Abstract
Background. Cognitive therapy reduces depressive symptoms of major depressive disorder, but little is known about concomitant reduction in social-interpersonal dysfunction.
Method. We evaluated social-interpersonal functioning (self-reported social adjustment, interpersonal problems and dyadic adjustment) and depressive symptoms (two self-report and two clinician scales) in adult outpatients (n=156) with recurrent major depressive disorder at several points during a 20-session course of acute phase cognitive therapy. Consenting acute phase responders (n=84) entered a 2-year follow-up phase, which included an 8-month experimental trial comparing continuation phase cognitive therapy to assessment-only control.
Results. Social-interpersonal functioning improved after acute phase cognitive therapy (dyadic adjustment d=0.47; interpersonal problems d=0.91; social adjustment d=1.19), but less so than depressive symptoms (d=1.55). Improvement in depressive symptoms and social-interpersonal functioning were moderately to highly correlated (r=0.39–0.72). Improvement in depressive symptoms was partly independent of social-interpersonal functioning (r=0.55–0.81), but improvement in social-interpersonal functioning independent of change in depressive symptoms was not significant (r=0.01–0.06). In acute phase responders, continuation phase therapy did not further enhance social-interpersonal functioning, but improvements in social-interpersonal functioning were maintained through the follow-up.
Conclusions. Social-interpersonal functioning is improved after acute phase cognitive therapy and maintained in responders over 2 years. Improvement in social-interpersonal functioning is largely accounted for by decreases in depressive symptoms.
INTRODUCTION
Major depressive disorder often involves significant social-interpersonal dysfunction (e.g. Fredman et al. 1988; Gotlib & Lee, 1989; Leader & Klein, 1996; Zlotnick et al. 2000). Diagnosis requires an essential depressive symptom (depressed mood or anhedonia), additional depressive symptoms (e.g. neurovegetative signs, negatively focused cognition), and more general ‘functional impairment,’ which may include social-interpersonal dysfunction (APA, 1994). Cognitive therapy (Beck et al. 1979), focused on relieving depressive symptoms, has proven quite efficacious in this regard over decades of research (e.g. Jarrett & Rush, 1994; Craighead et al. 1998; Strunk & DeRubeis, 2001). In contrast, the extent to which concomitant social-interpersonal dysfunction, which may be a common motivation for seeking treatment (e.g. Meller et al. 1989; Wills & DePaulo, 1991), also improves with cognitive therapy is not nearly as well assessed or understood. In this report, we evaluate changes in multiple measures of depressive symptoms and self-reported social-interpersonal functioning across acute-phase cognitive therapy and a 2-year follow-up, including a randomized clinical trial comparing 8 months of a continuation cognitive therapy to an assessment-only control. Participants were adult outpatients with DSM-IV (APA, 1994) recurrent major depressive disorder with clear inter-episode recovery.
Although causal connections are not always clear, a large empirical literature strongly links depressive symptoms with social-interpersonal dysfunction. For example, poor social adjustment in various roles and contexts (e.g. as a worker or a parent, with friends or family, in leisure activities) has been linked with several depressive diagnoses (e.g. Fredman et al. 1988; Leader & Klein, 1996) and has been shown to improve (although not fully normalize) with remission (Weissman & Paykel, 1974). Moreover, interpersonal problems in depression involving maladaptive behaviors, thoughts and feelings in interpersonal situations (e.g. inappropriate negative self-disclosure, lower assertiveness; Segrin, 2000) predict negative mood (Coyne, 1976), perceptions of low social skill (Lewinsohn et al. 1980) and even social rejection (e.g. Joiner et al. 1992; Joiner, 1999) from depressed persons’ social interaction partners. Finally, discord in marriage and similar dyads correlates moderately with depressive symptoms (O’Leary et al. 1994) and major depressive disorder is associated with poor overall marital adjustment (Stravynski et al. 1995; Dudek et al. 2001), including unpleasant interactions with the spouse or partner (Zlotnick et al. 2000).
Unfortunately, there is also considerable evidence that a reduced level of social-interpersonal dysfunction often persists beyond remission of depression. For example, social functioning may improve less than depressive symptoms with treatment and remain impaired relative to control groups at longitudinal follow-up (Gotlib & Lee, 1989). Moreover, persons with major depressive disorder in remission may have poorer social functioning than those without a history of mental illness (Serretti et al. 1999) and poorer marital adjustment (as rated by spouses) than persons with bipolar disorder in remission (Horesh & Fennig, 2000).
Social-interpersonal functioning may improve with cognitive therapy for depression. For example, social adjustment improves comparably with cognitive therapy, interpersonal psychotherapy and pharmacotherapy plus clinical management (Imber et al. 1990); and partial responders to pharmacotherapy make gains in social adjustment with the addition of cognitive therapy (Scott et al. 2000). However, cognitive therapy for depressed wives may not produce significant gains in dyadic adjustment, whereas behavioral marital therapy does produce gains in dyadic adjustment (Beach & O’Leary, 1992). Deeper examination of improvement in social-interpersonal functioning with cognitive therapy would be of value to clinicians and researchers weighing this treatment for depression against alternatives such as interpersonal psychotherapy (Klerman et al. 1984), which has a stronger research base supporting its social-interpersonal benefits (e.g. Weissman et al. 1974, 1981; Mufson et al. 1999; O’Hara et al. 2000).
Researchers have just begun to address the question of whether social-interpersonal improvement is accounted for by, or independent of, reduction in depressive symptoms. Hirschfeld et al. (2002) compared change in social adjustment (on three self-report scales) with change in depressive symptoms (on one clinician-rated scale) in groups with major depressive disorder receiving pharmacotherapy (nefazodone), a newer form of cognitive-behavioral psychotherapy [Cognitive Behavioral Analysis System of Psychotherapy (CBASP); McCullough, 2000], or both treatments. Consistent with past research, depressive symptoms and social adjustment improved more in the combined treatment group than in the two single treatment groups, which did not differ significantly on these outcomes. In addition, social adjustment improved less than, and partly independently of, depressive symptoms.
The current investigation offers several methodological and conceptual strengths to address these questions. First, Jarrett et al. (2001) reported that, after response to acute phase cognitive therapy (A-CT; Beck et al. l979), continuation phase cognitive therapy (C-CT; Jarrett & Kraft, 1997; Jarrett et al. 1998) reduced depressive relapse and recurrence compared to the assessment-only control in the current sample. In the current report, we utilize Jarrett et al.’s clinical trial dataset to evaluate the effects of C-CT on self-reported social-interpersonal functioning. Second, we present follow-up data 12 and 24 months post-A-CT (4 and 16 months post randomization to C-CT or control) to clarify the duration or maintenance of social-interpersonal improvement. Third, we present results for multiple measures of self-reported social-interpersonal functioning (social adjustment, interpersonal problems, and dyadic adjustment). Finally, we consider the relative magnitude and clinical significance of changes in social-interpersonal functioning and evaluate outcomes relative to normative samples.
We hypothesized that social-interpersonal functioning would improve with A-CT, but not as much as depressive symptoms, which are the primary target of A-CT. Similarly, we hypothesized that C-CT would improve social-interpersonal functioning compared to the assessment-only control group. Finally, we hypothesized that improvement in social-interpersonal functioning would be maintained across the follow-up period.
METHOD
Participants
Participants were adult outpatients presenting with DSM-IV non-psychotic, recurrent, major depressive disorder (APA, 1994). Inclusion criteria included clear inter-depressive episode recovery (≥2 months of at least nearly normal functioning) and a score ≥16 on the 17-item Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960). Exclusion criteria included concurrent medical disorders potentially accounting for depressive symptoms, organic mental disorders, psychotic disorders, active substance abuse or dependence, primary obsessive compulsive or eating disorders, borderline personality disorder and inability or unwillingness to complete questionnaires or to comply with the treatment protocol. Participants were recruited though media, printed announcements and self- and practitioner referral. They completed telephone screening (n>3500), diagnostic interviews (n=608) and provided informed consent to enter the protocol (n 156). More detail about participants, recruitment, inclusion and exclusion criteria are available in Jarrett et al. (2001).
