Abstract
Objective. We tested the effectiveness of a long-term coordinated care strategy—intensive case management (ICM)—compared with usual care (UC) among a group of substance-dependent women receiving Temporary Assistance for Needy Families (TANF).
Methods. Substance-dependent women on TANF (N=302) were recruited from welfare offices. They were assessed and randomly assigned to ICM or UC; follow-up was at 3, 9, and 15 months. UC consisted of a health assessment at the welfare office and a referral to substance abuse treatment and TANF services. ICM clients received ICM services in addition to UC services.
Results. ICM clients had significantly higher levels of substance abuse treatment initiation, engagement, and retention compared with UC clients. In some cases, ICM treatment attendance rates were double those of UC rates. Additionally, almost twice as many ICM clients were abstinent at the 15 month follow-up compared with UC clients (P<.0025).
Conclusions. ICM is a promising intervention for managing the chronic nature of substance dependence among women receiving TANF. Future research should refine long-term care strategies—such as ICM—that address the chronic nature of substance dependence among low-income populations.
Substance abuse is a national health problem that creates serious personal impairment and major social and economic burdens. Addressing substance abuse among low-income mothers may be especially important because of its impact on children, who face a much greater risk for becoming substance abusers themselves.1–3 Additionally, the combination of substance abuse and poverty fuels an inter-generational pattern of severe personal and social dysfunction that creates barriers to resolving substance use disorders.4
Substance abuse is a highly stigmatized behavior. Stigma and concealment issues are especially pronounced among low-income mothers, who may fear loss of welfare benefits or involvement with child protective services if they provide accurate reports about their substance use.5 Thus, accurate data on prevalence rates of substance abuse among low-income women are lacking; however, studies have consistently found that low-income women have significantly higher rates of illicit drug use and substance abuse compared with the rates of other women.6–8 Additionally, recent studies that used self-reports of women on Temporary Assistance for Needy Families (TANF) have yielded rates of substance dependence (alcohol and illicit drugs) that range from 5% to 11%, with an additional 5% to 8% engaged in regular heavy drinking or illicit drug use.5 Some studies have suggested that these ranges may significantly underestimate the true prevalence of this problem.9
Studies have shown that community substance abuse treatment, especially outpatient treatment, is poorly matched to the needs of substance-dependent low-income mothers.10,11 These women fail to enter and engage in treatment, and studies have reported poor outcomes. An evolving science-based model that views substance dependence as a chronic illness suggests that in order to improve outcomes, treatment must provide greater coordination of social and other health care services beyond just treating substance abuse.12 Additionally, long-term care strategies—similar to those used for other chronic diseases—must replace the current system of disconnected episodes of acute care.12
Substance abuse among low-income mothers has been a public health priority for more than 2 decades, and welfare reform legislation passed in 1996 has raised new concerns. Under TANF regulations, women who fail to participate in mandated work activities face sanction and loss of benefits. Current welfare reform emphasizes finding a job quickly and is not likely to be effective among substance-dependent women; however, simply referring these women to substance abuse treatment also is insufficient for reasons already noted. Indeed, studies have shown that substance-dependent women on TANF have significantly more social and health care problems that are barriers to employment: they are less likely to be employed, they are more likely to be sanctioned, and they have substantially higher rates of involvement with child protective services compared with women who do not have a substance use disorder.13 Despite rising concern, there is an absence of research for guiding policy and program development in this area.
Intensive case management (ICM) may be a promising approach for substance-dependent women on TANF. ICM is consistent with a chronic disease management strategy that augments current disconnected episodes of acute care with longer-term care strategies and cross-systems coordination that addresses other health and social needs and provides relapse monitoring and support during extended time periods. To date, studies that have examined the effectiveness of ICM among substance abusers have had mixed findings.11,14–17 Thus, in spite of the intuitive appeal, there is limited support for the hypothesis that longer-term care strategies and better service coordination actually improve treatment compliance and outcomes among substance abusers. No reported study has tested the effectiveness of ICM among substance-dependent women on TANF.
We conducted a randomized field trial to test the effectiveness of 2 models of care. Substance-dependent women were identified in welfare offices with routine self-report drug use screening procedures, which were part of determining TANF benefit eligibility. One group of women received referrals to a treatment program and welfare services (usual care [UC]). UC is often referred to as the “screen and refer” model and was the standard of care in New Jersey at the time of our study. The other group of women received ICM—coordinated social and health care services and long-term support and monitoring—in addition to the substance abuse treatment and other services available to the UC group.
