Abstract
OBJECTIVE
Autonomic nervous system dysfunction, a correlate of obesity and poor cardiorespiratory fitness, is associated with the development of diabetes. We tested whether estimates of autonomic nervous system function improved in the intensive lifestyle versus metformin or placebo arms of the Diabetes Prevention Program (DPP) and whether baseline or a change in autonomic nervous system function was associated with the development of diabetes over 3.2 years.
RESEARCH DESIGN AND METHODS
In 2,980 DPP participants, 12-lead electrocardiograms were measured at baseline and annually. Heart rate, heart rate variability (HRV), and QT duration were used to estimate fitness and autonomic nervous system function.
RESULTS
In the lifestyle arm, heart rate and QT indexes decreased, and HRV increased over time. The magnitude of decline in heart rate and QT duration was substantially smaller in the other arms, whereas HRV did not increase. Baseline heart rate was the only index significantly (P < 0.05) associated with incident diabetes after adjustment for demographics and weight change (hazard ratio for lifestyle and metformin arms = 1.19 and 1.17 per 10.6 beats/min, respectively). Decreases in heart rate and QT indexes and increases in HRV over time were associated with a lower risk of developing diabetes. The protective association between decreased heart rate and incident diabetes in the lifestyle arm remained significant after accounting for change in weight and physical activity.
CONCLUSIONS
Indexes that reflect autonomic function and fitness improved (i.e., heart rate decreased and HRV increased) in the lifestyle modification arm of the DPP. Improvements in these indexes are inversely associated with the development of diabetes independent of weight change.
Abbreviations: DPP, Diabetes Prevention Program; ECG, electrocardiogram; HRV, heart rate variability; QTc, Bazett’s correction; QTI, QT index; rMSSD, root mean square of successive differences between all normal-to-normal R-R intervals; SDNN, standard deviation of all normal-to-normal R-R intervals
Autonomic impairment has been identified at the time of diabetes diagnosis, which suggests that impairment may be present after a relatively brief exposure to hyperglycemia or develop in conjunction with obesity or insulin resistance (1,2). Cross-sectional studies in adults without diabetes provide evidence that markers of autonomic functioning are inversely associated with obesity, insulin resistance, and fasting glucose (3–6). Recent research suggesting that autonomic dysfunction predicts the development of diabetes (7,8) supports the long-held clinical suspicion that autonomic dysfunction is associated with the development of diabetes in healthy adults (9).
Adults were identified as eligible to participate in the Diabetes Prevention Program (DPP) because they were at risk for developing diabetes, most commonly because of existing hyperglycemia and obesity. Thus, it is plausible that many had existing autonomic impairment at baseline in the study. At the conclusion of the trial, there was a significantly lower incidence of diabetes in the intensive lifestyle modification arm compared with that in the metformin or placebo arms (10). Lifestyle modification involved increasing physical activity and lowering dietary fat intake with a goal of lowering weight. It is not known whether, secondary to weight loss, mechanisms such as improved autonomic function or fitness, which are both inversely associated with diabetes incidence in healthy adults (5,7,11,12), account for the lower incidence of diabetes in the lifestyle arm of the DPP trial.
Thus, the objectives of our post hoc analysis of the DPP trial were to 1) test whether measures of autonomic function at baseline were related to the development of diabetes in each arm over the course of the study, 2) investigate whether changes in measures of autonomic function over the course of the trial differed by treatment arm, and 3) test whether changes in autonomic function over time were related to the development of diabetes. We hypothesized that changes in autonomic function measures would be most favorable in the lifestyle modification arm of the trial and that those participants with the least favorable autonomic function at baseline and over time were more likely to develop diabetes.
RESEARCH DESIGN AND METHODS
Details of the DPP study design, participants, and primary outcomes have been published previously (13–16). In brief, adults aged ≥25 years who were at high risk for developing diabetes (i.e., BMI ≥24 kg/m2, fasting glucose 5.3–6.9 mmol/l, and 2-h glucose 7.8–11.0 mmol/l) were recruited from 27 U.S. clinical centers. The institutional review board at each center approved the protocol, and all participants gave written informed consent.