Study phases
Acute phase cognitive therapy
Acute phase cognitive therapy (A-CT; Beck et al. l979) was conducted by five experienced therapists within a 12–14 week protocol, including 20 individual sessions (50–60 min) held twice weekly for the first 8 weeks and once weekly for the last 4 weeks. No pharmacotherapy was provided. A-CT is designed to reduce depressive symptoms by eliciting thoughts associated with negative affect, teaching patients to evaluate the validity of such thoughts through logical and empirical methods, to generate more realistic alternatives when negative thoughts are not supported and to employ problem-solving skills when negative conclusions are warranted.
Experimental phase
A-CT responders who completed the post-A-CT assessment and consented to randomization (n=84) were assigned to either continuation phase cognitive therapy (C-CT; Jarrett & Kraft, 1997; Jarrett et al. 1998; n=41) or an assessment-only control condition (n=43). The C-CT protocol consisted of ten 60–90 min sessions of C-CT over 8 months (the first four sessions semi-monthly, and the next six sessions monthly) from the same therapist who had provided A-CT. C-CT is designed to prevent relapse and recurrence of depression through maintenance and generalization of skills learned in A-CT, reduction of residual depressive symptoms and preparation for current or anticipated vulnerabilities. In C-CT, patients are taught to use emotional distress and symptoms as cues to implement skills learned in A-CT. The patients in the assessment-only control attended evaluation visits scheduled at the same frequency as in C-CT. Evaluators of control patients were prohibited from using psychosocial interventions. Patients who relapsed during the experimental phase were asked to complete all sessions and referred for extra-protocol treatment if not receiving C-CT. Data collected after relapse are utilized in this report to increase the generalizability of findings.
Follow-up phase
All 84 patients entering the experimental phase were eligible for, and 74 entered, the follow-up phase.1,† This assessment-only period lasted 16 months beyond the experimental phase (24 months post-A-CT) and consisted of 10 sessions scheduled monthly at months 9–12 post-A-CT and bimonthly at months 14–24 post-A-CT. Patients who experienced relapse or recurrence of depression during follow-up were referred for extra-protocol treatment and followed naturalistically; their data are utilized in this report to increase generalizability.2
Assessment strategy and timing
Two pre-treatment assessments were used to establish eligibility for the study and to render diagnoses. Patients presented at the Department of Psychiatry at The University of Texas Southwestern Medical Center at Dallas and completed the Structured Clinical Interview for DSM-III-R (SCID outpatient version; Spitzer et al. 1989), with supplemental interview questions to assess DSM-IV disorders and subtypes, as well as other clinician-rated measures described below. The final assessment was conducted by a doctoral-level diagnostician. Inter-episode recovery and A-CT response definitions were chosen for consistency with the DSM (APA, 1994), consensual scientific definitions (Frank et al. 1991), and past research (e.g. Jarrett et al. 1998, 1999, 2001). Specifically, inter-episode recovery was defined as a return to more-or-less normal functioning for 2 or more months between major depressive episodes; and response was defined as not meeting criteria for current DSM major depressive disorder and an HRSD score of 9 or less when exiting or completing the A-CT protocol. Measures used in this report were completed: before A-CT session 1 (or at pre-treatment), at A-CT sessions 9 and 17; post-A-CT/pre-experimental phase (C-CT or assessment-only control); before experimental session 6; post-experimental phase; and 12 and 24 months post-A-CT (4 and 16 months post-experimental phase). As shown in Table 1, the sample size available for analysis varied due to missing data, attrition and the measure (i.e. participants not in committed, cohabitating romantic relationships did not complete the measure of dyadic adjustment described below).
Table 1.
Raw scale score descriptive statistics at each assessment
| Acute Phase Cognitive Therapy (A-CT) |
Continuation Phase Cognitive Therapy (C-CT) or control |
Post-A-CT follow-up |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Scale | Pre.* | Sess. 9 | Sess. 17 | Post. | Exit | Pre. | Sess. 6 | Post. | 12 mo. | 24 mo. |
| BDI | ||||||||||
| M | 24.78 | 13.57 | 9.23 | 7.57 | 9.35 | 3.81 | 6.30 | 4.79 | 5.27 | 3.81 |
| S.D. | 8.04 | 8.79 | 7.77 | 7.37 | 8.87 | 4.35 | 9.17 | 6.51 | 6.56 | 6.41 |
| n | 152 | 137 | 132 | 126 | 154 | 84 | 77 | 71 | 63 | 56 |
| HRSD | ||||||||||
| M | 18.41 | 8.91 | 6.64 | 7.42 | 8.22 | 3.62 | 5.31 | 4.12 | 4.63 | 4.06 |
| S.D. | 3.83 | 4.90 | 5.05 | 6.45 | 6.88 | 2.85 | 6.62 | 5.39 | 5.67 | 4.77 |
| n | 155 | 138 | 135 | 128 | 155 | 84 | 78 | 74 | 71 | 63 |
| IDSC | ||||||||||
| M | 33.14 | 17.38 | 12.66 | 13.12 | 14.60 | 6.31 | 8.87 | 7.21 | 7.35 | 6.52 |
| S.D. | 7.41 | 10.01 | 9.99 | 11.44 | 12.41 | 5.05 | 11.18 | 9.06 | 8.56 | 7.60 |
| n | 155 | 138 | 135 | 128 | 155 | 84 | 78 | 73 | 71 | 63 |
| IDSR | ||||||||||
| M | 37.47 | 21.13 | 14.77 | 13.02 | 15.40 | 7.63 | 9.45 | 8.79 | 8.55 | 6.46 |
| S.D. | 9.23 | 11.78 | 10.98 | 10.62 | 12.67 | 6.41 | 10.73 | 9.02 | 7.73 | 7.05 |
| n | 151 | 137 | 133 | 126 | 154 | 84 | 77 | 71 | 62 | 56 |
| SAS-SR | ||||||||||
| M | 2.52 | 2.12 | 1.93 | 1.82 | 1.92 | 1.64 | 1.72 | 1.67 | 1.66 | 1.59 |
| S.D. | 0.43 | 0.41 | 0.43 | 0.40 | 0.51 | 0.26 | 0.43 | 0.35 | 0.33 | 0.34 |
| n | 152 | 136 | 132 | 126 | 152 | 84 | 76 | 69 | 63 | 52 |
| IIP | ||||||||||
| M | 1.62 | — | — | 1.01 | 1.15 | 0.83 | 0.82 | 0.68 | 0.65 | 0.63 |
| S.D. | 0.53 | — | — | 0.55 | 0.64 | 0.48 | 0.60 | 0.51 | 0.50 | 0.52 |
| n | 147 | — | — | 122 | 147 | 83 | 76 | 69 | 62 | 51 |
| DYS | ||||||||||
| M | 88.24 | 91.65 | 95.27 | 97.69 | 94.37 | 101.96 | 97.45 | 101.57 | 106.82 | 105.46 |
| S.D. | 24.97 | 24.55 | 23.57 | 23.33 | 27.61 | 23.02 | 26.17 | 21.50 | 20.20 | 24.59 |
| n | 91 | 86 | 77 | 68 | 91 | 47 | 44 | 37 | 34 | 28 |
Pre., pre-treatment; Sess., session; Post., post-treatment; Exit, last available data point used in calculation of effect size and health statistics; Mo., months after completing A-CT; BDI, Beck Depression Inventory; HRSD, Hamilton Rating Scale for Depression; IDSC, Inventory of Depressive Symptomatology (clinician-report); IDSR, Inventory of Depressive Symptomatology (self-report); SAS-SR, Social Adjustment Scale – Self Report; IIP, Inventory of Interpersonal Problems; DYS, Dyadic Adjustment Scale; Follow-ups occurred 12 and 24 months post-A-CT, equivalent to 4 and 16 months post C-CT or assessment-only control.