METHODS
Participants
We worked with the case management agency to collect data on a sample of 302 substance dependent women on TANF as part of a welfare demonstration project. Participants were recruited from welfare offices in urban Essex County, New Jersey.
Eligibility criteria.
Formal selection criteria were (1) having a Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV )18 substance dependence diagnosis, (2) being TANF eligible, (3) having entered New Jersey’s welfare-to-work program and not been deferred for a medical problem, and (4) being able to speak English well enough to complete an interview. Women were excluded if they were psychotic, receiving or seeking methadone treatment, seeking long-term residential treatment, or were currently stably engaged in substance abuse treatment.
Recruitment.
Participants were recruited from September 1999 to May 2002. Welfare workers administered a brief screening measure—the CAGE-AID19—to all individuals who applied for or sought redetermination of TANF benefits in accordance with New Jersey state welfare regulations. Women who responded positively to 2 or more questions on the CAGE-AID were referred to trained addictions professionals at the welfare offices for further evaluation; the welfare workers then screened clients for study eligibility and obtained informed consent. Approximately 7% of welfare participants screened positive for substance use problems. We know screening in welfare settings does not capture everyone with substance use problems; therefore, we used methods designed to minimize reporting bias.20 Of the clients who screened positive, 47% (n = 280) did not meet eligibility criteria (e.g., receiving methadone treatment, no DSM-IV diagnosis), and 2.2% refused to participate. Thus, 95.9% (N = 302) of eligible participants were randomized (Figure 1 ▶).
FIGURE 1—
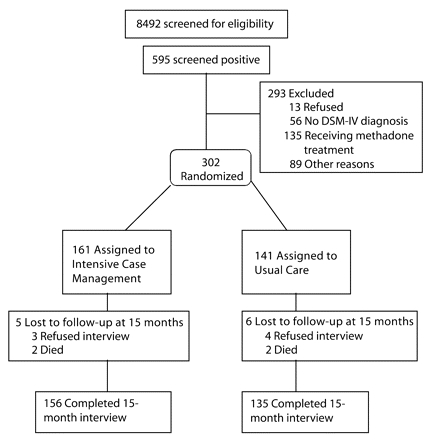
Flow of participants through the trial, including recruitment and randomization to treatment and control conditions.
Note. Number of clients screened, screened positive, and excluded for various reasons were estimated by an analysis of a representative 1-year period of screening, because screening records were not available for the entire recruitment period.
Study Interventions
Clinical staff for both treatment conditions (ICM and UC) were addiction counselors with master’s degrees. Women were randomly assigned to 1 of the 2 treatment conditions.
Intensive case management.
ICM was a manual-guided intervention ( J. M. et al., unpublished data, 1999) with 5 phases: (1) outreach and assessment; (2) planning, motivational enhancement, and treatment engagement; (3) treatment coordination, monitoring, and advocacy; (4) aftercare follow-up, peer support, and relapse monitoring; and (5) crisis management and termination. Women randomized to ICM met with a pair of case managers in a segregated clinical space at the local welfare office. During the first phase of ICM, case managers identified tangible barriers to treatment entry, including childcare, transportation, and housing problems, and provided needed services. Case managers also addressed clients’ resistance to entering treatment with motivational counseling strategies. If needed, case managers engaged in extensive outreach efforts, including home visits and contacting family members. Once clients entered treatment, case managers assisted treatment facility staff with coordinating needed services and met with clients weekly. Clients also received vouchers for purchasing items (e.g., children’s toys and cosmetics) as incentives for attending treatment. Case manager contact with clients was titrated and adapted on the basis of need and phase of treatment. For example, during periods of crisis, case managers often had daily contact, whereas if clients were compliant and stable, contact was reduced to 2 visits per month. Case management services were provided throughout the 15-month follow-up period.
Usual care.
UC was a screen and refer model and represented the standard of care in New Jersey at the time of our study. Although there are no national standards for substance abuse service delivery within welfare systems, as of 2000, every state reported having some type of substance abuse screening and referral system within their welfare departments.21 Women randomized into UC met with a clinical care coordinator, who reviewed their need for substance abuse treatment and the recommended level of care. Initial appointments were scheduled with treatment facility staff. Counselors contacted the treatment facility staff periodically to review clients’ progress and to authorize additional treatment, although a minimal amount of case monitoring was delivered proactively. When clients failed to attend a first session, outreach was limited to several phone calls and letters. Clients had the option of returning to be reassessed and assigned to treatment when initial treatment failed or at any time during the 15 months of study participation.
Measures
Baseline characteristics.
