Abstract
Objectives. We explored changing relations between substance use, welfare receipt, and substance-abuse treatment among low-income mothers before and after welfare reform.
Methods. We examined annual data from mothers aged 18 to 49 years in the 1990–2001 National Household Survey of Drug Abuse and the 2002 National Survey of Drug Use and Health. Logistic regression was used to examine determinants of treatment receipt.
Results. Among low-income, substance-using mothers, the proportion receiving cash assistance declined from 54% in 1996 to 38% in 2001. The decline was much smaller (37% to 31%) among low-income mothers who did not use illicit substances. Low-income, substance-using mothers who received cash assistance were much more likely than other low-income, substance-using mothers to receive treatment services. Among 2002 National Survey of Drug Use and Health respondents deemed “in need” of substance-abuse treatment, welfare recipients were significantly more likely than nonrecipients to receive such services (adjusted odds ratio=2.31; P<.05). Controlling for other factors, welfare receipt was associated with higher prevalence of illicit drug use. Such use declined among both welfare recipients and other mothers between 1990 and 2001.
Conclusions. Welfare is a major access point to identify and serve low-income mothers with substance-use disorders, but it reaches a smaller proportion of illicit drug users than it did prereform. Declining welfare receipt among low-income mothers with substance abuse disorders poses a new challenge in serving this population.
During the 1996 welfare reform debate, many policymakers and analysts worried that the proposed legislation would harm low-income mothers who used illicit drugs, and would have even more profound effects on those dependent on these substances or on alcohol.1,2 We examined these issues, focusing on 3 specific concerns: (1) trends in illicit drug use by welfare recipients (and nonrecipients) over the period that includes the 1996 reforms, (2) trends in welfare receipt by illicit drug users (and nonusers) over the same period, and (3) treatment receipt among welfare recipients (and others) after welfare reform.
First, we extended previous trend analyses on the reported prevalence of illicit substance use among welfare recipients and other low-income mothers, before and after the 1996 Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA) with data from the 1990–2001 National Household Survey of Drug Abuse (NHSDA) and its successor, the National Survey of Drug Use and Health (NSDUH). Second, we examined the relation between welfare receipt and participation in substance-abuse treatment among mothers aged 18 to 49 years in the 2002 NSDUH. Third, we examined the prevalence of substance-use-related symptoms among low-income mothers who did not satisfy substance abuse or dependence criteria, but who may have experienced some difficulties that they attributed to substance use.
Background and Significance
The 1996 welfare reform act3–5 abolished a 60-year entitlement, Aid to Families With Dependent Children (AFDC), replacing it with the avowedly transitional Temporary Assistance to Needy Families (TANF). PRWORA allowed states broad leeway to impose more stringent requirements and time limits than federal law required, and enacted strong requirements for states to quickly move recipients into paid employment.3,6,7
Temporary Assistance to Needy Families caseloads declined by 60% between 1996 and 2003.4,8,9 Journalists, researchers, and policymakers have argued that many who continue to receive TANF face personal barriers that hinder self-sufficiency.10 Indeed, “leaver studies” indicate that recipients who exit the TANF rolls have more favorable job characteristics than do those remaining on the rolls.5,11,12
Political advocates for low-income families expressed particular fear that welfare recipients experiencing substance-use disorders would have special difficulties and would be especially likely to be penalized by restrictions imposed in welfare reform. PRWORA permitted chemical drug testing, allowed states to deny benefits to adults convicted of drug felonies, and allowed states to terminate benefits to illicit drug-using women (along with others) who violated program requirements or who simply failed to find employment.13 Consistent with these fears, studies indicated that substance-use disorders were especially prevalent among recipients sanctioned for noncompliance with TANF rules.14,15
Several studies have examined the prevalence and type of substance use among welfare recipients. Metsch and Pollack summarized much of the existing literature on pre- and postreform substance-use trends among TANF recipients.7 Although much of the peer-review published literature relies upon data that predate welfare reform,16–18 a growing body of research explores substance-use disorders in the postreform TANF population.19–28
A significant literature explores screening and assessment practices in welfare agencies. After the reform, many welfare agencies intensely focused on efforts to move recipients from welfare to work, with less attention paid to diverse barriers,11 including substance-use disorders,24,29 domestic violence,21 and other personal or psychosocial barriers to self-sufficiency.22,25 Surprisingly few TANF recipients with substance-use disorders are successfully identified and referred to treatment by TANF administrative systems.24
Findings from the 1998 NHSDA and other surveys indicated that approximately one fifth of adult TANF recipients reported illicit drug use in the previous year. Among mothers aged 18 to 49 years, TANF recipients were about twice as likely as nonrecipients to report recent illicit substance use.30 Marijuana was the most commonly reported illicit drug used by TANF recipients. Yet about half of illicit substance users reported use of at least 1 other illicit drug during the previous year.16,30 About 5% of TANF recipients in the 1998 NHSDA satisfied criteria for drug dependence; 7.5% satisfied criteria for alcohol dependence.17,18
PRWORA also changed the programmatic setting for low-income mothers who use alcohol or illicit substances. For state governments, the welfare reform act’s explicit time limits and emphasis on rapid transitions into paid work provided strong incentives for welfare agencies to detect work barriers (including substance-use disorders) facing TANF recipients. For applicants and clients, the welfare reform act’s emphasis on detection posed new risks, because identified parental substance abuse and dependence—and sometimes mere use—is a strong criterion for child protective intervention. Such rules may have deterred some income-eligible mothers from applying. The welfare reform act may also have provided greater incentive for recipients to enter treatment, because treatment participation satisfies work requirements in some states.
