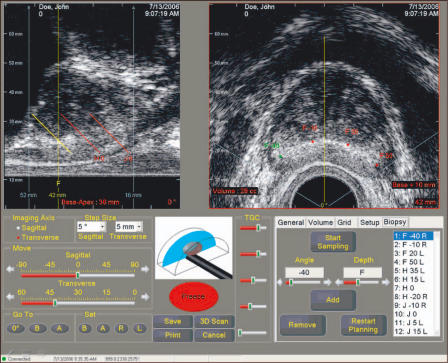
TargetScan. The TargetScan® TRUS-guided biopsy system (Envisioneering Medical Technologies, St. Louis, MO) is a recently developed device using a 3D imaging and targeting system to biopsy the prostate in a template fashion (Figure 6). The system uses a fixed transrectal ultrasound biopsy probe with computer-controlled biplanar movement of the transducer. At the time of transrectal ultrasound, the probe is inserted, positioned, and then fixed in place with a “brachystyle” probe stand (Figure 7). The contours of the prostate are recorded in both cross- and sagittal step-section without moving the probe. Acquired images then allow the calculation of a 3D prostate image for biopsy guidance. Serial step section allows assessment for visual abnormalities of the prostate as the image is recorded.
Figure 6.
The TargetScan® transrectal ultrasound-guided prostate biopsy system. Image courtesy of Envisioneering Medical Technologies.
Figure 7.
The fixed transducer probe is positioned in the rectum. The transducer crystal moves within the probe to positions designated by the program software. Image courtesy of Envisioneering Medical Technologies.
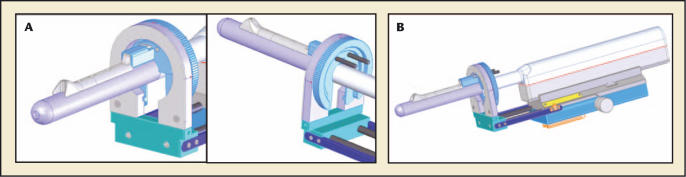
Next, biopsy positions are determined by the prostate for either 12- or 16-core sampling (Figure 8). The samples are positioned in the far-lateral and parasagittal positions, incorporating samples at the base, mid-gland, and apex in a standard template fashion; by arranging the cores at a fixed distance from the lateral border of the gland relative to the midline, reproducible sampling of specific regions is assured (Figure 9). The needle guide is rotated to the angle suggested by the computer (Figure 8A) and advanced in steps to the indicated distance from the apex of the gland (Figure 8B).
Figure 8.
The TargetScan® probe carriage allows (A) side-to-side rotation of the probe to align the needle with the radial position of the intended biopsy. The biopsy is performed with a bendable needle passed through a needle guide (B), which can be sequentially advanced along the probe to the appropriate distance from the apex. Image courtesy of Envisioneering Medical Technologies.
Figure 9.
The TargetScan® image allows simultaneous biplanar visualization of needle tracts relative to the gland apex and rectal wall. Radial lines plotted from the needle guide position allow determination of the degree of probe rotation. Image courtesy of Envisioneering Medical Technologies.
Biopsies are then taken using a novel bendable nitinol needle, which allows an angled deflection of the needle relative to the probe axis. In this manner, the cores are taken at a fixed distance from the probe and a fixed depth from the prostate capsule. Transition zone sampling requires the needle be advanced further into the guide. Biopsy positions and prostate contours are recorded in the device hard drive to be used for future reference in locating cancer or other abnormalities in the gland.
The proposed advantages of the TargetScan system include: 1) reliable localization of prostate zones; 2) recording of biopsy sites for future reference; 3) intra-operator and inter-operator reproducibility of biopsy techniques; 4) better spatial mapping of cancer volume; 5) better cancer detection; and 6) better localization of disease for potential focal therapy. The system has been used clinically for both biopsy and treatment guidance in brachytherapy.