This analysis includes participants randomly assigned to one of three groups (15): 1) standard lifestyle recommendations plus placebo twice daily; 2) standard lifestyle recommendations plus 850 mg of metformin twice daily; and 3) an intensive program of lifestyle modification. The goal for lifestyle intervention participants was to achieve and maintain a weight reduction of at least 7% of initial body weight through a healthy, low-fat diet and by engaging in moderate-intensity physical activity such as brisk walking for at least 150 min/week. A detailed description of intervention arms have been published (13). Study design and analysis were conducted according to the intention-to-treat principle.
Randomly assigned participants were excluded from this analysis for the following reasons: prior history of myocardial infarction (n = 32) or stroke (n = 8) at baseline, inability to calculate heart rate variability (HRV) (n = 180), and use of drugs known to cause heart rhythm disturbances (e.g., specific antidepressants and antihypertensive medications) (n = 45). No participants had a history of atrial fibrillation. There were no differences in exclusions across treatment arms. Remaining participants (n = 2,980) were followed for an average of 3.2 years (maximum 5 years) from June 1996 through 31 July 2001.
Measurements
Electrocardiograms (ECGs) were recorded at baseline and annually throughout the study using MAC PC-DT electrocardiographs (Marquette Electronics, Milwaukee, WI). A 10-s segment of simultaneous ECG leads was sampled at a rate of 250 samples/s. ECGs were transmitted daily to the Epidemiological Cardiology Research Center (Winston-Salem, NC) for analysis and classification using the Minnesota code derived from the NOVACODE ECG program (17,18). Multiple editing removed poor quality tracings. Participants whose records indicated frequent premature beats, second-or third-degree atrioventricular block, Wolff-Parkinson-White syndrome, an artificial pacemaker, or <5 acceptable R-R intervals were excluded from analysis.
Maximum QT duration was measured from simultaneously recorded leads from the earliest onset of QRS to the latest offset of the T-wave in the 12-lead ECG using Marquette GE program version 12SL. Interactive technician/ computer overreading was conducted on 10% of records that were selected because of extreme values. QT duration represents time between the onset of ventricular activation and the end of repolarization, a process thought to be controlled in part by sympathetic input. Longer QT intervals represent greater sympathetic tone. QT intervals were corrected for heart rate using the QT index (QTI) [(measured QT/ predicted QT) ×100, where the predicted QT = 656/(1 + 0.01 * heart rate) (18)] and Bazett’s correction (QTc = QT/ RR1/2) (19).
The following HRV measures were generated based on the 10-s digital rhythm strip: mean heart rate across all 12 leads (beats/min), the standard deviation of all normal-to-normal R-R intervals (SDNN) (milliseconds), and the root mean square of successive differences between all normal-to-normal R-R intervals (rMSSD) (milliseconds). Heart rate represents both overall autonomic function and cardiorespiratory fitness (20). SDNN represents joint sympathetic and parasympathetic modulation of heart rate, whereas rMSSD is thought to represent parasympathetic modulation of heart rate. Higher heart rate indicates poor autonomic function and low fitness, whereas lower SDNN and rMSSD represent poor function (21).
Diabetes was defined according to 1997 American Diabetes Association guidelines (22,23). Sociodemographic, anthropometric, and clinical measurements and health behaviors were collected according to standard procedures across study sites (23).
Statistical analysis
Means and proportions of baseline characteristics were computed for the total population and for the treatment arms. Fixed-effects models with the assumption of normally distributed errors (24) were used to assess differences in ECG indexes over time among the treatment groups. P values for the comparisons between any two-treatment arms were adjusted for multiple comparisons using the Holm procedure (25), and statistical significance was set at P < 0.05. Proportional hazards regression was used to assess the effect of baseline and time-dependent ECG indexes on the development of diabetes adjusted for baseline demographics (age, race/ethnicity, and sex) and known risk factors (physical activity and weight). We knowingly adjusted for factors along the causal pathway (i.e., physical activity and weight) because our objective was to determine whether another factor, autonomic function, exerted any independent effects on the development of diabetes. This type of etiologic modeling is cited as a special circumstance in which adjustment for factors along the causal pathway can be appropriate (26). The time-dependent changes in heart rate, HRV index, QT indexes, and weight were entered into the proportional hazards model as the average change experienced, updated for every visit assessment. Hazard ratios (HRs) and 95% CIs for the ECG indexes are presented in terms of a difference in SD at baseline and the SD change during follow-up (i.e., decreases in heart rate, QTI, and QTc and increases in SDNN and rMSSD). All analyses were conducted using SAS version 8.2 (SAS Institute, Cary, NC).