The alcohol and drug portions of the Addiction Severity Index–Expanded Female Version (ASI-F) were the core measure of baseline substance use and severity.22 The psychometric properties of the ASI-F have been validated in samples of substance-dependent women with children.22 The DSM-IV Structured Clinical Interview determined substance use diagnoses.23 The Level of Care Indicator—a clinician-administered measure that assesses the American Society of Addiction Medicine Patient Placement Criteria—evaluated the 4 levels of recommended treatment intensity (inpatient hospital, inpatient residential, intensive outpatient, or regular outpatient).24
Treatment attendance.
Treatment attendance data were provided to clinical staff each week, and the data were verified with the client during all in-person follow-ups. We used the National Commission for Quality Assurance’s Health Plan Employer Data and Information Set (HEDIS) 2004 benchmarks to designate phases of treatment, as suggested by the Washington Circle, to compare our findings with others.25 In accordance with these benchmarks, initiation was defined as an inpatient admission within the first 30 days or an outpatient service and any additional services within 14 days; engagement was defined as an intermediate step between initially accessing care and completing a full course of treatment, and it was defined as 2 additional days of treatment within 30 days after initiating treatment; and retention was defined as having successfully engaged in treatment and having attended at least 2 sessions of treatment during the third month after initiation of care.
Treatment fidelity and discriminability.
Treatment fidelity was assessed with 2 methods: supervisors’ periodic reviews of clinical cases and researchers’ reviews of clinical charts. A measure was designed for both methods that assessed which activities should occur during each of the 5 phases of case management, and a percentage of delivered activities was calculated. Treatment discriminability, i.e., being able to document that the experimental and control treatments were separate and did not overlap, was assessed with activity logs completed by the clinical staff. All clinical staff (ICM case managers and UC care coordinators) were required daily to log all activities relevant to a particular client, such as date of activity, ASI domain in which the activity was most related (alcohol/drugs, employment, housing, and so on), amount of time spent on the activity, and type of activity (in-person meeting with client, telephone call to coordinate services, and so on).
Outcome measures.
The Timeline Follow-back26 interview was the primary measure of substance use during the 15 months of the study. The Timeline Followback Interview involves collecting substance use data for each day from the last interview to obtain a continuous record of use and to construct a dichotomous measure of abstinence (abstinent or not) for each month of the 15-month follow-up period. Monthly rates of absolute abstinence were the primary outcome measure, because the participants were primarily dependent on opiates or cocaine, and the welfare, case management, and treatment systems focused on absolute abstinence rather than reduction of drug use as the goal.
Confirmation of self-reported data.
Self-reported alcohol and drug use data were confirmed using 2 methods: a collateral interview and urine screens. Collaterals’ reports and clients’ reports of use during the past 15 months were compared. Collaterals and clients were classified as having agreed when (1) both reported that the client used, (2) both reported the client had not used, or (3) the client reported use but the collateral did not. Agreement at 3-month, 9-month, and 15-month follow-ups ranged from 87.2% to 94.5% (k = 0.72–0.87). Testing of urine samples for the presence of illegal drugs (urine screens) were administered during all in-person follow-up interviews. Agreement between urine screens and self-reported substance use (defined as any outcome other than a positive urine screen but a negative self-report) ranged from 89.3% to 95.5% (k= 0.71–0.84). Thus, the data suggest that self-reported substance use was valid in our study. Although there may be some concern about the validity of urine screens for detecting some drugs (e.g., high rates for detecting marijuana but low rates for detecting cocaine), rates of agreement for both ICM and UC did not differ. Because rates of agreement were very high, self-reported data were considered valid and were not recoded on the basis of urine screening results or collateral verification.
Procedures
Clinicians conducted baseline assessments, and research staff conducted all follow-up interviews. All clinicians/interviewers had a bachelor’s or master’s degree and had experience assessing clients with substance use disorders. They received extensive training (50–75 hours) and were required to pass a rigorous certification process. Clinicians and research interviewers met together regularly with a doctoral-level researcher to prevent interviewer drift. Random assignment to ICM or UC was determined on the basis of random number generation and then put in a sealed envelope by the project director. The envelopes were opened after the baseline assessment was completed. This procedure ensured that clinicians were blind to the treatment condition while conducting the baseline assessment and that the possibility of cohort and treatment allegiance effects was minimized.
Participants received in-person follow-up interviews 3, 9, and 15 months after baseline assessment; 249 (82.4%) women completed the 3-month assessment, 261 (86.4%) completed the 9-month assessment, and 269 (89.1%) completed the 15-month assessment. Additionally, 25 women provided data during a subsequent follow-up at 24 months, so we had Timeline Followback interview data for the entire 15-month period. Consequently, 294 (97.4%) of the original sample had follow-up substance use data. Treatment attendance data were available for all participants during the 15-month period.