Preliminary Data With TargetScan. In preliminary evaluation of the TargetScan system, biopsy was performed on 20 radical prostatectomy specimens from men who underwent radical prostatectomy for localized prostate cancer.47 The specimen was placed within a model allowing transrectal biopsy to be simulated. The whole prostate specimen was then step-sectioned to identify the stage, grade, and location of the cancer. Several important observations suggested the potential efficacy of the system. First, the number of cores with cancer was greater than that observed with the preoperative conventional biopsy (3.0 ± 2.0 SD vs 1.79 ± 1.27 SD), suggesting efficacy in detection. Second, cancer was identified in 16 of 20 patients and in 31 of 64 prostate quadrants on whole mount. The latter observation suggested a potential for strong sensitivity upon refinement of the template. Finally, the correlation of Gleason score between biopsy was better with the TargetScan system than conventional biopsy. Only 19% of the TargetScan biopsies were upgraded, compared with 45% of the preoperative biopsies.
Although the biopsies were performed ex vivo, the rate of detection and identification of positive quadrants was notably higher than that observed for conventional biopsy performed in an ex vivo setting. The suggestion of these findings is that the TargetScan biopsy may in fact improve the detection rate through more accurate sampling of the intended areas. This offers clear advantages not only for detection but also ultimately for localization of cancer.
In the same study, TargetScan biopsies were repeated by different surgeons to assess reproducibility of cancer detection.47 The findings of each individual core were replicated by surgeons in 85% of cores, regardless of a positive or negative sample. The implication of this finding is that the system may allow effective monitoring of disease foci either in follow-up of focal therapy or in the active surveillance setting.
In a second preclinical study, the nitinol needle samples taken with the TargetScan system were compared with those taken with a standard biopsy needle.48 Specimen weights were identical. The collective findings of the preclinical studies suggested that the system is highly effective in identifying cancer, that the proposed template seems quite good, and that the negative prediction of a negative core may correlate well with the radical prostatectomy specimen. Additionally, the system did not seem to be inferior to conventional biopsy techniques in any way.
Clinical Experience With TargetScan. On the basis of the compelling preclinical data, several centers have begun preliminary evaluation of the TargetScan system. No published data are available, but at the time of first informal review of data by the study centers, TargetScan biopsies had been performed in 9 centers within the United States by a total of 13 urologists. A total of 95 procedures were completed with the TargetScan system, resulting in cancer detection among 41% of biopsied patients.
Early problems encountered with the system were related to technical difficulties with probe carriage placement, difficulty with patient movement relative to the fixed probe, prostate motion relative to the fixed probe, and difficulty with the requirement of lithotomy position. With increasing experience, fewer problems have been encountered, and the cancer detection rate seems to have increased, perhaps suggesting a modest learning curve for application of the technology. After modifications to the probe carriage and after increasing operator experience, 63 biopsies were completed, with a cancer detection rate of 44.2%.
On the basis of the preliminary success of the TargetScan biopsy, a prospective data registry of 300 prostate biopsies is planned in 5 centers (New York University, Washington University, Duke University, the University of Michigan, and the University of Southern California). The goals of data collection are to assess the rates of detection, reproducibility among centers, and the spatial assessment of cancer relative to radical prostatectomy specimen. It is anticipated that if indeed cancer targeting is more accurate with the system, then broad application of the technology would allow more reliable preclinical information for selection of therapy, transfer of data from one practitioner to another, and ultimately for guiding targeted therapies or monitoring cancers in active surveillance protocols. Upon completion of data analysis, the contribution of TargetScan to the optimization of prostate biopsy and prostate cancer targeting will be better defined.
Conclusions
Prostate biopsy has evolved from a lesion-directed sampling to an image-guided sampling to a modeled systematic sampling. Much of the evolution is due to improvements in technology, but it is also due to the gradual migration toward earlier-stage disease and lower volumes of cancer. With the increased detection of small, early-stage cancers has come a more complex decision-making process with regard to treatment. In cases of focal prostate cancers, there is an increased interest in focal therapy or simple monitoring of disease through active surveillance. Both strategies require an accurate means of localizing cancer deposits within the gland.