Measures
Hamilton Rating Scale for Depression
The Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960) is a widely used, 17-item, clinician rating scale to assess severity of depressive symptoms. Scores range from 0 to 52, and higher values represent greater depressive symptoms. The scale has demonstrated good inter-rater reliability (r=0.85; Clark & Watson, 1991), adequate internal consistency (alphas of 0.88 and 0.89 in two large clinic samples; Rush et al. 1996), and appropriate convergence with self-report depressive symptom measures (r=0.70–0.83; Clark & Watson, 1991). In the current sample, alpha internal consistency was adequate (median=0.85, range=0.73–0.90) with the exception of the pre-A-CT assessment (0.34). However, because the pre-A-CT HRSD correlated highly (0.72) with the clinician version of the Inventory for Depressive Symptomatology (Rush et al. 1986, 1996; described below), we retained this data point.
Beck Depression Inventory
The Beck Depression Inventory (BDI; Beck et al. 1961) is a very widely used, 21-item, self-report measure of depressive symptom severity. Scores range from 0 to 63, and higher values represent greater depressive symptoms. Beck et al. (1988) reported an average internal consistency of 0.87, an average short-term (<1 month) retest reliability of 0.60 and considerable convergence with clinical ratings of depressive symptoms, the HRSD and other self-report measures of depressive symptoms. In the current sample, alpha internal consistency was good to excellent (median=0.92, range 0.85–0.= 95).
Inventory for Depressive Symptomatology
This 28-item scale (Rush et al. 1986, 1996) has both self-report (IDSR) and clinician (IDSC) versions to measure the severity of depressive symptoms. Scores range from 0 to 84, and higher values represent greater depressive symptoms. Rush et al. (1986) reported internal consistency reliabilities of 0.85 (IDSR) and 0.88 (IDSC), as well as moderate to high convergence with the BDI (IDSR r=0.78; IDSC r=0.61) and HRSD (IDSR r=0.67; IDSC r=0.92). In the current sample, alpha internal consistency was moderate to high for both the IDSC (median=0.89, range=0.61–0.94) and the IDSR (median = 0.90, range=0.76–0.93).
Social Adjustment Scale – Self Report
The Social Adjustment Scale – Self Report (SAS-SR; Weissman & Bothwell, 1976) is a 56-item self-report measure of functioning in several important social domains. Participants complete only those sections of the questionnaire reflecting their social roles (e.g. not all participants complete marital or parenting sections). Scores range from 1 to 5 and higher values represent poorer adjustment. In past research, internal consistency for the overall adjustment score was moderate (alpha=0.74) and temporal stability was good (r=0.80) across 2-week intervals (Edwards et al. 1978). Validity evidence includes appropriate patterns of mean differences, significant correlations with clinical ratings, and sensitivity to change in psychopathology (Weissman & Bothwell, 1976; Weissmann et al. 1978). In the current sample, alpha internal consistency was good (median= 0.85, range=0.80–0.90).
Inventory of Interpersonal Problems
The Inventory of Interpersonal Problems (IIP; Horowitz et al. 1988) is a 127-item self report scale of the extent to which a number of behaviors, thoughts and feelings have been problematic in one’s significant relationships. Scores range from 0 to 4 and higher values represent greater interpersonal problems. Horowitz et al. (1988) provide evidence of the measure’s reliability and validity, including a 10-week retest correlation of 0.98, moderate correlations with measures of psychiatric symptoms, and mean score decreases with psychotherapy. In the current sample, alpha internal consistency for the total score was very high (median=0.98, range=0.97–0.98), due in part to the large number of items. Consequently, we note that the average inter-item correlation also suggested adequate internal consistency (median=0.28, range=0.18–0.32).
Dyadic Adjustment Scale
The Dyadic Adjustment Scale (DYS; Spanier, 1976) is a 32-item, self-report inventory of positive adjustment and satisfaction in marital and similarly committed dyads. Scores range from 0 to 151, and higher values represent better adjustment. Although it is possible to derive subscales, most clinicians use the total score as a reflection of overall relationship quality (Spanier & Thompson, 1978). Spanier (1976) reported an internal consistency of 0.96, as well as evidence for both content and criterion-related validity. In the current sample, alpha internal consistency was also quite high (median =0.96, range=0.95–0.97).
Standardization of scores
To facilitate examination of changes in and among measures of social-interpersonal functioning, and comparisons of these changes with depressive symptoms, individual scales were placed on a common metric. All available cases at the pre-A-CT assessment were used to standardize measures at all assessments into T-score units (M=50, s.d.=10). The formula (e.g. see Minium et al. 1993) used to convert a person’s raw score x into a T score was:
This linear transformation does not alter the significance of statistical tests of change within measures (e.g. pre- versus post-treatment) but aids understanding of the magnitude of changes. After scale-level standardization, the four depressive symptom measures (BDI, HRSD, IDSC, IDSR) were averaged to form a single index and again standardized to maintain s.d.= 10 pre-A-CT. Averaging the four depression symptom reduced the number of statistical analyses and was justified empirically by cross-time factor analyses of the current data set (Vittengl, J. R., et al. unpublished observations) which indicated that the scales aggregated strongly by time (e.g. pre-treatment, post-treatment) rather than by method (self- or clinician-report) or measure. Similarly, alpha internal consistency for the 4-item depressive symptom index was high (median=0.95, range=0.89– 0.97). Although the primary analyses utilize the standardized measures, Table 1 contains descriptive statistics for the raw scales at each assessment.
Identification of healthy participants
Identification of participants in the ‘healthy’ range of social-interpersonal functioning was based on a cut-off of 1.28 s.d. from the mean of best available (although not matched) normative samples (i.e. about 10% of the population would be considered unhealthy). This value represents a compromise between the traditional cut-off of 2 s.d. (i.e. about 2% of the population would be considered unhealthy; see e.g. Jacobson & Truax, 1991) and evidence that psychopathology with attendant social-interpersonal dysfunction is more prevalent than 2% in epidemiological samples (e.g. Kessler & Zhao, 1999, reported a 12-month prevalence of about 31% for any disorder; Fredman et al. 1988, reported a 2-week prevalence of about 9% for any disorder). For the DYS, Spanier’s (1976) norms for married couples were employed. For the IIP, norms from a community sample nominated as mentally healthy by licensed psychologists (and so likely ‘super normal’) were pooled with an identically sized sample of college students (both datasets from Hansen & Lambert, 1996). Although not ideal demographically, the item mean of this pooled sample did not differ significantly from that of a US census-stratified sample completing an IIP short form (Horowitz et al. 2000). Finally, norms from a large community sample (Weissman et al. 1978) were available for the SAS-SR. Examination of stricter and more lenient health cut-offs, as well as score distributions, suggested that there were no clear health categories in the current sample, but the 1.28 s.d. cut-off provided heuristically valuable results.
Hypothesis-testing strategy
We based our primary hypothesis tests on ordinary least squares regression and analysis of variance. Linear mixed-effect models using likelihood estimation are becoming increasingly popular for analyzing datasets with similar structures, and offer power and interpretive advantages in some cases (e.g. Nich & Carroll, 1998; Kreft, 2000; Wallace & Green, 2002). In our dataset, however, linear mixed-effect analyses with the social-interpersonal measures yielded substantively equivalent results. Consequently, we present only the more widely understood ordinary least squares analyses here. In addition, due to the use of multiple measures and analyses, we selected a conservative alpha of 0.01, 2-tailed, for significance in all statistical tests and we focus on effect sizes and patterns of results in drawing conclusions. Effect sizes were computed with Cohen’s (1988) formulas and included (benchmarks for small, medium and large effects) r for bivariate correlation (0.10, 0.30, 0.50), d for t tests (0.20, 0.50, 0.80), and f for analysis of variance (0.10, 0.25, 0.40).