RESULTS
Demographic and clinical characteristics in this sample are similar to previously reported distributions in the DPP population (15). The average ± SD age of participants was 50.4 ± 10.6 years, 68% were female, and nearly half of the cohort were race/ethnic minorities (African American 20%, Hispanic 16%, American Indian 5.3%, and Asian American 4.2%). Participants’ average BMI was 34 ± 7 kg/m2, and waist circumference was 104.9 ± 14.5 cm. On average, fasting glucose was 5.9 ± 0.5 mmol/l, HbA1c was 5.9 ± 0.5%, and systolic and diastolic blood pressures were 124 ± 15 and 78 ± 9 mmHg, respectively.
Over an average of 3.2 years, crude rates of diabetes were 10.6, 7.7, and 5.1 per 100 person-years in the placebo, metformin, and lifestyle arms, respectively, which is consistent with previous reports (10). There was no association between any of the HRV or QT indexes measured at baseline and incident diabetes. Higher baseline heart rate was modestly, but significantly, related to the development of diabetes in all treatment arms (Table 1). In the placebo, metformin, and lifestyle arms, each 4.5-kg weight gain over time was associated with a 1.4, 1.5, and 2.4-fold increase in the risk of developing diabetes, respectively. Heart rate remained significantly associated with diabetes development in the metformin and lifestyle arms even after adjustment for weight change and physical activity over time. Additional adjustment for hypertension status did not change the results.
Table 1.
Adjusted HRs (95% CI) of developing diabetes by baseline ECG indices and treatment arm
| Placebo | Metformin | Lifestyle | |
|---|---|---|---|
| Heart rate (per 11 bpm) | |||
| Model 1 | 1.13 (1.01–1.27) | 1.17 (1.03–1.34) | 1.27 (1.08–1.49) |
| Model 2 | 1.09 (0.97–1.22) | 1.17 (1.03–1.35) | 1.19 (1.02–1.40) |
| SDNN (per 19 ms) | |||
| Model 1 | 1.01 (0.90–1.14) | 0.88 (0.74–1.05) | 0.94 (0.79–1.14) |
| Model 2 | 1.04 (0.91–1.18) | 0.90 (0.76–1.06) | 0.99 (0.82–1.18) |
| rMSSD (per 24 ms) | |||
| Model 1 | 0.99 (0.87–1.11) | 0.87 (0.72–1.04) | 0.87 (0.71–1.08) |
| Model 2 | 1.01 (0.88–1.18) | 0.90 (0.76–1.06) | 0.89 (0.73–1.08) |
| QTc (per 18 ms) | |||
| Model 1 | 1.06 (0.94–1.20) | 1.09 (0.95–1.25) | 1.08 (0.93–1.26) |
| Model 2 | 0.98 (0.86–1.11) | 1.10 (0.96–1.27) | 0.96 (0.81–1.14) |
| QTI (per 4%) | |||
| Model 1 | 1.02 (0.90–1.15) | 1.02 (0.88–1.17) | 1.02 (0.87–1.20) |
| Model 2 | 0.95 (0.84–1.08) | 1.03 (0.89–1.19) | 0.91 (0.76–1.09) |
Model 1 adjusted for age, race, and sex. Model 2 adjusted for model 1 + baseline weight and weight change (per 4.5 kg) over follow-up.
Although ECG indexes were similar across treatment arms at baseline, the magnitude of the average change from baseline was greatest in the lifestyle arm for each of the ECG indexes except QTI (Table 2). Figure 1 is a graphic representation of the mean values in ECG indexes (A–F) at each time point over the study period. The lifestyle group experienced lower heart rate and QTc duration, accompanied by higher HRV (i.e., SDNN and rMSSD) compared with metformin and placebo arms.
Table 2.