Despite the improvements in cancer detection, prostate biopsy still lacks the ability to accurately map locations of cancer within the prostate. This is in part because of the multifocal nature of prostate cancer, but it is also owing to the variability of needle placement and image interpretation by urologists. Accurately re-identifying a location of small volume disease is virtually impossible.
Improvements in prostate imaging may allow more accurate mapping of overall disease volume. MR spectroscopy allows improved specificity in detecting even small foci of disease within the peripheral zone. Improvements in MR-guided biopsy techniques may allow this technology to be adapted to therapeutics as well. Computer modeling of individual prostates serves as a means of designing optimized plans for prostate biopsy.
The use of novel targeted biopsy schemes may allow an integration of available technologies in detection and localization of prostate cancer. Computer-directed needle biopsies based on anatomic landmarks within the prostate and computerized 3D reconstruction of the gland may allow highly reproducible means of identifying small foci of cancer, targeting them for therapy, and monitoring for recurrence. The TargetScan system is the first technology to integrate available targeting methodologies in a systematic fashion, and as such, it offers great potential in improving the accuracy of prostate cancer targeting.
Main Points.
In improving prostate biopsy to allow for more accurate localization of cancer, several concepts are critical: 1) improved image detection of small cancer deposits; 2) development of sampling templates that allow maximal sensitivity in detecting all foci of prostate cancer; 3) development of highly reproducible biopsy conditions; and 4) recording of biopsy sites to allow accurate targeting for therapy and resampling.
Improvements in cancer detection have been reported with color flow Doppler imaging, but high false-positive rates limit the utility of such modalities. Cross-sectional imaging, such as computerized tomography and/or magnetic resonance imaging (MRI), lack the specificity to localize small amounts of cancer. Endorectal MRI provides greater resolution of the prostate, and its use has generally improved the specificity of detection. Spectroscopy may allow further improvement in detection with MRI.
Critical to the success of targeted biopsy is the ability of the guidance system to link the image to a computer model to a designated template for accurate needle placement. The TargetScan® transrectal ultrasound-guided biopsy system (Envisioneering Medical Technologies, St. Louis, MO) is a recently developed device using a 3-dimensional imaging and targeting system to biopsy the prostate in a template fashion.
The proposed advantages of the TargetScan system include: 1) reliable localization of prostate zones; 2) recording of biopsy sites for future reference; 3) intra-operator and inter-operator reproducibility of biopsy techniques; 4) better spatial mapping of cancer volume; 5) better cancer detection; and 6) better localization of disease for potential focal therapy.
References
- 1.Roehl KA, Antenor JA, Catalona WJ. Serial biopsy results in prostate cancer screening study. J Urol. 2002;167:2435–2439. [PubMed] [Google Scholar]
- 2.Catalona WJ, Smith DS, Ratliff TL, et al. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N Engl J Med. 1991;324:1156–1161. doi: 10.1056/NEJM199104253241702. [DOI] [PubMed] [Google Scholar]