Recent analyses have explored the impact of substance use and use disorders on the probability that women with children would enter or exit systems of public cash aid.11,18,31 Surveys conducted before and after the welfare reform act found that adult welfare clients were more likely than other low-income women to satisfy Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition32 criteria for illicit drug abuse and dependence.17,30,33 Linkages appeared weaker and were less statistically significant between welfare receipt and alcohol disorders, though point estimates again suggest higher prevalence among TANF recipients. Mainly on the basis of prereform data, substance-use disorders have been identified as a barrier to both employment and to successful completion of education and training interventions.7,34
Substance-use disorders affect many low-income mothers who are not on the current TANF rolls. It is also the case that current recipients are only a fraction of those who will experience economic need or who will receive welfare at some period as either children or adults. Forty percent of all Americans born between 1970 and 1972, including 80% of African American children born during these years, experienced some welfare receipt during childhood.35 If one is concerned with the full effects of welfare reform on low-income mothers, its effects on current recipients and effects on other, potential recipients must both be considered.
Little attention has been paid to substance abuse and dependence in this broader population. For want of a better term, we refer to low-income mothers who abuse or who are dependent upon illicit substances as low-income, substance-abusing mothers. In like fashion, we refer to the group of low-income mothers who use illicit substances as low-income, substance-using mothers. We are mindful of dangers and costs associated with the use of acronyms to describe any group.
METHODS
Data and Methodology
This paper uses the 1990–2001 NHSDA and the 2002 NSDUH to examine prevalence of substance use, abuse, and dependence and substance-abuse treatment participation among low-income mothers and TANF recipients after welfare reform. These datasets include information regarding substance use, psychiatric disorders (including substance abuse and dependence), welfare receipt, and substance-abuse treatment participation during the 12 months before the survey interview.
Although the NHSDA and NSDUH surveys share common features, NSDUH included methodological improvements that appear to have increased response rates and that may have increased validity of survey responses. The forbidding term “drug abuse” was dropped from the survey title. The NSDUH increased respondent payments, and also introduced new procedures and interviewer training protocols to increase uniformity of survey responses.36 Both NHSDA and NSDUH are annual weighted and stratified surveys of the civilian noninstitutionalized US population, including residents of homeless shelters. We used Stata software (StataCorp LP, College Station, Tex) to perform statistical estimation, and used its “svy” routines to account for weighting and stratification. We focused our analysis on women aged 18 to 49 years who were pregnant or caring for children. This is the primary group of interest in welfare policy debate.
In Figures 1 ▶ and 2 ▶, we show trend data computed from 1990–2001 NHSDA data. These data provide the most consistent survey methodology to examine changes over time. The 2002 NSDUH provided the main data set for our cross-sectional analyses, because it likely provides improved data and response rates compared with NHSDA. We did not use the 2002 NSDUH data for trend analysis because methodological changes led to apparent trend discontinuities.
FIGURE 1—
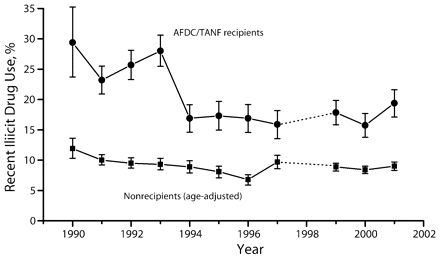
Past-year illicit drug use among welfare recipient and nonrecipient mothers aged 18–49 years.
Source. 1990–2001 National Household Survey of Drug Abuse.
FIGURE 2—
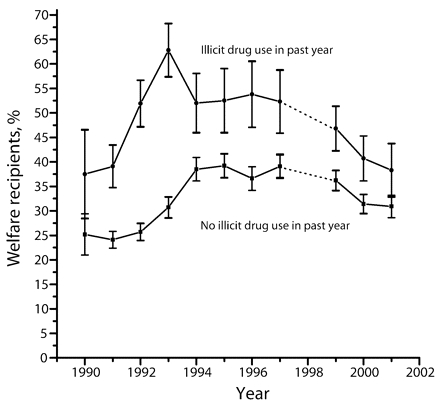
Welfare receipt among low-income mothers aged 18 to 49 years.
Source. 1990–2001 National Household Survey of Drug Abuse.
We examined 3 alternative measures of the prevalence and severity of substance use among low-income mothers: (1) illicit drug use, separating marijuana and nonmarijuana use in each year, (2) alcohol and drug dependence, and (3) substance abuse.37
Our NHSDA and NSDUH data are derived from survey responses rather than from clinical evaluation of respondents for substance-use disorders. Previous research indicated that well-administered household surveys have high interrater reliability and validity compared with clinical measures. The most detailed research has been conducted using the widely used Composite International Diagnostic Interview (CIDI).38,39
Like the NHSDA and NSDUH surveys, CIDI operationalizes Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV ) criteria for dependence and abuse.37 Concordance between CIDI and other diagnostic instruments appears notably stronger for measures of substance dependence than for measures of harmful use.40 Pollack et al.39 cited the literature on the “short-form” CIDI, which bears especially close similarity to the post–2000 NHSDA and the NSDUH implementation. Although survey data have been validated at the population level, responses are subject to both type 1 and type 2 error. Attenuation bias may lead us to understate the importance of use disorders in multivariate analysis of specific outcomes. Our trend analysis focused exclusively upon substance use. The NHSDA survey did not operationalize abuse and provided no standardized trend dependence before the year 2000.