RESULTS
Sample characteristics
The sample entering A-CT consisted of 155 adult outpatients with DSM-IV recurrent major depressive disorder, including 74.2% females (the intention-to-treat sample of 156 included 1 participant who consented to A-CT but did not begin treatment). The mean age was 41.3 years (s.d.=11.0); the mean level of education was 15.4 years (s.d.=2.8); and 7.1% were African American, 4.5% Hispanic, 1.3% Native American and 87.1% White. The participants’ mean age of onset of major depressive disorder was 19.9 years (s.d.=9.6), and participants had experienced a mean of 3.4 major depressive episodes (s.d.=1.3). Prior treatment exposure data for participants’ first, most recent two and current major depressive episodes, indicated that 1.9% had been treated previously with electro-convulsive therapy, 56.8% with pharmacotherapy, 59.4% with psychotherapy and 41.3% with at least two of these types of therapy. In addition to the diagnosis of recurrent major depressive disorder, the number of DSMIV Axis I disorders pre-A-CT ranged from 0 to 4 (M=0.59; s.d.=0.78). Co-morbid Axis I disorders included social phobia (20.0%),3 specific phobias (12.3%), panic disorder without agoraphobia (8.4%), post-traumatic stress disorder (7.7%), dysthymic disorder (5.2%), obsessive-compulsive disorder (1.3%), panic disorder with agoraphobia (1.3%) and 0.6% each of agoraphobia without a history of panic disorder, attention deficit hyperactivity disorder, bulimia nervosa and hypochondriasis.
Previous outcome analyses with the current dataset
Jarrett et al. (2001) present greater detail about treatment outcome in the current dataset. Using the intention-to-treat sample (n=156), the response rate to A-CT when exiting A-CT was 62.6% (n=97) as rated by the therapist (when the participant attrited; n=10) or by an independent clinician (when the participant completed the post-A-CT assessment; n=87).4 These data are consistent with the research showing that A-CT reduces the symptoms of major depressive disorder in adults (e.g. Rush et al. 1977; Hollon et al. 1992; Jarrett et al. 1999). In addition, C-CT reduced relapse and recurrence of DSM-IV major depressive disorder over 8 months post-A-CT compared to the assessment-only control (10% v. 31%) in the current dataset.
Changes in social-interpersonal functioning across A-CT
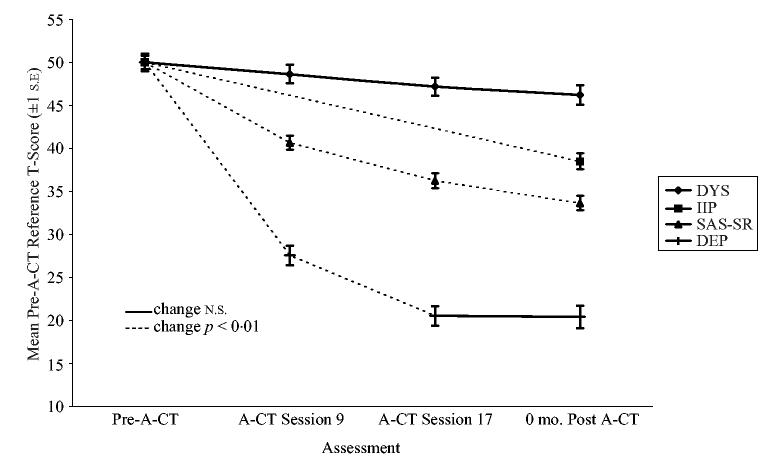
Fig. 1 depicts changes in the standardized SASSR, IIP, DYS and depressive symptom scores, using all available data at each assessment (see Table 1 for raw M and n). All changes (decreases) in the standardized scores represent improved social-interpersonal functioning relative to the pre-A-CT distributions (i.e. decreases in the SAS-SR represent improved social adjustment; and the DYS scale scores have been reflected such that decreases represent improved dyadic adjustment in contrast to the increasing raw score means shown in Table 1). The difference between the first and the last available A-CT assessments, regardless of therapy completion (i.e. 155 individuals began A-CT, 130 completed the A-CT protocol and 128 also completed the post-A-CT assessment) was used to compute effect sizes for overall change in measures. The DYS improved a small amount [d=0.47; t(90)=4.53, p<0.0001, 2-tailed], the IIP [d=0.91; t(146)=11.01, p<0.0001, 2-tailed] and SAS-SR [d=1.19; t(151)=14.67, p <0.0001, 2-tailed] improved a large amount and depressive symptoms improved by a very large amount [d=1.55; t(154)=19.31, p<0.0001, 2-tailed]. Moreover, the standardized depressive symptom index had decreased more than the three social-interpersonal measures at the session 9, session 17 and 0 months post-A-CT assessments, dependent t (67–135)>15.11, p<0.0001, 2-tailed, median d=1.59 (range 1.41–2.20).However, depressive symptoms improved mostly early in treatment with no significant change between session 17 and 0 months post-A-CT.
Fig. 1.
Changes in standardized social-interpersonal and depressive symptoms scales during acute phase cognitive therapy (A-CT) represent improved functioning. DYS, dyadic adjustment scale; IIP, Inventory of Interpersonal Problems; SAS-SR, Social Adjustment Scale – Self Report; DEP, Depressive symptoms index formed from two self-report and two clinician-report scales (see text for details); mo., months.
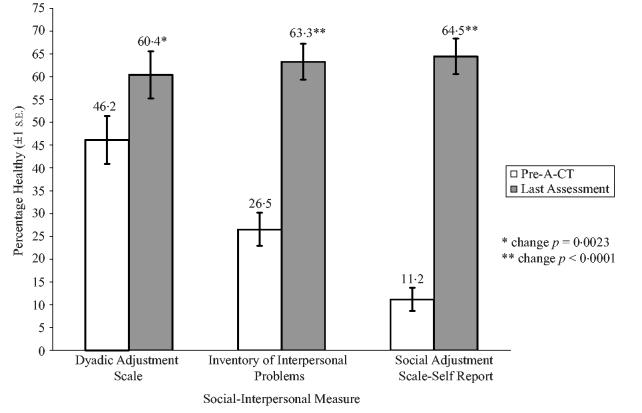
Social-interpersonal ‘health’ before and after A-CT
The first and last available A-CT assessments were used to calculate proportions in the estimated ‘healthy’ range of social-interpersonal functioning based on a cutoff of 1.28 s.d. from the mean of available normative samples (i.e. about 10% of the population would be considered unhealthy). Estimated proportions of healthy participants are depicted in Fig. 2. The three social-interpersonal measures yielded quite similar healthy proportions at exit (60–65%), and each increased significantly from pre-A-CT (p<0.003, 2-tailed, by McNemar’s test). Although the available normative samples were not matched to one another or to the current sample of depressed patients, results were parallel to continuous measures: The smallest change was in marital discord (DYS) and the greatest was in social role functioning (SAS-SR).
Fig. 2.
Percentage of social-interpersonally healthy individuals (at or below the 90th percentile of dysfunction in a normative sample) entering and exiting acute phase cognitive therapy (A-CT).
Correlated change in depressive symptoms and social-interpersonal functioning during A-CT
Because social-interpersonal functioning changed less than depressive symptoms, regressions were computed to determine to what degree changes in social-interpersonal functioning could be accounted for by change in depressive symptoms and vice versa. Specifically, change (pre-A-CT minus last A-CT assessment) in each social-interpersonal measure was predicted by change in depressive symptoms. From these regression equations, the t test for nonzero intercept reflects systematic change in social-interpersonal functioning independent of change in depressive symptoms. In each model, change in depressive symptoms was correlated moderately to highly with change in social-interpersonal functioning (r=0.36, 0.57 and 0.72, for the DYS, IIP and SAS-R, respectively, p<0.0005, 2-tailed), but there was no significant change in social-interpersonal functioning independent of change in depressive symptoms (converting t to r for effect sizes comparable to the correlations above, r=0.06, 0.01 and 0.05 for the DYS, IIP and SAS-SR, respectively, p>0.51, 2-tailed). Conversely, in a second set of regressions in which change in depressive symptoms was predicted by change in the social-interpersonal measures, depressive symptoms changed partly independently of the social-interpersonal measures singly (converting from t, r=0.81, 0.69 and 0.55, for prediction by the DYS, IIP and SAS-SR, respectively, p<0.0001, 2-tailed) and collectively (converting from t, r=0.48, p<0.0001, 2-tailed).