- 3.Levine MA, Ittman M, Melamed J, Lepor H. Two consecutive sets of transrectal ultrasound guided sextant biopsies of the prostate for the detection of prostate cancer. J Urol. 1998;159:471–475. doi: 10.1016/s0022-5347(01)63951-x. discussion 475–476. [DOI] [PubMed] [Google Scholar]
- 4.Borboroglu PG, Comer SW, Riffenburgh RH, Amling CL. Extensive repeat transrectal ultrasound guided prostate biopsy in patients with previous benign sextant biopsies. J Urol. 2000;163:158–162. [PubMed] [Google Scholar]
- 5.Babaian RJ, Toi A, Kamoi K, et al. A comparative analysis of sextant and an extended 11-core multisite directed biopsy strategy. J Urol. 2000;163:152–157. [PubMed] [Google Scholar]
- 6.Keetch DW, Catalona WJ, Smith DS. Serial prostatic biopsies in men with persistently elevated serum prostate specific antigen values. J Urol. 1994;151:1571–1574. doi: 10.1016/s0022-5347(17)35304-1. [DOI] [PubMed] [Google Scholar]
- 7.Naughton CK, Ornstein DK, Smith DS, Catalona WJ. Pain and morbidity of transrectal ultrasound guided prostate biopsy: a prospective randomized trial of 6 versus 12 cores. J Urol. 2000;163:168–171. [PubMed] [Google Scholar]
- 8.Chan TY, Chan DY, Stutzman KL, Epstein JI. Does increased needle biopsy sampling of the prostate detect a higher number of potentially insignificant tumors? J Urol. 2001;166:2181–2184. [PubMed] [Google Scholar]
- 9.Chen ME, Troncoso P, Tang K, et al. Comparison of prostate biopsy schemes by computer simulation. Urology. 1999;53:951–960. doi: 10.1016/s0090-4295(98)00639-6. [DOI] [PubMed] [Google Scholar]
- 10.Uzzo RG, Wei JT, Waldbaum RS, et al. The influence of prostate size on cancer detection. Urology. 1995;46:831–836. doi: 10.1016/s0090-4295(99)80353-7. [DOI] [PubMed] [Google Scholar]
- 11.Chen ME, Troncoso P, Johnston DA, et al. Optimization of prostate biopsy strategy using computer based analysis. J Urol. 1997;158:2168–2175. doi: 10.1016/s0022-5347(01)68188-6. [DOI] [PubMed] [Google Scholar]
- 12.Eskew LA, Woodruff RD, Bare RL, McCullough DL. Prostate cancer diagnosed by the 5 region biopsy method is significant disease. J Urol. 1998;160(3 pt 1):794–796. doi: 10.1016/S0022-5347(01)62789-7. [DOI] [PubMed] [Google Scholar]
- 13.Eskew LA, Bare RL, McCullough DL. Systematic 5 region prostate biopsy is superior to sextant method for diagnosing carcinoma of the prostate. J Urol. 1997;157:199–202. discussion 202–203. [PubMed] [Google Scholar]
- 14.Babaian RJ. Extended field prostate biopsy enhances cancer detection. Urology. 2000;55:453–456. doi: 10.1016/s0090-4295(00)00469-6. [DOI] [PubMed] [Google Scholar]
- 15.Chen ME, Troncoso P, Johnston D, et al. Prostate cancer detection: relationship to prostate size. Urology. 1999;53:764–768. doi: 10.1016/s0090-4295(98)00574-3. [DOI] [PubMed] [Google Scholar]
- 16.Hodge KK, McNeal JE, Stamey TA. Ultrasound guided transrectal core biopsies of the palpably abnormal prostate. J Urol. 1989;142:66–70. doi: 10.1016/s0022-5347(17)38663-9. [DOI] [PubMed] [Google Scholar]
- 17.Hodge KK, McNeal JE, Terris MK, Stamey TA. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989;142:71–74. doi: 10.1016/s0022-5347(17)38664-0. discussion 74–75. [DOI] [PubMed] [Google Scholar]
- 18.Terris MK, Wallen EM, Stamey TA. Comparison of mid-lobe versus lateral systematic sextant biopsies in the detection of prostate cancer. Urol Int. 1997;59:239–242. doi: 10.1159/000283071. [DOI] [PubMed] [Google Scholar]