We defined low-income, substance-abusing mothers as women who live with minor children, who satisfy survey criteria for substance abuse or dependence, and who have family incomes less than $20000 in year-2002 dollars. Unfortunately, NHSDA and NSDUH survey incomes are coded in wide and discrete nominal dollar categories. We therefore could not construct a fully consistent time-series with constant income thresholds adjusted for inflation. Before 1998, we could divide family income into discrete categories that included nominal dollar cutoffs at $15000 and $20000. After 1998, the income variable indicated only that income is less than $20000, with no correction possible for inflation. For consistency, we used a $20000 nominal dollar cutoff for all years. (Applying a $15000 cutoff for 1990–1996 data and a subsequent $20000 cut-off produced similar patterns, so we believe we have captured 1990–2002 trends well.)
Because access to substance-abuse treatment is of policy concern, we also explored treatment receipt among individuals deemed “in need” of such services. Individuals are deemed to require treatment if they satisfy criteria for substance abuse or dependence, or if they report receipt of treatment services during the previous year. Some individuals who report recent treatment receipt do not satisfy criteria for substance abuse or dependence. Consistent with previous NHSDA analyses, we considered these individuals to be in need of treatment services. These individuals were likely to have been in need at treatment entry, though some may have entered because of other reasons, such as legal difficulties following arrest, rather than specific problems rooted in substance abuse or dependence.
Neither NHSDA nor NSDUH survey was specifically designed to address welfare policy.41–43 We therefore tested whether the surveys showed differential nonresponse among welfare recipients or experienced underreporting of welfare receipt. Estimates of welfare receipt drawn from NHSDA and NSDUH tracked well the average AFDC/TANF enrollments reported by program administrators over the survey period.8 (Results are available from the authors.)
RESULTS
Prevalence of Substance Use and Use Disorders
In all years, illicit drug use was more than twice as common among AFDC/TANF recipients as among mothers who did not receive cash aid.7,39 Figure 1 ▶ reports trends, comparing AFDC/TANF recipients with an age-matched comparison group. As mentioned, methodological differences between the NSDUH and NHSDA surveys led us to end our trend analysis at the year 2001.36 (Analysis of 2002 and preliminary analysis of 2003 NSDUH data indicated a slight increase in reported prevalence between 2001 and 2002 accompanying the changed survey methodology, with a slight subsequent decline in reported prevalence between 2002 and 2003.) Note that 1998 data are unavailable because of our inability to identify mothers with dependent children consistently with other years. For each group, we include 95% confidence intervals, computed with the “ci” procedure in the Stata Version 9.0 software package (StataCorp LP, College Station, Tex).
Both groups reported substantial declines in illicit drug use between 1990 and 1996, then stable rates between 1996 and 2001. Prevalence among welfare recipients was always substantially and significantly higher than among nonrecipients. In bivariate and multivariate trend comparisons, we found no absolute or relative increase in prevalence disparities by welfare receipt between 1990 and 2001. A χ2 test indicated that the prevalence of substance use among welfare recipients was higher in 1990 than in 2001 (χ12=4.94; P<.03).
Figure 2 ▶ displays welfare receipt among low-income illicit drug users and nonusers over the same period. We again included error bars to indicate 95% confidence intervals. Although illicit drug users were more likely to receive AFDC and then TANF in all years, welfare receipt declined much more rapidly among illicit drug users (from 54% in 1996 to 38% in 2001) than among nonusers (from 37% to 30%) after the 1996 reforms.
Although substance use and use disorders were uncommon among welfare recipients, many mothers who did use illicit substances or who satisfied criteria for abuse or dependence had received AFDC or TANF cash aid. Despite the significant postreform contraction in TANF caseloads, 31.7% of low-income, substance-abusing mothers in the 2002 NSDUH sample had received TANF aid. In the previous 12 months, welfare receipt among low-income, substance-abusing mothers was quite similar to welfare receipt observed (30.6%) among other low-income mothers.
Table 1 ▶ provides detailed descriptive statistics on the current TANF caseload, using the 2002 NSDUH. It consists of 4 panels, each with 2 columns. The first 3 panels compare substance use characteristics of recipient and nonrecipient mothers aged 18–49. The fourth panel compares the fraction of users satisfying at least one abuse or dependence criterion in each population. The first 2 columns also include the pertinent number of NSDUH respondents in each category. Two categories were dropped from the analysis: Only 4 TANF recipients reported sedative use in the past year and only 7 TANF recipients reported inhalant use during the past year.