Data Analytic Plan
We assessed the equivalence of treatment conditions with t test statistics to examine whether the treatment conditions differed on any demographic or participant characteristic, and we used t tests to assess whether treatment conditions differed in dose of care management services received across the 15 months postbaseline. When variances differed significantly between the 2 treatment conditions, we conducted t tests for unequal variances. We used multivariate analysis of variance to assess differences in service receipt by ASI domain. Frequency percentages for treatment initiation and engagement rates were compared using χ2 analyses. We conducted repeated-measures analyses for categorical outcomes using generalized estimating equations27,28 to examine condition differences on dichotomous substance use outcomes within the context of other covariates, designating point prevalence abstinence for each of the 15 months as the dependent variable. Analyses were conducted using the PROC GENMOD function of SAS version 9.1 (SAS Institute Inc, Cary, NC), specifically the Logit link function and a compound symmetric correlation matrix. Baseline substance use severity was entered into the model as a covariate to control for the effects of a small number of participants who were abstinent during the month before baseline. Thus, independent variables for the generalized estimating equations included treatment condition, substance use severity, and a variable that carried the linear effect of time. Treatment conditions differed by marital status at baseline; however, we did not enter marital status into the model as a covariate because it was not related to outcome. We entered time by condition interaction into the second step of the model to assess if the strength of the effects changed over time.
RESULTS
Equivalence of Conditions at Baseline
Treatment conditions did not differ on the basis of demographics (income or education) or any of the baseline ASI Composite Scores (alcohol/drugs, family, employment, legal, medical, or psychiatric). However, we did find that ICM clients were older than UC clients. Consequently, we entered age into further analyses as a covariate.
Demographic Characteristics
Overall, most women were Black, aged 35 to 37 years, had not graduated from high school, had a median annual income of less than $10 000, and had received welfare benefits as an adult for an average of 12 years (Table 1 ▶). They also had an average of 3 to 4 children, most of whom were older than 5 years. The primary dependence diagnosis was for a hard drug (69.8%), either heroin or cocaine. Less than 5% of women were injection drug users (IDUs), because IDUs almost always were referred to methadone maintenance treatment. On average, women reported either drinking alcohol to intoxication or using illicit drugs on approximately two thirds of the days during the past month. On average, we found chronic patterns of problem substance use. For example, almost all women (99.1%) reported regular use of some substance, which was defined as at least 3 times a week for a year or longer, and on average, women reported using substances regularly for about 13 years. About one third of the women required inpatient detoxification or rehabilitation (21–28 days) before referral to outpatient care (on the basis of American Society of Addition Medicine Patient Placement Criteria).
TABLE 1—
Characteristics of Substance–Dependent TANF Women: Essex County, New Jersey, 1999–2002.
| Intensive Case Management (n = 161) | Usual Care (n = 141) | |
| Age, y | 37.00 | 35.48 |
| Race/ethnicity, % | ||
| Black | 95.65 | 95.74 |
| Hispanic | 3.73 | 2.13 |
| Other | .62 | 2.13 |
| Marital Status,* % | ||
| Married/living as married | 6.21 | .71 |
| Separated/widowed/divorced | 19.25 | 18.44 |
| Never married | 74.53 | 80.85 |
| Graduated from high school, % | 47.83 | 48.23 |
| Median income level,a $ | 5000–9999 | 5000–9999 |
| Welfare, yb ±SD | 12.90 (7.98) | 11.28 (7.44) |
| No. of children ±SD | 3.25 (1.82) | 3.16 (1.83) |
| Percentage with a child in each age group, y | ||
| 0–5 | 36.02 | 39.72 |
| 6–11 | 57.76 | 63.12 |
| 12–17 | 59.63 | 56.74 |
| Primary substance use diagnosis, % | ||
| Alcohol | 18.63 | 26.43 |
| Cocaine | 39.13 | 30.71 |
| Heroin | 37.27 | 35.00 |
| Marijuana | 4.97 | 7.86 |
| Drank/used drugs during past month, days (SD) | ||
| Alcohol | 7.77 (10.49) | 10.18 (12.35) |
| Heroin, cocaine | 14.23 (12.93) | 14.41 (13.16) |
| Marijuana, other | 3.40 (8.37) | 4.33 (9.40) |
| Regular heavy drinking/drug use, y (SD)c | ||
| Alcohol | 13.87 (8.46) | 12.44 (8.82) |
| Cocaine | 9.38 (6.23) | 9.24 (5.68) |
| Heroin | 7.40 (6.39) | 8.20 (5.92) |
| Marijuana | 9.77 (7.73) | 8.13 (6.76) |
| Any drug/alcohol | 13.01 (8.01) | 12.98 (7.50) |
| ASAM Initial Level of Care, % | ||
| Outpatient | 71.33 | 65.67 |
| Inpatient | 28.67 | 34.33 |
Note. ASAM = American Society of Addiction Medicine; TANF = Temporary Assistance for Needy Families.
aResponse format was $5000 increments.
bSelf-reported years on welfare since age 18 y.
cRegular use was defined as use at least 3 times per week for a year or longer.