Our finding that social-interpersonal improvement was accounted for by change in depressive symptoms appeared to contradict Hirschfeld et al.’s (2002) recent report that social adjustment, as measured by the SAS-SR, improved partly independently of depressive symptoms, as measured by the HRSD. To help understand this difference, an additional series of regressions was run to predict change in the social-interpersonal measures (SAS-SR, IIP, DYS) from change in depressive symptom measures (HRSD, BDI, IDSC, IDSR) individually, instead of our multi-measure/multi-method depressive symptom index. In these regressions, the SAS-SR changed partly independently of the HRSD ( r=0.22, p=0.0067, 2-tailed), in replication of Hirschfeld et al. However, all other pairings of social-interpersonal and depressive symptom measures left no significant independent social-interpersonal change ( p>0.05, 2-tailed).
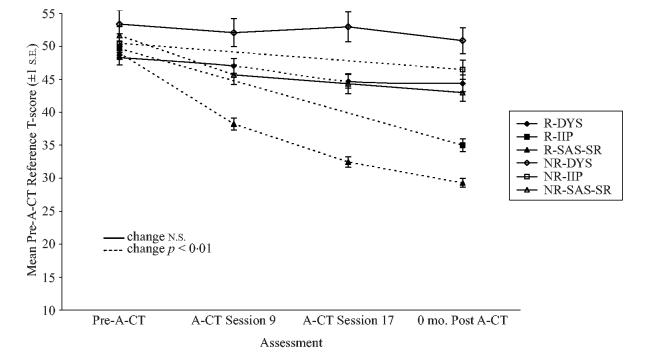
Differentiation of A-CT responders’ and non-responders’ social-interpersonal functioning
To understand better the relations between depressive symptoms and social-interpersonal change, we compared A-CT responders’ (absence of major depressive disorder and an HRSD score of 9 or less when exiting A-CT; n=97) and non-responders’ ( n=58) social-interpersonal functioning across A-CT. Plots of responders’ and non-responders’ standardized scores are shown in Fig. 3. As these plots suggest, responders and non-responders did not differ significantly at the pre-A-CT assessment on the SAS-SR or IIP ( p>0.10, 2-tailed), but there was a trend for better pre-A-CT functioning in responders on the DYS, t(89)=2.35, p=0.021, 2-tailed, d=0.52. Consequently, pre-A-CT scores were controlled in analyses of covariance comparing responders and nonresponders at later assessments for each measure. Responders showed better social-interpersonal functioning at the later A-CT assessments on the SAS-SR (session 9, session 17 and post-A-CT) and the IIP (post-A-CT), F(1, 115–132)>19.87, p<0.0001, median f=0.66 (range 0.39–0.92). For the DYS, responders and non-responders did not differ at A-CT session 9 ( p=0.32), but responders functioned better at A-CT session 17, F(1, 72)=7.64, p=0.0037, f=0.33 and marginally better post-A-CT, F(1, 63)=4.51, p=0.038, f=0.27.
Fig. 3.
Acute phase cognitive therapy (A-CT) responders’ (R) and non-responders’ (NR) standardized social-interpersonal functioning and depressive symptoms. DYS, dyadic adjustment scale; IIP, Inventory of Interpersonal Problems; SAS-SR, Social Adjustment Scale – Self Report; DEP, Depressive symptoms index formed from two self-report and two clinician-report scales (see text for details); mo., months.
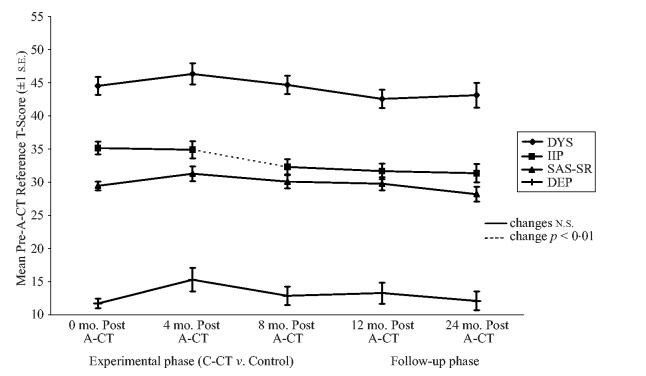
Changes in social-interpersonal functioning across experimental and follow-up phases
Differences between the C-CT and control groups on the SAS-SR, IIP and DYS were evaluated pre-C-CT (0 months post-A-CT), at C-CT session 6 (4 months post-A-CT), post C-CT (8 months post-A-CT), 4 months post CCT (12 months post-A-CT) and 16 months post C-CT (24 months post-A-CT), but no significant differences were detected ( p>0.05, 2-tailed, with pairwise deletion of cases with missing data using t tests at each assessment; with listwise deletion of cases with missing data using repeated-measures ANOVAs; and with all cases having at least one non-missing assessment included in linear mixed-effect analyses). However, the C-CT group had numerically (but not statistically significantly) better average functioning than the control group on the SASSR, IIP and DYS at the 4, 6, 8, 12 and 24 month assessments (with the exception of the DAS at the 4 month post-A-CT assessment) suggesting that the lack of statistically significant effects might relate to low statistical power. Conversely, the observed effect sizes for C-CT were typically small for the SAS-SR, IIP and DYS, at the four post-A-CT assessments (median d=0.34, range=x0.11–0.66), suggesting that clinical significance would be marginal, even if a larger sample had supported statistical significance. Based on these findings, Fig. 4 depicts standardized means after pooling the C-CT and control groups (see Table 1 for raw M). Two conclusions are evident in this sample of A-CT responders. First, social-interpersonal functioning was relatively stable, with no notable further improvement in functioning across the experimental or follow-up phases of the study. Second, there was a clear ordering of these variables with each maintaining its level of improvement relative to pre-A-CT scores and depressive symptoms.
Fig. 4.
Social-interpersonal functioning after acute phase cognitive therapy (A-CT) for pooled continuation phase cognitive therapy (C-CT) and control groups. DYS, dyadic adjustment scale; IIP, Inventory of Interpersonal Problems; SAS-SR, Social Adjustment Scale – Self Report; DEP, Depressive symptoms index formed from two self-report and two clinician-report scales (see text for details); mo., months.
DISCUSSION
The results of this study supported our first hypothesis that social-interpersonal functioning would improve after A-CT in a sample of adult outpatients with recurrent major depressive disorder. Three major domains of self-reported social-interpersonal functioning – social adjustment, interpersonal problems, and dyadic adjustment – improved significantly across A-CT; however, none improved as much as depressive symptoms relative to the pre-A-CT distribution. Similarly, effect sizes indicated a substantial decrease in depressive symptoms, less substantial but clinically significant improvement in social adjustment and interpersonal problems, and statistically, but likely less clinically, significant improvement in dyadic adjustment.
Regarding potential mechanisms for improvement, social-interpersonal improvement was largely accounted for by change in depressive symptoms across A-CT. In contrast, Hirschfeld et al. (2002) found that social adjustment, measured by the SAS-SR, improved partly independently of depressive symptoms, measured by the HRSD. In our data set, too, when only the clinician-rated HRSD was controlled, as opposed to our multi-measure/multi-method depressive symptom index, the SAS-SR changed partly independently. This significant independent change in a social-interpersonal measure was unique to the pairing of the HRSD with the SAS-SR, however; there was no significant independent change in the DYS or IIP when controlling the HRSD and no significant independent change in any of the social-interpersonal measures when controlling the other depressive symptom measures (BDI, IDSC, IDSR) individually, given the current moderate sample size. Consequently, we speculate that the HRSD taps aspects of depressive symptoms less overlapping with social adjustment than other commonly used depressive symptom measures. Further research involving multiple measures of both depressive symptoms and specific social-interpersonal constructs would help clarify this fundamental issue.