Baseline ECG indices* and average changes over 3.2 years by treatment arm
| Placebo | Metformin | Lifestyle | |
|---|---|---|---|
| Heart rate (bpm) | |||
| Baseline | 68.8 (68.2–69.4) | 68.1 (67.4–68.8) | 68.3 (67.7–69.0) |
| Average change | −2.12 (−2.57 to −1.67) | −1.88 (−2.39 to −1.37) | −4.74 (−5.21 to −4.27) |
| SDNN (ms) | |||
| Baseline | 24.9 (23.6–26.1) | 24.7 (23.6–25.8) | 25.6 (24.4–26.8) |
| Average change | −1.21 (−2.03 to −0.39) | −0.58 (−1.54 to 0.38) | 1.32 (0.30–2.34) |
| rMSSD (ms) | |||
| Baseline | 27.5 (25.8–29.2) | 27.0 (25.5–28.4) | 27.8 (26.3–29.3) |
| Average change | −0.88 (−1.96 to 0.20) | −0.25 (−1.58 to 1.08) | 2.98 (1.71–4.25) |
| QTc (ms) | |||
| Baseline | 416 (414.9–417.0) | 415.3 (414.2–416.4) | 416 (414.8–417.1) |
| Average change | −1.68 (−2.66 to −0.70) | −3.41 (−4.37 to −2.45) | −4.78 (−5.82 to −3.74) |
| QTI (%) | |||
| Baseline | 100.1 (99.9–100.2) | 100 (99.8–100.3) | 100.1 (99.9–100.4) |
| Average change | −0.20 (−0.42 to 0.02) | −0.62 (−0.84 to −0.40) | −0.43 (−0.67 to −0.19) |
Data are means (95% CI).
There were no significant differences between baseline ECG indices across treatment arms.
Figure 1.
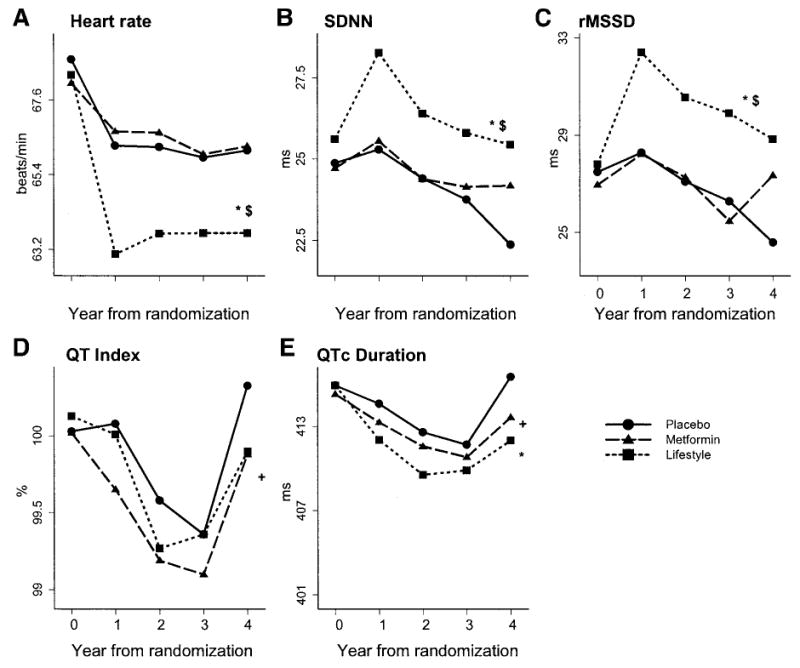
Changes in heart rate, HRV indexes, and QT duration over time by treatment arm. *P < 0.05, placebo vs. lifestyle; +P < 0.05, placebo vs. metformin; and $P < 0.05, metformin vs. lifestyle.
Next, we calculated HRs for developing incident diabetes in each treatment arm if ECG indexes demonstrated the hypothesized increases in SDNN and rMSSD and decreases in heart rate, QTI, and QTc over follow-up, adjusting for the baseline value (Table 3). After adjustment for demographic characteristics and the baseline ECG index, decreasing heart rate, QTI, and QTc and increasing SDNN and rMSSD were associated with lower diabetes risk in the lifestyle arm. SDNN in the lifestyle arm continued to be associated with a lower risk of incident diabetes when we further adjusted for changes in weight and physical activity over time, whereas a significant effect of heart rate remained in both the lifestyle and placebo arms.
Table 3.