*Conditions differed on marital status at the P < .05 level.
Treatment Discriminability and Fidelity
Fidelity to the ICM model was good; on average, clinical staff completed 70% of the required activities (SD = 18.8%). Discriminability between the treatment conditions was high (Table 2 ▶). ICM clients used care management services approximately twice as long as did UC clients across the 15-month period. Additionally, ICM clients had approximately 3 times as many direct contacts with their caseworkers compared with UC clients, and ICM case managers spent almost 5 times more time delivering services to ICM clients. ICM clients also received more minutes of services that addressed their ASI domain needs.
TABLE 2—
Treatment Fidelity and Discriminability
| Treatment Condition | ||||
| Intensive Case Management (ICM) (n = 161) | Usual Care (UC) (n = 141) | P | Effect Size | |
| Dose of care management services (SD) | ||||
| Direct contacts | 21.09 (17.57) | 7.13 (4.52) | .0001 | 1.06 |
| Duration/days in ICM or UC | 301.15 (143.00) | 182.33 (153.83) | .0001 | .80 |
| Dose/minutes in ICM or UC | 512.69 (461.69) | 111.29 (101.28) | .0001 | 1.17 |
| Care management services delivered by ASI domain, mean in minutes (SD) | ||||
| Alcohol | 221.53 (231.82) | 85.92 (67.15) | .0001 | .78 |
| Drug | 351.41 (322.45) | 100.76 (72.31) | .0001 | 1.04 |
| Family | 44.71 (63.46) | 15.32 (14.61) | .0001 | .62 |
| Legal | 40.04 (50.74) | 14.40 (12.47) | .0330 | .68 |
| Housing | 92.26 (161.72) | 15.10 (13.85) | .0001 | .65 |
| Employment | 122.58 (121.91) | 27.57 (24.67) | .0001 | 1.05 |
| Psychiatric | 29.79 (31.41) | 14.85 (13.79) | .0001 | .60 |
| Medical | 43.87 (67.50) | 15.62 (14.38) | .0001 | .56 |
| Care management addressing other issues in minutes (SD) | ||||
| Childcare | 35.52 (38.38) | 15.50 (13.45) | .0001 | .68 |
| Transportation | 65.97 (81.15) | 16.36 (14.46) | .0001 | .83 |
Notes. ASI = Addiction Severity Index. Differences between treatment conditions on dose of received care management were tested with t tests. Services received by ASI domain and services that addressed other issues were tested in 1 model with multivariate analysis of variance. Effect size calculations were determined on the basis of the difference in time spent in each domain between the largest and the smallest mean. Because of large differences in standard deviations, the unequal variance t test was conducted.
Treatment Retention and Engagement
There were significant differences between the treatment conditions on all substance abuse treatment benchmarks (Table 3 ▶). Significantly more ICM clients initiated treatment within the first 30 days, and ICM engagement rates were almost double those of UC rates. Retention rates were more than twice as high among ICM clients compared with UC clients, and ICM clients attended significantly more treatment days throughout the 15-month period. Rates for program completion (continuous attendance and completion of at least 1 outpatient treatment episode) also were almost twice as high among ICM clients than among UC clients.
TABLE 3—
Treatment Condition Differences in Performance Benchmarks During the 15 Months After Baseline Assessments
| Treatment Condition | ||||
| Measure/Variable | Intensive Case Management | Usual Care | P | Effect Size |
| Treatment for alcohol and other drugs | ||||
| Initiation | 66.46% | 50.35% | .0045 | .33 |
| Engagement | 60.25% | 34.04% | .0001 | .54 |
| Retention | 42.24% | 18.44% | .0001 | .53 |
| Completion of an outpatient program | 43.48% | 22.70% | .0001 | .45 |
Abstinence Outcomes
Results of the generalized estimating equations analysis showed that the likelihood of point prevalence abstinence (percentage of participants abstinent during the 1-month window) during months 1 through 15 were 75% higher among ICM clients than among UC clients (β=.56; SE=.18; odds ratio=1.75; 95% confidence interval=1.22, 2.51; P=.0025). We controlled for potential confounding influences across treatment conditions, and during both estimating equations. During the second step of the generalized estimating equation, we added interaction terms between treatment condition and time. The interaction was not significant (P=.11), which suggests that time did not moderate the effect of treatment condition on outcome. Figure 2 ▶ shows the percentage of clients who were abstinent during each of the 15 months by condition; by month 15, 43% of ICM clients were abstinent compared with 26% of UC clients.