Our finding that most social-interpersonal improvement was accounted for by reduction in depressive symptoms is consistent with past research, including equivalent social adjustment outcomes among cognitive therapy, interpersonal therapy, imiprimine plus clinical management, and pill placebo plus clinical management groups in the NIMH Treatment of Depression Collaborative Research Program (Imber et al. 1990); and pharmacotherapy alone improving social adjustment (e.g. Kocsis et al. 1997). Consequently, we speculate that focusing primarily on depressive symptom reduction in A-CT does not detract from, and may even promote, improvement in social adjustment. Moreover, the current results are consistent with amelioration of depressive symptoms leading to improved social-interpersonal functioning, an idea that corresponds with the complex social-behavioral impairments in depression (e.g. problems in speech content and style, facial expression and gaze, and bodily posture and gestures; Segrin, 2000). Data structures allowing fine-grained time-lagged analyses (e.g. social-interpersonal functioning and depressive symptoms assessed at every therapy session) would be useful in testing potential causal relations among these constructs.
Dyadic adjustment changed relatively little across A-CT, compared to greater change in social adjustment and interpersonal problems. We speculate that dyadic adjustment improved less because it was less strongly associated with depressive symptom severity, which accounted for all significant change in social-interpersonal functioning and because it was less normatively impaired pre-A-CT, which left less room for improvement. This interpretation is consistent with past research. For example, the current sample’s DYS scores were similar to other depressed samples pre-A-CT and to remitted samples post-A-CT (e.g. Dobson, 1987). Moreover, the magnitude of association between dyadic adjustment and depressive symptom severity was consistent with previous reports (e.g. Olin & Fenell, 1989). Our finding of less improvement in dyadic adjustment also may reflect the fact that relationship partners did not participate in the therapy protocol. This is consistent with past research suggesting that behavioral marital (involving both partners), but not cognitive (involving only one partner), therapy for depression improves dyadic adjustment (Jacobson et al. 1991; Beach & O’Leary, 1992). We speculate that substantial improvement in dyadic adjustment often requires a treatment targeting relationship satisfaction and involving both partners.
Our second hypothesis that C-CT would further improve social-interpersonal functioning after A-CT was not supported. For those responding to A-CT, who demonstrated larger gains in social-interpersonal functioning than non-responders, C-CT did not significantly enhance social-interpersonal functioning compared to an assessment-only control. In contrast, C-CT does appear helpful in reducing risk of relapse of major depressive disorder over 8 months post-A-CT (Jarrett et al. 1998, 2001). Because our data suggest that depressive symptoms change partly independently of social-interpersonal functioning, we speculate that C-CT’s power to reduce relapse does not generalize to substantial social-interpersonal benefits. Instead, the potential gains in social-interpersonal functioning amenable to cognitive therapy may occur in a 20-session course of A-CT, leaving little room for additional improvement with C-CT. At the same time, we note that approximately 35–40% of the sample entering C-CT needed some yet-to-be-identified intervention to reach the estimated healthy range of social-interpersonal functioning.
Consistent with our third hypothesis, gains in social-interpersonal functioning were maintained across the follow-up period. Both at 12 and 24 months post-A-CT, SAS-SR, IIP and DYS scores were similar to previous assessments at 0, 4 and 8 months post-A-CT. That is, the relatively large improvements in social adjustment and interpersonal problems, and small improvements in dyadic adjustment, were maintained across a 2-year period. These data demonstrate for the first time the long-term maintenance of positive social-interpersonal outcomes of A-CT, as well as add to the large database supporting A-CT’s efficacy in reducing depressive symptoms (e.g. Jarrett & Rush, 1994; Craighead et al. 1998; Strunk & DeRubeis, 2001).
The current study involves noteworthy limitations. Perhaps most importantly, changes in social-interpersonal functioning with A-CT were not compared with no treatment, a waitlist control, or pharmacotherapy. Consequently, improvement in social-interpersonal functioning cannot be strongly attributed to A-CT relative to a comparison condition. Research demonstrating the efficacy of A-CT in reducing depression in controlled trials (e.g. Jarrett et al. 1999) may reduce, but cannot eliminate, this limitation of the current design.
Moreover, social-interpersonal functioning was assessed only by self-report. Consequently, changes in social-interpersonal functioning may represent subjective experiences rather than independently observable behavioral change. Research documenting the correspondence of the current social-interpersonal measures with others’ ratings of the same constructs (e.g. Weissman & Bothwell, 1976; Horowitz et al. 1988; Dudek et al. 2001; Ready & Clark, 2002) lessens but does not eliminate this concern. Future research using additional methods to assess social-interpersonal functioning (e.g. collateral reports; behavioral observations) would make valuable contributions.
Finally, it is possible that a shared negative affectivity component accounts for observed associations among social-interpersonal and depressive symptoms measures (e.g. see Watson & Clark, 1984). Although negative affectivity has been separated from the unique components of depressive symptoms (e.g. Clark & Watson, 1991; Watson et al. 1995), comparable work remains for social-interpersonal functioning measures. Discriminant validity in measurement would be an asset in future investigations of concomitant change in depressive symptoms and social-interpersonal functioning. However, elsewhere (Clark et al. 2003) we present analyses from the current sample indicating that the overlap among the SAS-SR and IIP and additional psychosocial measures, which related strongly to a measure of trait negative affectivity, is more predictive of depressive symptoms than unique components of the measures. Consequently, efforts to isolate highly discriminant components of social-interpersonal measures may prove challenging.
The maintenance of gains in social-interpersonal functioning across 2 years clarifies the potential benefit of A-CT for individuals with recurrent major depressive disorder. Further, the finding that C-CT did not further improve social-interpersonal functioning suggests that the potential social-interpersonal benefits may be achieved over a typical course of A-CT. Additional research is necessary to conclude definitively that A-CT improves social-interpersonal functioning, and that this improvement is governed by changing depressive symptoms. In future research aimed at clarifying the meaning and causes of social-interpersonal improvements, the results of the current study further highlight the value of multi-measure assessment of the complex constructs of depressive symptoms and social-interpersonal functioning.
ACKNOWLEDGEMENTS
The clinical trial was conducted at the University of Texas Southwestern Medical Center as Dallas, Department of Psychiatry, in the Psychosocial Research and Depression Clinic directed by Dr Jarrett and was supported in part by grants MH-38238 and MH-01571 from the National Institute of Mental Health, Bethesda, MD (Dr Jarrett). Gratitude is expressed to our colleagues for contributing to this research. Dolores Kraft, Ph.D., coordinated the trial and provided clinical support. Jeanette Doyle, M.A., Greg Eaves, Ph.D., Paul Silver, Ph.D., Marjorie Woodruff, Ph.D., Bethany Hampton, Ph.D., Catherine Judd, P. A.-C., M.S., Douglas Lisle, Ph.D., Regina Kinney, Ph.D., Maria Marwill-Magee, Ph.D., Andrew Clifford, Ph.D., Martin Schaffer, M.D., and Rodger Kobes, M.D., also provided clinical support. Research support was provided by Barbara Foster, Ph.D., Michelle White, B.S., Edna Christian, M.A., Joseph Begue, B.A., Julie Lowe, B.A., Daisha Cipher, Ph.D., Patricia Green, M.S., Demetria Clinton, B.A., and Paula Reese. Brian F. Shaw, Ph.D., rated the cognitive therapists. We appreciate the administrative support of both Eric J. Nestler, M.D., Ph.D. (The Lou and Ellen McGinley Distinguished Chair in Psychiatric Research and current chair), and Kenneth Z. Altshuler, M.D. (Stanton Sharp Professor and previous chair), Department of Psychiatry, The University of Texas Southwestern Medical Center at Dallas.
Footnotes
The notes will be found on p. 656.
Jarrett et al. (2001) reported n=60 entering the follow-up phase because the data from 14 patients who met criteria for relapse or recurrence of DSM-IV major depressive disorder during the experimental phase were censored. In the current analyses, all available data, including those collected after relapse or recurrence, were utilized to maximize the generalizability of findings.