TABLE 1—
Substance Use (%) Among Women Aged 18 to 49 Years Who Live With Minor Children, by Substance Use Disorders and Temporary Assistance to Needy Families Receipt
| Used in Past Year (n) | Satisfy Abuse or Dependence Criteria | Meet at Least 1 Criterion for Abuse or Dependence | Used in Past Year and Meet at Least 1 Criterion for Abuse or Dependence | |||||
| Nonrecipients | Recipients | Nonrecipients | Recipients | Nonrecipients | Recipients | Nonrecipients | Recipients | |
| Alcohol | 69.1*** (5840) | 61.7 (873) | 5.35 | 6.46 | 19.9*** | 28.2 | 28.6*** | 45.1 |
| Alcohol or any illicit drug | 70.1** (5962) | 64.8 (903) | 6.6*** | 10.4 | 22.7*** | 33.8 | 32.1*** | 51.8 |
| Any illicit drug | 12.8*** (1418) | 22.3 (333) | 1.8*** | 5.1 | 5.6*** | 12.5 | 44.0* | 55.9 |
| Marijuana | 8.0*** (1000) | 14.4 (249) | 0.81*** | 2.0 | 3.1*** | 6.4 | 38.8 | 44.2 |
| Cocaine | 1.5*** (191) | 4.0 (49) | 0.4* | 0.9 | 0.9*** | 2.5 | 55.4 | 60.6 |
| Analgesics | 4.5* (483) | 6.4 (106) | 0.66 | 1.39 | 1.6** | 3.5 | 36.0* | 53.8 |
| Tranquilizers | 2.0 (206) | 2.7 (41) | 0.2 | 0.5 | 0.7** | 1.8 | 40.9 | 49.4 |
| Stimulants | 1.3** (141) | 2.9 (40) | 0.12 | 0.6 | 0.5 | 0.9 | 36.9 | 29.4 |
| Hallucinogens | 1.1* (194) | 1.8 (46) | 0.1* | 0.3 | 0.4 | 1.0** | 32.3* | 55.8 |
Source. Data are from the 2002 National Survey of Drug Use and Health.
*P < .05; **P < .01; ***P < .001 (differences between Temporary Assistance to Needy Families recipients and others).
For every substance except alcohol, TANF recipients were more likely than nonrecipients to report recent use. Differences were statistically significant (P < .05) for all of these substances, except tranquilizer use. Some illicit drug use over the previous year was reported by 22.3% of TANF recipients, compared with 12.8% of nonrecipients (P < .001). Marijuana was by far the most prevalent form of illicit substance use. However, 6.4% of TANF recipients reported analgesic use and 4.0% reported cocaine use. The TANF recipients were 7 percentage points less likely than nonrecipients to report alcohol consumption during the past year.
The TANF recipients were also more likely than nonrecipients to satisfy NSDUH criteria (which were based on DSM-IV criteria37) for dependence or abuse. Abuse or dependence criteria for some substance were satisfied by 10.4% of TANF recipients and 6.6% of nonrecipients. Criteria for illicit drug dependence or abuse were satisfied by 5.1% of TANF recipients, a significantly greater percentage (P < .001) than the 1.8% prevalence observed among nonrecipients. Differences in alcohol disorders were much smaller and statistically insignificant: 6.5% of TANF recipients, compared with 5.4% of nonrecipients.
Less than a quarter of women who reported recent illicit drug use satisfied explicit criteria for abuse or dependence. Yet a notable minority of users did report specific economic, social, or family difficulties that they attributed to substance use. Twenty-eight percent of TANF recipients reported at least 1 alcohol-related difficulty. Among nonrecipients, 19.9% reported the same symptoms (P<.001).
Because illicit drug use was less common than alcohol use, less than 10% of all respondents indicated any problem attributable to illicit drugs. However, about half of all mothers who reported actual use of illicit drugs reported some related difficulties (55.9% among TANF recipients, 44.0% among nonrecipients; P<.05). Consistent with findings in previous research, respondents who had recently used an illicit drug were more likely than others to report alcohol-related difficulties.
Treatment Receipt
In our 2002 data, only 7.1% of women who satisfied criteria for substance dependence or abuse reported that they had received substance-abuse treatment services during the previous 12 months. The TANF recipients in our sample who satisfied abuse or dependence criteria were more likely than others (11.9% compared with 6.2%; P < .08) to receive treatment services. The TANF recipients accounted for an estimated 34% of treatment clients (and represented an estimated 9.5% of the overall population) within our NSDUH sample. Almost half (46.7%) of low-income, substance-using mothers who received treatment in the past year also received TANF. As mentioned, trend data regarding low-income, substance-using mothers are unavailable before the year 2000 because the NHSDA did not consistently operationalize dependence and did not operationalize abuse before that survey wave.
In 1993, more than 60% of mothers who reported recent use of illicit drugs had received TANF aid, compared with 31% of other low-income sample mothers. Our NSDUH data indicated rather similar observed welfare receipt in the 2 groups by 2002. Among low-income mothers who reported no illicit substance use, 29.6% had received TANF cash aid, compared with 35.3% of those who reported recent use of an illicit substance.
Table 2 ▶ shows results of a multivariate model for all mothers deemed in need of treatment. (As a robustness check, we excluded women who received treatment but did not satisfy abuse or dependence criteria. We obtained slightly smaller point estimates but the same qualitative conclusions.) The baseline plus dependence columns add controls for dependence on specific substances. Few variables other than TANF receipt were statistically significant. African Americans, Hispanics/Latinos, and respondents outside metropolitan statistical areas were less likely than others to receive treatment services. Perhaps surprisingly, low income was associated with increased treatment receipt. Cocaine disorders were associated with an increased probability, and stimulant disorders are associated with a decreased probability of treatment receipt.