FIGURE 2—
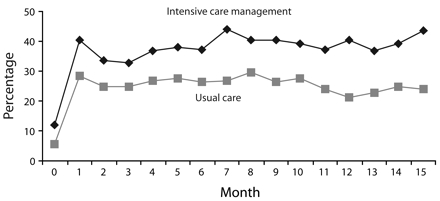
Percentage of clients who were abstinent during each month, by intervention condition.
Note. Month “zero” refers to the month preceding the study.
DISCUSSION
Overall Evidence
Our study provides experimental support for ICM as a strategy for engaging and retaining substance-dependent women on TANF in substance abuse treatment and for reducing their drug use during a relatively long follow-up period. A number of methodological features strengthen the internal validity of our study: (1) random assignment, (2) a carefully ascertained and relatively large sample, (3) well-documented treatment fidelity and discriminability, (4) external confirmation of self-reported illicit drug use, and (5) very high follow-up rates. Our study also exhibited good external validity, because (1) recruitment occurred in welfare offices with existing screening procedures for welfare eligibility, (2) sample refusal rates were low, and (3) the control condition was the standard of care in New Jersey. Our findings show that differences between ICM and UC were not only statistically significant but also clinically meaningful. Rates of treatment engagement, retention, and completion were 1.5- to 2.5-times greater among ICM clients than among UC clients. Moreover, during later months of follow-up, rates of abstinence were as much as 65% higher among ICM clients than among UC clients.
Interpretation
Overall, our results support the underlying assumptions of the ICM intervention model. Specifically, ICM facilitated access to tangible social services and provided psychological support to assist women with entering and remaining in treatment. Moreover, ICM provided long-term monitoring and support. Longer-term support was important for managing the chronic relapse nature of drug dependence. However, in spite of the superiority of ICM compared with UC, fewer than half of the ICM clients completed an episode of outpatient treatment or were abstinent in any given month. It is difficult to compare these rates with those of other treatment studies, because these women were identified through a screening process conducted in welfare offices and were not seeking treatment. Nevertheless, the outcomes were clearly modest in absolute terms and leave a great deal of room for improvement.
Generalizability
A limited number of studies have tested the effectiveness of case management among substance-dependent clients, and only a handful of these have involved random-assignment designs.29,30 Overall, support for case management has been modest, with only about half of the random-assignment studies reporting significant results. Reviews have questioned whether the modest findings may be the result of design flaws (e.g., small sample size) or a restriction in the scope of case management services.31 Our findings are the strongest to date in supporting the hypothesis that case management improves access, engagement, retention, and outcome among substance-dependent clients. The stronger support may be the result of a stronger design, a more consistent intervention, or the long duration of treatment. Only 1 other study has reported outcomes from an intensive intervention for substance-dependent women on TANF. That study, CASAWORKS—a multicomponent intervention that included case management—showed significant pre-improvement to postimprovement in drug use and employment with a single-group evaluation design.32
A number of study limitations should be noted. First, we applied a number of exclusion criteria, including psychosis, severe medical problems, and methadone treatment. Although some exclusion criteria were modeled on criteria that welfare agencies use for deferring clients from work eligibility (e.g., psychosis, severe medical problems), others were a practical factor in study design. Results from our study should generalize to work-eligible substance-dependent women on TANF; however, generalizability to methadone clients is unclear. Additionally, reporting bias in these populations does occur, and we know screening for substance use problems in welfare settings is only modestly effective.
Case management interventions are less standardized than other behavioral interventions, such as motivational interviewing or cognitive behavioral treatment. We used a manual-guided approach to ICM and provided an array of services. The extent to which our findings will generalize to other versions of case management is unclear. The effectiveness of case management also might vary on the basis of the population and the setting in which it is delivered. Importantly, our study was conducted in the context of welfare reform. The clients—who were not seeking substance abuse treatment—were identified within welfare offices with screening procedures that were codified by New Jersey statutes. It is unclear whether our results will generalize to the provision of ICM to patients already in treatment. Our findings are limited to access to care and substance use outcomes. It was beyond the scope of our study to examine the impact of ICM on other domains of functions, but these will be considered in future studies.