The Longitudinal Interval Follow-up Evaluation structured interview (Keller et al. 1987), was administered 4, 8, 12 and 24 months post-ACT, respectively, and indicated that 15.4, 27.8, 38.9 and 44.1% of the assessment-only group, and 10.3, 7.9, 25.0 and 41.9% of the C-CT group, reported receiving extra-protocol treatment (i.e. pharmacotherapy and/or psychotherapy) in the interval since the previous assessment.
Substantial co-morbidity of anxiety and unipolar mood disorders is common (e.g. Mineka et al. 1998). However, co-morbid social phobia was potentially problematic given our focus on social-interpersonal functioning. The subsample with social phobia had poorer social adjustment, more interpersonal problems, and greater depressive symptoms pre-A-CT (p<0.01), as one would expect, but dyadic adjustment did not differ. By 0 months post-A-CT and throughout the experimental and follow-up phases, however, the sub-sample with an initial diagnosis of social phobia did not differ significantly from the subsample not co-morbid for social phobia (p>0.05). Consequently, co-morbid social phobia did not interfere with hypothesis tests.
Jarrett et al. (2001) reported n=87 treatment responders, according to ratings made by an independent evaluator, and consistent with their focus on participants eligible to enter C-CT (i.e. those who completed the A-CT protocol and the post-treatment assessment, in addition to the absence of DSM-IV major depressive disorder and an HRSD score of 9 or less).
REFERENCES
- Diagnostic and Statistical Manual of Mental Disorders. 4th edn American Psychiatric Press; Washington, DC: 1994. [Google Scholar]
- Beach SRH, O’Leary DK. Treating depression in the context of marital discord: outcome and predictors of response of marital therapy versus cognitive therapy. Behavior Therapy. 1992;23:507–528. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. Guilford Press; New York: 1979. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Clark LA, Vittengl JR, Kraft D, Jarrett RB. Shared, not unique, components of personality and psychosocial functioning predict depression severity after acute-phase cognitive therapy. Journal of Personality Disorders. 2003;17:406–430. doi: 10.1521/pedi.17.5.406.22975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–333. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analyses for the Behavioral Sciences. 2nd Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- Coyne JC. Depression and the response of others. Journal of Abnormal Psychology. 1976;85:186–193. doi: 10.1037//0021-843x.85.2.186. [DOI] [PubMed] [Google Scholar]
- Craighead WE, Craighead LW, Ilardi SS. Psychosocial treatments for major depressive disorder. In: Nathan PE, Gorman JM, editors. A Guide to Treatments that Work. Oxford University Press; New York: 1998. pp. 226–239. [Google Scholar]
- Dobson KS. Marital and social adjustment in depressed and remarried women. Journal of Clinical Psychology. 1987;43:261–265. doi: 10.1002/1097-4679(198703)43:2<261::aid-jclp2270430216>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Dudek D, Zieba A, Jawor M, Szymaczek M, Opila J, Dattilio FM. The impact of depressive illness on spouses of depressed patients. Journal of Cognitive Psychotherapy. 2001;15:49–57. [Google Scholar]
- Edwards DW, Yarvis RM, Mueller DP, Zingale HC, Wagman WJ. Test-taking and the stability of adjustment scales: can we assess patient deterioration? Evaluation Quarterly. 1978;2:275–291. [Google Scholar]
- Frank E, Prien R, Jarrett RB, Keller MB, Kupfer DJ, Lavori PW, et al. Conceptualization and rationale for consensus definitions of terms in major depressive disorder: remission, recovery, relapse, recurrence. Archives of General Psychiatry. 1991;48:851–855. doi: 10.1001/archpsyc.1991.01810330075011. [DOI] [PubMed] [Google Scholar]
- Fredman L, Weissman MW, Leaf PJ, Bruce ML. Social functioning in community residents with depression and other psychiatric disorders: results of the New Haven epidemio-logic catchment area study. Journal of Affective Disorders. 1988;15:103–112. doi: 10.1016/0165-0327(88)90077-8. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, Lee CM. The social functioning of depressed patients: a longitudinal study. Journal of Social and Clinical Psychology. 1989;8:223–237. [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen NB, Lambert MJ. Assessing clinical significance using the Inventory of Interpersonal Problems. Assessment. 1996;3:133–136. [Google Scholar]
- Hirschfeld RMA, Dunner DL, Keitner G, Klein DN, Koran LM, Kornstein SG, et al. Does psychosocial functioning improve independent of depressive symptoms? A comparison of nefazodone, psychotherapy, and their combination. Biological Psychiatry. 2002;51:123–133. doi: 10.1016/s0006-3223(01)01291-4. [DOI] [PubMed] [Google Scholar]
- Hollon SD, DeRubeis RJ, Evans MD, Wiemer MJ, Garvey MJ, Grove WM, et al. Cognitive therapy and pharmacotherapy for depression: singly and in combination. Archives of General Psychiatry. 1992;49:774–781. doi: 10.1001/archpsyc.1992.01820100018004. [DOI] [PubMed] [Google Scholar]
- Horesh N, Fennig S. Perception of spouses and relationships: a matched control study of patients with severe affective disorder in remission and their spouses. Journal of Nervous and Mental Disease. 2000;188:463–466. doi: 10.1097/00005053-200007000-00012. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Alden LE, Wiggins JS, Pincus AL. Inventory of Interpersonal Problems Manual. The Psychological Corporation; Odessa, FL: 2000. [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureño G, Villaseñor VS. Inventory of interpersonal problems: psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- Imber SD, Pilkonis PA, Sotsky SM, Elkin I, Watkins JT, Collins JF, et al. Mode-specific effects among three treatment for depression. Journal of Consulting and Clinical Psychology. 1990;58:352–359. doi: 10.1037//0022-006x.58.3.352. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Dobson K, Fruzzetti AE, Schmaling KB, Salusky S. Marital therapy as a treatment for depression. Journal of Consulting and Clinical Psychology. 1991;59:547–557. doi: 10.1037//0022-006x.59.4.547. [DOI] [PubMed] [Google Scholar]
- Jacobson NS, Truax P. Clinical significance: a statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology. 1991;59:12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- Jarrett RB, Basco MR, Risser R, Ramanan J, Marwill M, Kraft D, et al. Is there a role for continuation phase cognitive therapy for depressed outpatients? Journal of Consulting and Clinical Psychology. 1998;66:1036–1040. doi: 10.1037//0022-006x.66.6.1036. [DOI] [PubMed] [Google Scholar]
- Jarrett RB, Kraft D. Prophylactic cognitive therapy for major depressive disorder. In Session: Psychotherapy in Practice. 1997;3:65–79. [Google Scholar]
- Jarrett RB, Kraft D, Doyle J, Foster BM, Eaves GG, Silver PC. Preventing recurrent depression using cognitive therapy with and without a continuation phase: a randomized clinical trial. Archives of General Psychiatry. 2001;58:381–388. doi: 10.1001/archpsyc.58.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett RB, Rush AJ. Short-term psychotherapy of depressive disorders: current status and future directions. Psychiatry: Interpersonal & Biological Processes. 1994;57:115–132. doi: 10.1080/00332747.1994.11024675. [DOI] [PubMed] [Google Scholar]