TABLE 2—
Logistic Regression Analysis of Treatment Receipt by Mothers Aged 18 to 49 Years in Need of Treatment
| All Mothers, Adjusted Odds Ratio (95% Confidence Interval) | Low-Income Mothers,Adjusted Odds Ratio (95% Confidence Interval) | |||
| Baseline Specification (n = 898) | Baseline + Dependence (n = 898) | Baseline Specification (n = 306) | Baseline + Dependence (n = 306) | |
| Direct TANF receipt | 2.45** (1.15, 5.23) | 2.62** (1.18, 5.81) | 2.31** (1.04, 5.16) | 2.31** (1.02, 5.24) |
| High-school graduate | 0.64 (0.34, 1.19) | 0.69 (0.37, 1.31) | 1.29 (0.55, 3.02) | 1.49 (0.64, 3.50) |
| Mother younger than 21 y | 0.78 (0.43, 1.42) | 0.77 (0.42, 1.41) | 2.14* (0.93, 4.92) | 2.08 (0.86, 5.01) |
| Mother aged 35 to 49 y | 0.81 (0.41, 1.58) | 0.73 (0.37, 1.45) | 1.20 (0.44, 3.31) | 1.22 (0.43, 3.46) |
| Race/ethnicity | ||||
| Non-Hispanic White | Referent | Referent | Referent | Referent |
| African American | 0.61 (0.28, 1.35) | 0.53 (0.22, 1.25) | 0.84 (0.28, 2.47) | 0.78 (0.25, 2.48) |
| Hispanic/Latino | 0.66 (0.23, 1.91) | 0.53 (0.17, 1.67) | 0.32* (0.09, 1.08) | 0.26* (0.07, 1.04) |
| Other race/ethnicity | 1.23 (0.50, 3.03) | 1.30 (0.53, 3.17) | 1.89 (0.68, 5.25) | 2.17 (0.74, 6.36) |
| Metropolitan statistical area | ||||
| More than 1 million people | 0.67 (0.33, 1.33) | 0.65 (0.32, 1.32) | 0.91 (0.35, 2.33) | 1.035 (0.38, 2.79) |
| Fewer than 1 million people | Referent | Referent | Referent | Referent |
| Non-metropolitan statistical area | 0.45** (0.23, 0.86) | 0.43** (0.22, 0.85) | 0.53 (0.21, 1.33) | 0.57 (0.21, 1.53) |
| Number of children | ||||
| 1 | Referent | Referent | Referent | Referent |
| 2 | 0.55* (0.28, 1.08) | 0.51* (0.26, 1.01) | 0.94 (0.34, 2.62) | 0.86 (0.31, 2.35) |
| 3 or more | 1.08 (0.52, 2.27) | 1.12 (0.52, 2.42) | 2.39* (0.94, 6.07) | 2.24 (0.85, 5.96) |
| Mother pregnant at interview | 0.56 (0.16, 1.88) | 0.48 (0.16, 1.42) | 0.62 (0.19, 2.02) | 0.73 (0.22, 2.44) |
| Substance abuse/dependence | ||||
| Alcohol | Referent | Referent | Referent | Referent |
| Cocaine | 4.39*** (1.65, 11.67) | . . . | 2.54 (0.55, 11.74) | |
| Marijuana | . . . | 0.62 (0.32, 1.23) | . . . | 0.53 (0.21, 1.35) |
| Stimulant | . . . | 0.06** (0.006, 0.61) | . . . | 0.42 (0.02, 9.96) |
| Analgesic | . . . | 0.67 (0.12, 3.82) | . . . | 4.73 (0.38, 59.53) |
| Psychotropic | . . . | 1.44 (0.29, 7.11) | . . . | 0.22 (0.02, 2.33) |
| Other (heroin, hallucinogen, sedatives) | . . . | 1.57 (0.32, 7.81) | . . . | 1.85 (0.17, 19.72) |
| Income less than $20 000 | 1.92** (1.01, 3.64) | 1.82* (0.96, 3.48) | . . . | . . . |
| Model diagnostics | ||||
| F statistic | F13 885 = 2.93 | F19 879 = 2.44 | F12 294 = 1.96 | F18 288 = 1.82 |
| P | P < .001 | P < .001 | P = .03 | P = .02 |
Source. Data are from the 2002 National Survey of Drug Use and Health.
Note. TANF = Temporary Assistance to Needy Families. Mother were considered in need of treatment if they satisfied criteria for substance abuse or dependence or reported receipt of treatment services during the previous year.
*P < .10; **P < .05; ***P < .01.
In both the baseline and baseline plus dependence specifications, TANF receipt was associated with a large and significant increase in the probability of treatment. After controlling for specific confounders, TANF receipt was associated with an adjusted odds ratio of 2.45 in our baseline specification. The adjusted odds ratio slightly increased when substance of abuse was accounted for. Among mothers in need of treatment, TANF recipients were more likely to report abuse or dependence of illicit drugs other than marijuana, and were less likely to be alcohol-dependent than were nonrecipients. The second pair of columns in Table 2 ▶ restricts the analysis to low-income mothers who satisfy abuse or dependence criteria. TANF receipt is again associated with increased treatment receipt, though the adjusted odds ratio of 2.31 is slightly smaller than was found in the broader sample.