- 19.Applewhite JC, Matlaga BR, McCullough DL. Results of the 5 region prostate biopsy method: the repeat biopsy population. J Urol. 2002;168:500–503. [PubMed] [Google Scholar]
- 20.Chon CH, Lai FC, McNeal JE, Presti JC., Jr. Use of extended systematic sampling in patients with a prior negative prostate needle biopsy. J Urol. 2002;167:2457–2460. [PubMed] [Google Scholar]
- 21.Gore JL, Shariat SF, Miles BJ, et al. Optimal combinations of systematic sextant and laterally directed biopsies for the detection of prostate cancer. J Urol. 2001;165:1554–1559. [PubMed] [Google Scholar]
- 22.Presti JC , Jr, Chang JJ, Bhargava V, Shinohara K. The optimal systematic prostate biopsy scheme should include 8 rather than 6 biopsies: results of a prospective clinical trial. J Urol. 2000;163:163–166. discussion 166–167. [PubMed] [Google Scholar]
- 23.Bauer JJ, Zeng J, Weir J, et al. Three-dimensional computer-simulated prostate models: lateral prostate biopsies increase the detection rate of prostate cancer. Urology. 1999;53:961–967. doi: 10.1016/s0090-4295(99)00068-0. [DOI] [PubMed] [Google Scholar]
- 24.Keetch DW, Catalona WJ. Prostatic transition zone biopsies in men with previous negative biopsies and persistently elevated serum prostate specific antigen values. J Urol. 1995;154:1795–1797. [PubMed] [Google Scholar]
- 25.Fleshner NE, Fair WR. Indications for transition zone biopsy in the detection of prostatic carcinoma. J Urol. 1997;157:556–558. [PubMed] [Google Scholar]
- 26.Terris MK, Pham TQ, Issa MM, Kabalin JN. Routine transition zone and seminal vesicle biopsies in all patients undergoing transrectal ultrasound guided prostate biopsies are not indicated. J Urol. 1997;157:204–206. [PubMed] [Google Scholar]
- 27.Bazinet M, Karakiewicz PI, Aprikian AG, et al. Value of systematic transition zone biopsies in the early detection of prostate cancer. J Urol. 1996;155:605–606. [PubMed] [Google Scholar]
- 28.Chang JJ, Shinohara K, Hovey RM, et al. Prospective evaluation of systematic sextant transition zone biopsies in large prostates for cancer detection. Urology. 1998;52:89–93. doi: 10.1016/s0090-4295(98)00116-2. [DOI] [PubMed] [Google Scholar]
- 29.Lui PD, Terris MK, McNeal JE, Stamey TA. Indications for ultrasound guided transition zone biopsies in the detection of prostate cancer. J Urol. 1995;153(3 pt 2):1000–1003. [PubMed] [Google Scholar]
- 30.Mian BM, Naya Y, Okihara K, et al. Predictors of cancer in repeat extended multisite prostate biopsy in men with previous negative extended multisite biopsy. Urology. 2002;60:836–840. doi: 10.1016/s0090-4295(02)01950-7. [DOI] [PubMed] [Google Scholar]
- 31.Pinkstaff DM, Igel TC, Petrou SP, et al. Systematic transperineal ultrasound-guided template biopsy of the prostate: three-year experience. Urology. 2005;65:735–739. doi: 10.1016/j.urology.2004.10.067. [DOI] [PubMed] [Google Scholar]
- 32.Philip J, Dutta RS, Scally J, et al. Importance of TURP in diagnosing prostate cancer in men with multiple negative biopsies. Prostate. 2005;64:200–202. doi: 10.1002/pros.20239. [DOI] [PubMed] [Google Scholar]
- 33.Pryor MB, Schellhammer PF. The pursuit of prostate cancer in pateints with a rising prostate specific antigen and multiple negative transrectal ultrasound-guided biopsies. Clin Prostate Cancer. 2002;1:172–176. doi: 10.3816/cgc.2002.n.019. [DOI] [PubMed] [Google Scholar]
- 34.Taneja SS, Epelbaum A, Penson D, et al. Does site-specific labelling of sextant biopsy cores of the prostate predict the site of extracapsular extension in radical prostatectomy surgical specimen? J Urol. 1999;162:1352–1358. [PubMed] [Google Scholar]