Finally, our findings do not provide a clear explanation about whether improvements in abstinence rates were the result of increased participation in substance abuse treatment or the independent effects of case management, or which aspects of ICM may have been effective. For example, recent findings have supported the effectiveness of more minimal long-term interventions that simply monitor substance-dependent clients during extended periods.33,34 Further research is needed.
Our findings have important implications for intervening with substance-dependent women on TANF. Many welfare settings have screening procedures for substance abuse at the time of benefit eligibility determination and procedures for assessing and referring substance-dependent clients to substance abuse treatment. Other welfare settings do not provide even this level of intervention, and very few welfare settings offer ICM. Our findings clearly support the effectiveness of ICM compared with existing models of care. Additionally, ICM is likely to be less expensive and more feasible to implement than other evidence-based behavioral or pharmacological interventions for substance dependence, because ICM augments existing treatment services and does not require dramatic changes to treatment program practices.
Our findings have implications for the delivery of care to the broader population of disadvantaged substance-dependent individuals, beyond women on TANF. The majority of clients in publicly funded substance abuse treatment programs are referred by social services, such as welfare, child welfare, and criminal justice agencies. These populations share a similar set of problems with the women in our sample (e.g., chronic drug problems, co-occurring disorders, poor social supports), and they face a fragmented service system that provides disconnected episodes of acute care. Further research is needed to determine whether ICM may be an effective intervention for this much larger population.
Acknowledgments
This study was supported with funding from the National Institute on Drug Abuse (grant 5 RO1 DA12256), the Administration for Children and Families, the Assistant Secretary for Planning and Evaluation (grant 90XP0002), and the New Jersey Department of Human Services (NJDHS).
The authors acknowledge the strong support of Annette Riordan and the Division of Family Development staff at NJDHS, as well as Len Feldman. We also acknowledge assistance from Wayne Wirta, Mollie Brodsky, Helen Raytek, and the staff at the National Council on Alcohol and Drug Dependence–New Jersey.
Human Participant Protection The Rutgers University and National Center on Addiction and Substance Abuse at Columbia University institutional review boards approved this study.
Peer Reviewed
Contributors J. Morgenstern, B. S. McCrady, and R. J. Pandina secured the initial funding. J. Morgenstern and B. S. McCrady supervised all aspects of the study’s implementation and conducted the data analysis with input from the other authors. K. A. Blanchard, K. H. McVeigh, and T. J. Morgan supervised data collection and fidelity monitoring. All authors originated ideas, interpreted findings, and reviewed drafts of the article.
References
- 1.Gotham HJ, Sher KJ. Children of alcoholics. In: Kinney J, ed. Clinical Manual of Substance Abuse. 2nd ed. New York, NY: Mosby; 1996:272–287.
- 2.McGue M. Genes, environment, and the etiology of alcoholism. In: Zucker R, Boyd G, Howard J, eds. The Development of Alcohol Problems: Exploring the Biopsychological Matrix of Risk. Rockville, Md: National Institute on Alcohol Abuse and Alcoholism; 1994: 1–40.
- 3.Russell M. Prevalence of alcoholism among children of alcoholics. In: Windle M, Searles J, eds. Children of Alcoholics: Critical Perspectives. New York, NY: Guilford; 1990:9–38.
- 4.Kost KA, Smyth NJ. Two strikes against them? Exploring the influence of a history of poverty and growing up in an alcoholic family on alcohol problems and income. J Soc Serv Res. 2002;28:23–52. [Google Scholar]
- 5.Metsch LR, Pollack HA. Welfare reform and substance abuse. Milbank Q. 2005;83:65–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Adelmann PK. Mental and substance use disorders among Medicaid recipients: prevalence estimates from two national surveys. Adm Policy Ment Health. 2003;31:111–129. [DOI] [PubMed] [Google Scholar]
- 7.Fox K, Merrill JC, Chang HH, Califano JA Jr. Estimating the cost of substance abuse to the Medicaid hospital care program. Am J Public Health. 1995;85: 48–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olsen K, Pavetti L. Personal and Family Challenges to the Successful Transition From Welfare to Work. Washington, DC: US Dept of Health and Human Services; 1996.
- 9.Kline A, Bruzios C, Rodriguez G, Mammo A. Substance Abuse Needs Assessment Survey of Recipients of Temporary Assistance for Needy Families (TANF). Trenton, NJ: New Jersey Dept of Health; 1998.