DISCUSSION
Study Limitations
Our study had several limitations. Our self-reported data were vulnerable to under-reporting of both substance use and treatment receipt.44 The NHSDA survey is known to underrepresent frequent use of cocaine and heroin, and to underrepresent the overall volume consumed of both substances.43,45,46 Fendrich and colleagues found that the majority of women who tested positive for heroin and cocaine in hair, urine, or saliva tests did not reveal their use of these substances.46 Responses regarding marijuana appeared more complete in these data.
Our data did not allow analysis of plausible intergenerational or lagged effects. Because we did not have panel data, we also could not scrutinize causality issues that deserve attention. Substance abuse treatment facilities may provide an outreach mechanism to enroll some low-income women into TANF, creating an issue of reverse causality for our analysis. We suspect that this issue is more pressing for data collected after the 1996 welfare reform act. The TANF enrollment and retention requirements are more stringent than pertained for AFDC, so professional assistance with such matters may be correspondingly more valuable.7,33,39
We also lacked data on specific state policies or implementation details for both TANF and substance-abuse treatment. Many studies (e.g., Pavetti and Bloom47) have identified the importance of such factors.47 Our statistical results indicated that urban respondents were more likely than otherwise comparable rural respondents to receive treatment services. Such findings may suggest differential access to treatment services.
Survey methodology posed other obstacles. Over the 1990s, NHSDA used varying operationalization of important demographic variables, including family income, welfare participation, and the age and number of dependent children in the household. We believe that we have constructed consistent subsamples for our trend analysis. The data did not allow trend analysis of dependence or abuse.
Implications
Despite these limitations, our analysis offers several insights for research and policy. Our results, like those of others, underscore the low prevalence of substance-use disorders among welfare recipients. Abuse and dependence appear less common than other educational, physical, or mental health barriers to self-sufficiency.11
More surprising to us, low-income women who reported recent illicit drug use now report similar welfare receipt to that reported by other low-income mothers. Since the early 1990s, reported welfare receipt declined much more sharply among mothers who reported recent illicit drug use than among other mothers.
From one perspective, such findings provide reassurance regarding the composition of the TANF population after welfare reform. Although caseloads have declined so that they include a potentially more disadvantaged core of recipients, the prevalence of illicit drug use among welfare recipients in 2001 and 2002 remained lower than levels reported in 1990. A more worrisome possibility is that an increased proportion of low-income women who use illicit substances is becoming “disconnected” from welfare without achieving economic self-sufficiency.
We observed a slight increase in reported substance use among TANF recipients between 1996 and 2001, but these were similar to observed patterns among mothers who did not receive TANF aid. The observed trends suggest, though our analysis cannot prove, that changes in illicit substance use among welfare recipients reflect changing behavior throughout American society rather than specific developments within the welfare system itself.
We found more disturbing results when we broadened our conception of “problem” substance use. Although few respondents fully satisfied criteria for abuse or dependence, many reported economic, social, or medical concerns associated with substance use. We were surprised to find that 12.5% of TANF recipients—compared with 5.6% of mothers who did not receive TANF aid—experienced at least 1 identified symptom of illicit substance abuse or dependence. Once alcohol was included, one third of recipients reported some tangible difficulty that they attributed to drug or alcohol use.
The implications of these symptoms, which, though tangible, do not satisfy DSM-IV criteria for dependence or abuse, have received limited research, though suggestive findings have been reported regarding alcohol (e.g., Eng et al.48). Unpacking the meaning of these symptoms is especially difficult when the reported impact of substance use is influenced by context. For example, employed individuals may be more likely than others to report workplace consequences of alcohol use.
We believe our most striking finding was the large, albeit declining, proportion of welfare recipients among low-income mothers who use or abuse illicit drugs, and the large proportion of welfare recipients among clients of treatment interventions. The welfare system includes a smaller proportion of substance users than was found before the 1996 welfare reform act. However, the welfare system remains a central arena to identify, assess, and serve women with substance-use disorders.
Welfare recipients still account for a large proportion of low-income mothers who receive drug or alcohol treatment. Although only 30% of welfare recipients in need of treatment actually received such services in the past year, actual treatment participation appears almost 3 times higher than among other mothers in need of treatment who did not receive TANF aid.
We do not know why welfare recipients are such a large proportion of mothers receiving substance-abuse treatment. Medicaid secured through TANF may expand access to treatment. Among 2002 NSDUH respondents who did not receive TANF aid, 45% of low-income, substance-abusing mothers and 41% of low-income, substance-using mothers lacked health insurance coverage at the time of interview. Receipt of TANF may provide other pathways into treatment services, such as screening and assessment services that bring TANF recipients into contact with substance-abuse treatment.15,25,26,49 It is also possible that treatment facilities assist clients in claiming public entitlements.
Traditionally, AFDC was a gateway into substance-abuse treatment for many women. As welfare rolls decline, welfare recipients account for a decreasing proportion of treatment clients. As in the case of declining health insurance coverage of low-income mothers, an unintended consequence may be to alter the funding streams and entitlements available for key services.50,51 This trend equally challenges child protection and other systems of outreach and recruitment closely linked with public aid. As TANF caseloads decrease, finding new means to identify and to serve mothers with substance-use disorders becomes an important policy challenge of welfare reform.