Adjusted HRs (95% CI) of developing diabetes by changes in ECG indices across treatment arm
| Placebo | Metformin | Lifestyle | |
|---|---|---|---|
| Heart rate (per 8 bpm decrease) | |||
| Model 1 | 0.80 (0.70–0.92) | 0.88 (0.75–1.03) | 0.60 (0.49–0.72) |
| Model 2 | 0.85 (0.74–0.98) | 0.91 (0.77–1.06) | 0.72 (0.58–0.90) |
| SDNN (per 17 ms increase) | |||
| Model 1 | 0.93 (0.79–1.09) | 0.97 (0.82–1.14) | 0.66 (0.51–0.86) |
| Model 2 | 0.96 (0.83–1.12) | 0.98 (0.83–1.15) | 0.75 (0.58–0.97) |
| rMSSD (per 22 ms increase) | |||
| Model 1 | 0.89 (0.75–1.06) | 0.90 (0.75–1.08) | 0.67 (0.51–0.88) |
| Model 2 | 0.91 (0.77–1.08) | 0.92 (0.77–1.09) | 0.78 (0.61–1.01) |
| QTc (per 15 ms Decrease) | |||
| Model 1 | 0.89 (0.79–1.00) | 0.84 (0.71–0.98) | 0.73 (0.61–0.86) |
| Model 2 | 0.91 (0.80–1.02) | 0.88 (0.75–1.03) | 0.86 (0.71–1.04) |
| QTI (per 3% decrease) | |||
| Model 1 | 0.93 (0.83–1.06) | 0.90 (0.77–1.05) | 0.83 (0.69–0.99) |
| Model 2 | 0.93 (0.83–1.05) | 0.93 (0.80–1.10) | 0.89 (0.74–1.08) |
Model 1 adjusted for baseline age, race, sex, and baseline ECG index. Model 2 adjusted for model 1 + weight change and change in physical activity.
CONCLUSIONS
Over the course of the DPP trial, estimates of autonomic function derived from the 12-lead ECG improved in the lifestyle arm compared with the metformin or placebo arm. Higher heart rate at baseline, representing both poor fitness and impaired autonomic function, was associated with a modestly increased incidence of diabetes. Further, we found that increasing fitness or autonomic function over time, as indicated by lowered heart rate and increased SDNN, was associated with a reduced risk of development of diabetes even after adjustment for changes in weight and physical activity. Although these factors are in the causal pathway between lifestyle modification and incident diabetes, they did not account for all of the observed effects of autonomic function.
Modifying autonomic function
The improvements in estimates of autonomic functioning that we report in the lifestyle arm are plausible given reported associations in clinical and population-based studies among fitness, physical activity, and autonomic functioning (27–30). Nearly three-quarters (74%) of participants in the lifestyle arm of the DPP met their goal of at least 150 min of physical activity per week at 24 weeks after randomization (10). In a previously sedentary and overweight population, this amount of activity probably improved fitness in addition to inducing weight loss. Unfortunately, we did not have measurements of fitness, such as VO2max determined by graded exercise treadmill testing, available in the DPP study.
Primary results from the DPP trial indicated a significant reduction in incident diabetes in both the lifestyle and metformin arms, with the greater reduced risk in the lifestyle arm (10). In this post hoc analysis, we report little difference in ECG estimates of autonomic function between the metformin and placebo arms. Participants in the metformin arm experienced changes in autonomic functioning that were midway between those in the lifestyle and placebo groups (i.e., QT indexes, SDNN, and rMSSD). The modest protection conferred by metformin may be attributable to its ability to lower blood glucose, which at higher levels contributes to the degradation of autonomic fibers. Findings in the metformin arm suggest that lowering glucose boosts autonomic function. However, additional benefits may be conferred by increasing physical activity and potentially improving fitness as demonstrated by the superior results in the lifestyle modification arm.
Incident diabetes
The hypothesis that autonomic nervous system function precedes the onset of diabetes is biologically plausible because the pancreas is heavily innervated with parasympathetic fibers. Whereas parasympathetic fibers stimulate the β-cells to release insulin in response to circulating glucose, sympathetic activation inhibits insulin secretion from the β-cells. Persistently elevated glucose levels in the non-diabetic range may damage peripheral nerve fibers, thus stimulating sympathetic activity and decreasing parasympathetic control (31–33). Thus, conditions of autonomic imbalance may result in impaired transport of blood glucose to the muscle cells, a negative feedback cycle that may continue as circulating glucose levels gradually increase. Additionally, sympathetically mediated catecholamine release increases circulating free fatty acids, which further contribute to the development of insulin resistance and diabetes (34,35).