- 35.Abe M, Hashimoto T, Matsuda T, et al. Prostatic biopsy guided by transrectal ultrasonography using real-time linear scanner. Urology. 1987;29:567–569. doi: 10.1016/0090-4295(87)90057-4. [DOI] [PubMed] [Google Scholar]
- 36.Hodge KK, McNeal JE, Terris MK, Stamey TA. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989;142:71–74. doi: 10.1016/s0022-5347(17)38664-0. discussion 74–75. [DOI] [PubMed] [Google Scholar]
- 37.Cheng S, Rifkin MD. Color Doppler imaging of the prostate: important adjunct to endorectal ultrasound of the prostate in the diagnosis of prostate cancer. Ultrasound Q. 2001;17:185–189. doi: 10.1097/00013644-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 38.Kravchick S, Cytron S, Peled R, et al. Using grayscale and two different techniques of color Doppler sonography to detect prostate cancer. Urology. 2003;61:977–981. doi: 10.1016/s0090-4295(02)02520-7. [DOI] [PubMed] [Google Scholar]
- 39.Coakley FV, Qayyum A, Kurhanewicz J. Magnetic resonance imaging and spectroscopic imaging of prostate cancer. J Urol. 2003;170(6 pt 2):S69–S75. doi: 10.1097/01.ju.0000094958.23276.c4. discussion S75–S76. [DOI] [PubMed] [Google Scholar]
- 40.Beyersdorff D, Taupitz M, Winkelmann B, et al. Patients with a history of elevated prostate-specific antigen levels and negative transrectal US-guided quadrant or sextant biopsy results: value of MR imaging. Radiology. 2002;224:701–706. doi: 10.1148/radiol.2243011553. [DOI] [PubMed] [Google Scholar]
- 41.Perrotti M, Han KR, Epstein RE, et al. Prospective evaluation of endorectal magnetic resonance imaging to detect tumor foci in men with prior negative prostatic biopsy: a pilot study. J Urol. 1999;162:1314–1317. [PubMed] [Google Scholar]
- 42.Coakley FV, Kurhanewicz J, Lu Y, et al. Prostate cancer tumor volume: measurement with endorectal MR and MR spectroscopic imaging. Radiology. 2002;223:91–97. doi: 10.1148/radiol.2231010575. [DOI] [PubMed] [Google Scholar]
- 43.Scheidler J, Hricak H, Vigneron DB, et al. Prostate cancer: localization with three-dimensional proton MR spectroscopic imaging-clinicopathologic study. Radiology. 2002;213:473–480. doi: 10.1148/radiology.213.2.r99nv23473. [DOI] [PubMed] [Google Scholar]
- 44.Wefer AE, Hricak H, Vigneron DB, et al. Sextant localization of prostate cancer: comparison of sextant biopsy, magnetic resonance imaging and magnetic resonance spectroscopic imaging with step section histology. J Urol. 2000;164:400–404. [PubMed] [Google Scholar]
- 45.Zakian KL, Eberhardt S, Hricak H, et al. Transition zone prostate cancer: metabolic characteristics at 1H MR spectroscopic imaging-initial results. Radiology. 2003;229:241–247. doi: 10.1148/radiol.2291021383. [DOI] [PubMed] [Google Scholar]
- 46.Akin O, Sala E, Moskowitz CS, et al. Transition zone prostate cancers: features, detection, localization, and staging at endorectal MR imaging. Radiology. 2006;239:784–792. doi: 10.1148/radiol.2392050949. [DOI] [PubMed] [Google Scholar]
- 47.Bullock TL, Traxel EJ, Belani JS, et al. Evaluation of TargetScan™ system in prostate cancer detection [poster 223]; Annual Meeting of the American Urological Society; May 21–26, 2005; San Antonio, TX. [Google Scholar]
- 48.Bullock TL, Belani JS, Yan Y, Andriole GL. Comparison of biopsy sample weights between a novel bendable biopsy needle versus the industry standard [poster 116]; Annual Meeting of the American Urological Society; May 21–26, 2005; San Antonio, TX. [Google Scholar]