Acknowledgments
This analysis received financial support from the Robert Wood Johnson Foundation’s Substance Abuse Policy Research program (grant 380971) and the Smith-Richardson Foundation (grant 9601-795).
Human Participant Protection This analysis of nonidentified secondary data is exempt from institutional review board approval.
Peer Reviewed
Contributors Both authors originated the analysis and wrote the initial draft. H. A. Pollack performed the statistical analysis. P. Reuter took overall responsibility for article revision.
References
- 1.National Center on Addiction and Substance Abuse at Columbia University, American Public Human Services Association. Building Bridges: States Respond to Substance Abuse and Welfare Reform. New York, NY: National Center on Addiction and Substance Abuse at Columbia University; 1999.
- 2.Califano J. It’s Drugs, Stupid. New York Times Sunday Magazine. January 29, 1995:40–41.
- 3.Weaver RK. Ending Welfare as We Know It: Policy Making for Low-Income Families in the United States. Washington, DC: Brookings Institution; 2000.
- 4.Schoeni RM, Blank RF. What Has Welfare Reform Accomplished? Impact on Welfare Participation, Employment, Income, Poverty, and Family Structure. Cambridge, Mass: National Bureau of Economic Research; 2000.
- 5.Danziger SH. Economic Conditions and Welfare Reform: What Are the Early Lessons? Kalamazoo, Mich: Upjohn Institute for Employment Research; 1999.
- 6.Danziger SH, Haveman RH. Understanding Poverty. Cambridge, Mass: Harvard University Press; 2001.
- 7.Metsch LR, Pollack HA. Welfare reform and substance abuse. Milbank Q. 2005;83:65–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Green Book Overview of Entitlement Programs. Washington, DC: United States House of Representatives, Committee on Ways and Means; 2000.
- 9.Lichter D, Jayakody R. Welfare reform: how do we measure success? Annu Rev Sociol. 2002;28: 117–141. [Google Scholar]
- 10.Kaufman L. New York says those on welfare are increasingly hard to employ. New York Times. November 29, 2002:A1.
- 11.Danziger SK, Corcoran M, Danziger S, et al. Barriers to the employment of welfare recipients. In: Cherry R, Rogers WM, eds. Prosperity for All? The Economic Boom and African-Americans. New York, NY: Russell Sage Foundation; 2000.
- 12.Loprest PJ. Families Who Left Welfare: Who Are They and How Are They Doing? Washington, DC: Urban Institute; 1999. Report No. 99–02.
- 13.Personal Responsibility and Work Opportunity Reconciliation Act, Pub L No. 104–193, 110 Stat 2105. (1996).
- 14.Morgenstern J, Riordan A, McCrady B, McVeigh K, Blanchard K, Irwin T. Outcomes of a public health model approach to assisting women on TANF with substance abuse problems. Paper presented at: 2001 Annual Meeting of the American Public Health Association.
- 15.Morgenstern J, Riordan A, Dephilippis D, et al. Specialized screening approaches can substantially increase the identification of substance abuse problems among welfare recipients. Available at: http://aspe.hhs.gov/hsp/njsard00/screening-rn.htm. Accessed September 13, 2006.
- 16.Delva J, Neumark YD, Furr CD, Anthony JC. Drug use among welfare recipients in the United States. Am J Drug Alcohol Abuse. 2000;26:335–342. [DOI] [PubMed] [Google Scholar]
- 17.Grant BF, Dawson DA. Alcohol and drug use, abuse, and dependence among welfare recipients. Am J Public Health. 1996;86:1450–1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jayakody R, Danziger S, Pollack H. Welfare reform, substance use, and mental health. J Health Polit Policy Law. 2000;25:623–651. [DOI] [PubMed] [Google Scholar]
- 19.Danziger S, Seefeldt K. Barriers to employment and the “hard to serve”: implications for services, sanctions, and timer limits. Focus. 2002;22:76–81. [Google Scholar]
- 20.Danziger S, Kalil A, Anderson N. Human capital, health and mental health of welfare recipients: co-occurrence and correlates. J Soc Issues. 2000;56:635. [Google Scholar]
- 21.Lown EA, Schmidt LA, Wiley J. Interpersonal violence among women seeking welfare: unraveling lives. Am J Public Health. 2006;96(8):1409–1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Montoya ID, Atkinson JS, Struse HM. A comparison of psychological barriers among welfare recipients: implications for drug treatment. Subst Use Misuse. 2001; 36:771–788. [DOI] [PubMed] [Google Scholar]
- 23.Montoya ID, Atkinson JS. A synthesis of welfare reform policy and its impact on substance users. Am J Drug Alcohol Abuse. 2002;28:133–146. [DOI] [PubMed] [Google Scholar]
- 24.Morgenstern J. Why are screening and treatment referral rates lower than expected in the New Jersey substance abuse initiative? Paper presented at: Improving the Identification and Referral Processes between the Welfare and Substance Abuse Systems; Washington, DC: December 30, 1999.