With the exception of the association between higher heart rate at baseline and incident diabetes, the associations between ECG indexes at baseline and incident diabetes were largely null. Our results with baseline measures were consistent with the modest (20%) statistically significant increase in the risk of developing diabetes with higher heart rate over ~8 years in the Atherosclerosis Risk in Communities (ARIC) study (7). Participants in the Coronary Artery Development in Young Adults (CARDIA) study with joint poor cardiorespiratory fitness and slower heart rate recovery after a graded exercise treadmill test were at a threefold increased risk for developing diabetes compared with those with faster heart rate recovery (8). Given the independent association between poor fitness and diabetes development (11,12), it is not surprising that the strongest and most consistent finding to date is the importance of fitness and an estimate of fitness such as heart rate in the development of diabetes.
Limitations of ECG measurements
The absence of an association between baseline HRV and incident diabetes in this study does not negate the possibility of an association but may be attributable to measurement error. HRV is a reliable estimate of autonomic function for use in population studies (21). However, in a recent study of the repeatability of HRV measurements, Schroeder et al. (36) reported that the repeatability of a single measure of HRV from the 10-s ECG is low (SDNN r = 0.41; rMSSD r = 0.47). The authors recommended the use of the mean of several available recordings, which were not available in the present study. Heart rate–corrected QT duration is controlled in part by sympathetic nerve activity (37). Longer QT intervals, representing higher sympathetic activity, have been related to glucose and insulin in cross-sectional studies (38). Because other factors contribute to QT length, including heart rate, additional research using other methods to ascertain the sympathetic component of autonomic function is warranted.
In summary, we conclude that improved fitness and autonomic function may have contributed to the lower risk of development of diabetes in the lifestyle arm of the DPP compared with the metformin and placebo arms. Although we were unable to quantify the contribution or separate the effects of fitness versus autonomic function, this report provides further evidence that lifestyle changes that include increased physical activity improve physiologic parameters related to diabetes development.
Acknowledgments
Funding was provided by the National Institutes of Health through the National Institute of Diabetes and Digestive and Kidney Diseases, the Office of Research on Minority Health, the National Institute of Child Health and Human Development, the Office of Women’s Health, and the National Institute on Aging. In addition, the Indian Health Service, the Centers for Disease Control and Prevention, the American Diabetes Association, and two pharmaceutical companies, Bristol-Myers Squibb and Parke-Davis, contributed support. The General Clinical Research Center Program, National Center for Research Resources, supported many of the clinical centers. Support to the clinical centers and the Coordinating Center was provided by the National Institute of Diabetes and Digestive and Kidney Diseases through a Cooperative Agreement, except for the Southwestern American Indian Centers, which were supported directly by the National Institute of Diabetes and Digestive and Kidney Diseases and the Indian Health Service. M.R.C. was supported in part by career development award 1 K01 HL073249-02 from the National Heart, Lung, and Blood Institute, National Institutes of Health.
Footnotes
A table elsewhere in this issue shows conventional and Système International (SI) units and conversion factors for many substances.
References
- 1.Lehtinen JM, Uusitupa M, Siitonen O, Pyorala K. Prevalence of neuropathy in newly diagnosed NIDDM and nondia-betic control subjects. Diabetes. 1989;38:1307–1313. doi: 10.2337/diab.38.10.1307. [DOI] [PubMed] [Google Scholar]