- 10.Beckmann MP, Betsholtz C, Heldin CH, et al. Comparison of biological properties and transforming potential of human PDGF-A and PDGF-B chains. Science. 2000;77:34–38. [DOI] [PubMed] [Google Scholar]
- 11.Brindis CD, Theidon KS. The role of case management in substance abuse treatment services for women and their children. J Psychoactive Drugs. 1997; 29:79–88. [DOI] [PubMed] [Google Scholar]
- 12.McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–1695. [DOI] [PubMed] [Google Scholar]
- 13.Morgenstern J, McCrady BS, Blanchard KA, McVeigh KH, Riordan A, Irwin TW. Barriers to employability among substance dependent and non-substance abusing women on federal welfare: implications for program design. J Stud Alcohol. 2003;64: 239–246. [DOI] [PubMed] [Google Scholar]
- 14.Homan SM, Flick LH, Heaton TM, Mayer JP, Klein M. Reaching beyond crisis management: design and implementation of extended shelter-based services for chemically dependent homeless women and their children. Alcohol Treatment Q. 1993;10:101–112. [Google Scholar]
- 15.Jessup M, Soman L. Models of Case Management for Pregnant and Parenting Addicted Women and Their Families: A Report of the Case Management Models Project. Sacramento, Calif: Department of Alcohol and Drug Programs; 1994.
- 16.Laken MP, Ager JW. Effects of case management on retention in prenatal substance abuse treatment. J Drug Alcohol Abuse. 1996;22:439–448. [DOI] [PubMed] [Google Scholar]
- 17.Pavetti L, Olsen K, Pindus N, Pernas M. Designing Welfare-to-Work Programs for Families Facing Personal or Family Challenges: Lessons From the Field. Washington, DC: Urban Institute; 1997.
- 18.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994.
- 19.Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252:1905–1907. [DOI] [PubMed] [Google Scholar]
- 20.Morgenstern J, Riordan A, Dephilippis D, et al. Specialized screening approaches can substantially increase the identification of substance abuse problems among welfare recipients. Report prepared for the US DHHS Administration for Children and Families; 2001. Available at: http://aspe.hhs.gov/hsp/njsard00/screening-rn.htm. Accessed January 2001.
- 21.Brown R. Addressing substance abuse and mental health problems under welfare reform: state issues and strategies. Paper presented at: meeting of the National Governors Association; June 30, 2001; Washington, DC.
- 22.Center for Substance Abuse Treatment. Supplementary Administration Manual for the Expanded Female Version of the Addiction Severity Index (ASI) Instrument: The ASI-F. Washington, DC: Government Printing Office; 1997. DHHS publication no. SMA 96–8056.
- 23.First MG, Spitzer RL, Gibbon M. Structured Clinical Interview for DSM-IV. New York, NY: Biometric Department, State Psychiatric Institute; 1996.
- 24.Gastfriend RA. Patient placement criteria and their relation to access to appropriate level of care and engagement in alcoholism treatment. Recent Dev Alcohol. 2001;15:157–176. [DOI] [PubMed] [Google Scholar]
- 25.The Washington Circle. Specification of performance measures for the identification, initiation, and engagement of alcohol and other drug services. Available at: www.washingtoncircle.org. Accessed April 2004.
- 26.Sobell L, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. Br J Addict. 1988;83: 393–402. [DOI] [PubMed] [Google Scholar]
- 27.Liang K-Y, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73: 13–22. [Google Scholar]
- 28.Zeger SL, Liang K-Y. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 29.McLellan AT, Grissom GR, Zanis D, et al. Problem-service ‘matching’ in addiction treatment. Arch Gen Psychiatry. 1997;54:730–735. [DOI] [PubMed] [Google Scholar]
- 30.McLellan AT, Hagan TA, Levine M, et al. Supplemental social services improve outcomes in public addiction treatment. Addiction. 1998;93:1489–1499. [DOI] [PubMed] [Google Scholar]
- 31.Stahler GJ, Shipley TFJ, Bartelt D, DuCette JP, Shandler IW. Evaluating alternative treatments for homeless substance-abusing men: outcomes and predictors of success. J Addict Dis. 1995;14:151–167. [DOI] [PubMed] [Google Scholar]
- 32.Morgenstern J, Nakashian M, Woolis DD, Gibson F, Bloom N, Kaulback BG. CASAWORKS for families: a new treatment model for substance abusing parenting women on welfare. Eval Rev. 2003;27:583–596. [DOI] [PubMed] [Google Scholar]
- 33.Dennis ML, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Eval Program Planning. 2003;26:339–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone based continuing care for alcohol and cocaine dependence: 24-month outcomes. Arch Gen Psychiatry. 2005;62:199–207. [DOI] [PubMed] [Google Scholar]