- 25.Morgenstern J, McCrady BS, Blanchard KA, McVeigh KH, Riordan A, Irwin TW. Barriers to employability among substance dependent and nonsubstance-affected women on federal welfare: implications for program design. J Stud Alcohol. 2003;64:239–246. [DOI] [PubMed] [Google Scholar]
- 26.Morgenstern J, Nakashian M, Woolis DD, Gibson FM, Bloom NL, Kaulback BG. CASAWORKS for families: a new treatment model for substance-abusing parenting women on welfare. Eval Rev. 2003;27:583–596. [DOI] [PubMed] [Google Scholar]
- 27.Schmidt L, Dohan D, Wiley J, Zabkiewicz D. Addiction and welfare dependency: interpreting the connection. Soc Problems. 2002;49:221–241. [Google Scholar]
- 28.Schmidt L, Weisner C, Wiley J. Substance abuse and the course of welfare dependency. Am J Public Health. 1998;88:1616–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morgenstern J, Riordan A, Dephilippis D, et al. Research Notes. Specialized Screening Approaches Can Substantially Increase the Identification of Substance Abuse Problems Among Welfare Recipients. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services; 2001.
- 30.Pollack H, Danziger S, Jayakody R, Seefeldt K. Substance use among welfare recipients: trends and policy responses. Soc Serv Rev. 2002;76:256–274. [Google Scholar]
- 31.Kaestner R. Drug use and AFDC participation: is there a connection? J Policy Analysis Manage. 1998;17: 493–520. [Google Scholar]
- 32.Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition. Washington, DC: American Psychiatric Association; 1987.
- 33.Pollack HA, Danziger S, Jayakody R, Seefeldt KS. Drug testing welfare recipients—false positives, false negatives, unanticipated opportunities. Womens Health Issues. 2002;12:23–31. [DOI] [PubMed] [Google Scholar]
- 34.Schmidt LA, McCarty D. Welfare reform and the changing landscape of substance abuse services for low-income women. Alcohol Clin Exp Res. 2000;24: 1298–1311. [PubMed] [Google Scholar]
- 35.Duncan G. Trends in the Well-Being of America’s Children and Youth. Washington, DC: Department of Health and Human Services; 1997.
- 36.Substance Abuse and Mental Health Services Administration. Results From the 2002 National Survey on Drug Use and Health: National Findings. Rockville, Md: Department of Health and Human Services; 2003.
- 37.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994.
- 38.Warner LA, Kessler RC, Hughes M, Anthony JC, Nelson CB. Prevalence and correlates of drug use and dependence in the United States: Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:219–229. [DOI] [PubMed] [Google Scholar]
- 39.Pollack H, Danziger S, Seefeldt K, Jayakody R. Substance abuse among welfare recipients: trends and policy responses. Soc Serv Rev. 2002;76:256–274. [Google Scholar]
- 40.Pull CB, Saunders JB, Mavreas V, et al. Concordance between ICD-10 alcohol and drug use disorder criteria and diagnoses as measured by the AUDADIS-ADR, CIDI and SCAN: results of a cross-national study. Drug Alcohol Depend. 1997;47:207–216. [DOI] [PubMed] [Google Scholar]
- 41.Edin K, Lein L. Making Ends Meet: How Single Mothers Survive Welfare and Low-Wage Work. New York, NY: Russell Sage Foundation; 1997.
- 42.Magura S, Kang SY. Validity of self-reported drug use in high risk populations: a meta-analytical review. Subst Use Misuse. 1996;31:1131–1153. [DOI] [PubMed] [Google Scholar]
- 43.The Validity of Self-Reported Drug Use: Improving the Accuracy of Survey Estimates. Washington, DC: National Institute on Drug Abuse; 1997.
- 44.Midanik LT, Greenfield TK. Telephone versus in-person interviews for alcohol use: results of the 2000 National Alcohol Survey. Drug Alcohol Depend 2003; 72:209–214. [DOI] [PubMed] [Google Scholar]
- 45.What America’s Users Spend on Illicit Drugs, 1988–2000. Washington, DC: The White House Office of National Drug Control Policy; 2001.
- 46.Fendrich M, Johnson TP, Wislar JS, Hubbell A, Spiehlter V. The utility of drug testing in epidemiological research: results from a general population survey. Addiction. 2004;99:197–208. [DOI] [PubMed] [Google Scholar]
- 47.Pavetti L, Bloom D. State sanctions and time limits. In: Blank RM, Haskins R, eds. The New World of Welfare. Washington, DC: Brookings Institution; 2001.
- 48.Eng MY, Schuckit MA, Smith TL. A five-year prospective study of diagnostic orphans for alcohol use disorders. J Stud Alcohol. 2003;64:227–234. [DOI] [PubMed] [Google Scholar]
- 49.Morgenstern J, Riordan A, McCrady B, McVeigh K, Blanchard K, Irwin T. Intensive Case Management Improves Welfare Clients’ Rates of Entry and Retention in Substance Abuse Treatment. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services; 2001.
- 50.Kronebusch K. Medicaid for children: federal mandates, welfare reform, and policy backsliding. Health Aff (Millwood). 2001;20:97–111. [DOI] [PubMed] [Google Scholar]
- 51.Kronebusch K. Children’s Medicaid enrollment: the impacts of mandates, welfare reform, and policy delinking. J Health Polit Policy Law. 2001;26: 1223–1260. [DOI] [PubMed] [Google Scholar]