- 2.Pfeifer MA, Weinberg CR, Cook DL, Ree-nan A, Halter JB, Ensinck JW, Porte D., Jr Autonomic neural dysfunction in recently diagnosed diabetic subjects. Diabetes Care. 1984;7:447–453. doi: 10.2337/diacare.7.5.447. [DOI] [PubMed] [Google Scholar]
- 3.Liao D, Cai J, Brancati FL, Folsom A, Barnes RW, Tyroler HA, Heiss G. Association of vagal tone with serum insulin, glucose, and diabetes mellitus—the ARIC Study. Diabetes Res Clin Pract. 1995;30:211–221. doi: 10.1016/0168-8227(95)01190-0. [DOI] [PubMed] [Google Scholar]
- 4.Singh JP, Larson MG, O’Donnell CJ, Wilson PF, Tsuji H, Lloyd-Jones DM, Levy D. Association of hyperglycemia with reduced heart rate variability (the Framingham Heart Study) Am J Cardiol. 2000;86:309–312. doi: 10.1016/s0002-9149(00)00920-6. [DOI] [PubMed] [Google Scholar]
- 5.Panzer C, Lauer MS, Brieke A, Blackstone E, Hoogwerf B. Association of fasting plasma glucose with heart rate recovery in healthy adults: a population-based study. Diabetes. 2002;51:803–807. doi: 10.2337/diabetes.51.3.803. [DOI] [PubMed] [Google Scholar]
- 6.Festa A, D’Agostino R, Jr, Hales CN, Mykkanen L, Haffner SM. Heart rate in relation to insulin sensitivity and insulin secretion in nondiabetic subjects. Diabetes Care. 2000;23:624–628. doi: 10.2337/diacare.23.5.624. [DOI] [PubMed] [Google Scholar]
- 7.Carnethon MR, Golden SH, Folsom AR, Haskell W, Liao D. Prospective investigation of autonomic nervous system function and the development of type 2 diabetes: the Atherosclerosis Risk in Communities Study, 1987–1998. Circulation. 2003;107:2190–2195. doi: 10.1161/01.CIR.0000066324.74807.95. [DOI] [PubMed] [Google Scholar]
- 8.Carnethon MR, Jacobs DR, Jr, Sidney S, Liu K. Influence of autonomic nervous system dysfunction on the development of type 2 diabetes: the CARDIA study. Diabetes Care. 2003;26:3035–3041. doi: 10.2337/diacare.26.11.3035. [DOI] [PubMed] [Google Scholar]
- 9.Landsberg L, Young JB. Insulin-mediated glucose metabolism in the relationship between dietary intake and sympathetic nervous system activity. Int J Obes. 1985;9:63–68. [PubMed] [Google Scholar]
- 10.Diaetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr, Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. JAMA. 2003;290:3092–3100. doi: 10.1001/jama.290.23.3092. [DOI] [PubMed] [Google Scholar]
- 12.Wei M, Gibbons LW, Mitchell TL, Kampert JB, Lee CD, Blair SN. The association between cardiorespiratory fitness and impaired fasting glucose and type 2 diabetes mellitus in men. Ann Intern Med. 1999;130:89–96. doi: 10.7326/0003-4819-130-2-199901190-00002. [DOI] [PubMed] [Google Scholar]
- 13.The Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25:2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Diabetes Prevention Program. design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999;22:623–634. doi: 10.2337/diacare.22.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The Diabetes Prevention Program. baseline characteristics of the randomized cohort: the Diabetes Prevention Program Research Group. Diabetes Care. 2000;23:1619–1629. doi: 10.2337/diacare.23.11.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rubin RR, Fujimoto WY, Marrero DG, Brenneman T, Charleston JB, Edelstein SL, Fisher EB, Jordan R, Knowler WC, Lichterman LC, Prince M, Rowe PM. The Diabetes Prevention Program: recruitment methods and results. Control Clin Trials. 2002;23:157–171. doi: 10.1016/s0197-2456(01)00184-2. [DOI] [PubMed] [Google Scholar]
- 17.Rautaharju PM, MacInnis PJ, Warren JW, Wolf HK, Rykers PM, Calhoun HP. Methodology of ECG interpretation in the Dalhousie program; NOVACODE ECG classification procedures for clinical trials and population health surveys. Methods Inf Med. 1990;29:362–374. [PubMed] [Google Scholar]
- 18.Rautaharju PM, Calhoun HP, Chaitman BR. NOVACODE serial ECG classification system for clinical trials and epidemiologic studies. J Electrocardiol. 1992;24:179–187. doi: 10.1016/s0022-0736(10)80041-x. [DOI] [PubMed] [Google Scholar]
- 19.Bazett HC. An analysis of the time-relations of electrocardiograms. Heart. 1920;7:353–370. [Google Scholar]
- 20.Blomqvist CG, Saltin B. Cardiovascular adaptations to physical training. Annu Rev Physiol. 1983;45:169–189. doi: 10.1146/annurev.ph.45.030183.001125. [DOI] [PubMed] [Google Scholar]
- 21.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation. 1996;93:1043–1065. [PubMed] [Google Scholar]
- 22.Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20:1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 23.Diabetes Prevention Program Coordinating Center. Manual of Operation. Rockville, MD: The George Washington University Biostatistics Center; [Google Scholar]
- 24.Diggle P, Liang K-Y, Zeger S. Analysis of Longitudinal Data. New York: Oxford University Press; 1994. [Google Scholar]
- 25.Holm S. A simple sequentially rejective Bonferroni test procedure. Scand J Stat. 1979;6:5–70. [Google Scholar]
- 26.Szklo M, Nieto FJ. Epidemiology: Beyond the Basics. Gaithersburg, MD: Aspen Publishers; 2000. [Google Scholar]
- 27.Cole CR, Blackstone EH, Pashkow FJ, Snader CE, Lauer MS. Heart-rate recovery immediately after exercise as a predictor of mortality. N Engl J Med. 1999;341:1351–1357. doi: 10.1056/NEJM199910283411804. [DOI] [PubMed] [Google Scholar]
- 28.Rennie KL, Hemingway H, Kumari M, Brunner E, Malik M, Marmot M. Effects of moderate and vigorous physical activity on heart rate variability in a British study of civil servants. Am J Epidemiol. 2003;158:135–143. doi: 10.1093/aje/kwg120. [DOI] [PubMed] [Google Scholar]
- 29.Carnethon MR, Jacobs DR, Jr, Sidney S, Sternfeld B, Gidding SS, Shoushtari C, Liu K. A longitudinal study of physical activity and heart rate recovery: CARDIA, 1987–1993. Med Sci Sports Exerc. 2005;37:606–612. doi: 10.1249/01.mss.0000158190.56061.32. [DOI] [PubMed] [Google Scholar]
- 30.Gregoire J, Tuck S, Yamamoto Y, Hughson RL. Heart rate variability at rest and exercise: influence of age, gender, and physical training. Can J Appl Physiol. 1996;21:455–470. doi: 10.1139/h96-040. [DOI] [PubMed] [Google Scholar]
- 31.Van De Borne P, Hausberg M, Hoffman RP, Mark AL, Anderson EA. Hyperinsulinemia produces cardiac vagal withdrawal and nonuniform sympathetic activation in normal subjects. Am J Physiol. 1999;276:R178–R183. doi: 10.1152/ajpregu.1999.276.1.R178. [DOI] [PubMed] [Google Scholar]
- 32.Vanninen E, Uusitupa M, Lansimies E, Siitonen O, Laitinen J. Effect of metabolic control on autonomic function in obese patients with newly diagnosed type 2 diabetes. Diabet Med. 1993;10:66–73. doi: 10.1111/j.1464-5491.1993.tb01999.x. [DOI] [PubMed] [Google Scholar]
- 33.Emdin M, Gastaldelli A, Muscelli E, Macerata A, Natali A, Camastra S, Ferrannini E. Hyperinsulinemia and autonomic nervous system dysfunction in obesity: effects of weight loss. Circulation. 2001;103:513–519. doi: 10.1161/01.cir.103.4.513. [DOI] [PubMed] [Google Scholar]
- 34.Benthem L, Keizer K, Wiegman CH, de Boer SF, Strubbe JH, Steffens AB, Kuipers F, Scheurink AJ. Excess portal venous long-chain fatty acids induce syndrome X via HPA axis and sympathetic activation. Am J Physiol. 2000;279:E1286–E1293. doi: 10.1152/ajpendo.2000.279.6.E1286. [DOI] [PubMed] [Google Scholar]
- 35.Pankow JS, Duncan BB, Schmidt MI, Ballantyne CM, Couper DJ, Hoogeveen RC, Golden SH. Fasting plasma free fatty acids and risk of type 2 diabetes: the Atherosclerosis Risk in Communities Study. Diabetes Care. 2004;27:77–82. doi: 10.2337/diacare.27.1.77. [DOI] [PubMed] [Google Scholar]
- 36.Schroeder EB, Whitsel EA, Evans GW, Prineas RJ, Chambless LE, Heiss G. Repeatability of heart rate variability measures. J Electrocardiol. 2004;37:163–172. doi: 10.1016/j.jelectrocard.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 37.Bednar MM, Harrigan EP, Anziano RJ, Camm AJ, Ruskin JN. The QT interval. Progr Cardiovasc Dis. 2001;43:1–45. doi: 10.1053/pcad.2001.21469. [DOI] [PubMed] [Google Scholar]
- 38.Dekker JM, Feskens EJ, Schouten EG, Klootwijk P, Pool J, Kromhout D. QTc duration is associated with levels of insulin and glucose intolerance: the Zutphen Elderly Study. Diabetes. 1996;45:376–380. doi: 10.2337/diab.45.3.376. [DOI] [PubMed] [Google Scholar]