- Jarrett RB, Schaffer M, McIntire D, Witt-Browder A, Kraft D, Risser RC. Treatment of atypical depression with cognitive therapy or phenelzine: a double-blind, placebo-controlled trial. Archives of General Psychiatry. 1999;56:431–437. doi: 10.1001/archpsyc.56.5.431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joiner TE. A test of interpersonal theory of depression in youth psychiatric patients. Journal of Abnormal Child Psychology. 1999;27:77–85. doi: 10.1023/a:1022666424731. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jr., Alfano MS, Metalsky GI. When depression breeds contempt: reassurance seeking, self-esteem, and rejection of depressed college students by their roommates. Journal of Abnormal Psychology. 1992;101:165–173. doi: 10.1037//0021-843x.101.1.165. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Methodology, design, and evaluation in psychotherapy research. In: Bergin AE, Garfield SL, editors. Handbook of Psychotherapy and Behavior Change. 4th edn Wiley; New York: 1994. pp. 19–71. [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, et al. The longitudinal interval follow-up evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Zhao S. Overview of descriptive epidemiology of mental disorders. In: Aneshensel CS, Phelan JC, editors. Handbook of the Sociology of Mental Health. Kluwer Academic/Plenum; New York: 1999. pp. 127–150. [Google Scholar]
- Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal Psychotherapy of Depression. Basic Books; New York: 1984. [Google Scholar]
- Kocsis JH, Zisook S, Davidson J, Shelton R, Yonkers K, Hellerstein DJ, et al. Double-blind comparison of sertraline, imiprimine, and placebo in the treatment of dysthymia: psychosocial outcomes. American Journal of Psychiatry. 1997;154:390–395. doi: 10.1176/ajp.154.3.390. [DOI] [PubMed] [Google Scholar]
- Kreft IGG. Using random coeffcient linear models for the analysis of hierarchically nested data. In: Tinsley HA, Brown SD, editors. Handbook of Applied Multivariate Statistics and Mathematical Modeling. Academic Press; San Diego: 2000. pp. 613–639. [Google Scholar]
- Leader JB, Klein DN. Social adjustment in dysthymia, double depression and episodic major depression. Journal of Affective Disorders. 1996;37:91–101. doi: 10.1016/0165-0327(95)00076-3. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Mischel W, Chaplin W, Barton R. Social competence and depression: the role of illusory self-perceptions. Journal of Abnormal Psychology. 1980;89:203–212. doi: 10.1037//0021-843x.89.2.203. [DOI] [PubMed] [Google Scholar]
- McCullough JP., Jr. Treatment for Chronic Depression : Cognitive Behavioral Analysis System of Psychotherapy (CBASP) Guilford; New York: 2000. [DOI] [PubMed] [Google Scholar]
- Meller I, Fichter M, Weyeyer S, Witzke W. The use of psychiatric facilities by depressives: results of the Upper Bavarian study. Acta Psychiatrica Scandinavica. 1989;79:27–31. doi: 10.1111/j.1600-0447.1989.tb09230.x. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Minium EW, King BW, Bear G. Statistical Reasoning in Psychology and Education. 3rd edn Wiley; New York: 1993. [Google Scholar]
- Mufson L, Weissman MM, Moreau D, Garfinkel R. Effcacy of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry. 1999;56:573–579. doi: 10.1001/archpsyc.56.6.573. [DOI] [PubMed] [Google Scholar]
- Nich C, Carroll K. Now you see it, now you don’t: a comparison of traditional versus random-effects regression models in the analysis of longitudinal follow-up data from a clinical trial. Journal of Consulting and Clinical Psychology. 1998;65:252–261. doi: 10.1037//0022-006x.65.2.252. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Stuart S, Gorman LL, Wenzel A. Effcacy of interpersonal psychotherapy for postpartum depression. Archives of General Psychiatry. 2000;57:1039–1045. doi: 10.1001/archpsyc.57.11.1039. [DOI] [PubMed] [Google Scholar]
- Olin GV, Fenell DL. The relationship between depression and marital adjustment in a general population. Family Therapy. 1989;16:11–20. [Google Scholar]
- O’Leary KD, Christian JL, Mendell NR. A closer look at the link between marital discord and depressive symptomatology. Journal of Social and Clinical Psychology. 1994;13:33–41. [Google Scholar]
- Ready RE, Clark LA. Correspondence of psychiatric patient and informant ratings of personality traits, temperament, and interpersonal problems. Psychological Assessment. 2002;14:39–49. [PubMed] [Google Scholar]
- Rush AJ, Beck AT, Kovacs M, Hollon SD. Comparative effcacy of cognitive therapy and pharmacotherapy in the treatment of depressed outpatients. Cognitive Therapy and Research. 1977;1:17–37. [Google Scholar]
- Rush AJ, Giles DE, Schlesser MA, Fulton CL, Weissenburger JE, Burns CT. The Inventory for Depressive Symptomatology (IDS): preliminary findings. Psychiatry Research. 1986;18:65–87. doi: 10.1016/0165-1781(86)90060-0. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS): psychometric properties. Psychological Medicine. 1996;26:477–486. doi: 10.1017/s0033291700035558. [DOI] [PubMed] [Google Scholar]
- Scott J, Teasdale JD, Paykel ES, Johnson AL, Abbott R, Hayhurst H, et al. Effects of cognitive therapy on psychological symptoms and social functioning in residual depression. British Journal of Psychiatry. 2000;177:440–446. doi: 10.1192/bjp.177.5.440. [DOI] [PubMed] [Google Scholar]
- Segrin C. Social skills deficits associated with depression. Clinical Psychology Review. 2000;20:379–403. doi: 10.1016/s0272-7358(98)00104-4. [DOI] [PubMed] [Google Scholar]
- Serretti A, Cavallini MC, Macciardi F, Namia C, Franchini L, Sourey D, et al. Social adjustment and self-esteem in remitted patients with mood disorders. European Psychiatry. 1999;14:137–142. doi: 10.1016/s0924-9338(99)80731-7. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment : new scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976;38:15–28. [Google Scholar]
- Spanier GB, Thompson L. A confirmatory analysis of the Dyadic Adjustment Scale. Journal of Marriage and the Family. 1978;40:731–738. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R-Outpatient Version (with Psychotic Screen) New York State Psychiatric Institute; New York: 1989. [Google Scholar]
- Stravynski A, Tremblay M, Verreault R. Marital adjustment and depression. Psychopathology. 1995;28:112–117. doi: 10.1159/000284908. [DOI] [PubMed] [Google Scholar]
- Strunk DR, DeRubeis RJ. Cognitive therapy for depression: a review of its effcacy. Journal of Cognitive Psychotherapy: An International Quarterly. 2001;15:289–297. [Google Scholar]
- Wallace D, Green SB. Analysis of repeated measures designs with linear mixed models. In: Moskowitz DS, Hershberger SL, editors. Modeling Intra-individual Variability with Repeated Measures Data: Methods and Applications. Lawrence Erlbaum Associates; Mahwah, NJ: 2002. pp. 103–134. [Google Scholar]
- Watson D, Clark LA. Negative affectivity: the disposition to experience aversive emotional states. Psychological Bulletin. 1984;96:465–490. [PubMed] [Google Scholar]
- Watson D, Clark LA, Weber K, Assenheimer JS, Strauss ME, McCormick RA. Testing a tripartite model. II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. Journal of Abnormal Psychology. 1995;104:15–25. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bothwell S. Assessment of social-adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL, Paykel ES, Prusoff B, Hanson B. Treatment effects on the social adjustment of depressed patients. Archives of General Psychiatry. 1974;30:771–778. doi: 10.1001/archpsyc.1974.01760120033006. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL, Prusoff BA, Sholomskas D, Padian N. Depressed outpatients: results one year after treatment with drugs and/or interpersonal psychotherapy. Archives of General Psychiatry. 1981;38:51–55. doi: 10.1001/archpsyc.1981.01780260053005. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Paykel ES. The Depressed Woman: A Study of Social Relationships. University of Chicago Press; Chicago, IL: 1974. [Google Scholar]
- Weissman MM, Prusoff BA, Thompson WD, Harding PS, Myers JK. Social adjustment by self-report in a community sample and in psychiatric outpatients. Journal of Nervous and Mental Disease. 1978;166:317–326. doi: 10.1097/00005053-197805000-00002. [DOI] [PubMed] [Google Scholar]
- Wills TA, DePaulo BM. Interpersonal analysis of the help-seeking process. In: Snyder CR, Forsyth DR, editors. Handbook of Social and Clinical Psychology: The Health Perspective. Pergamon; New York: 1991. pp. 350–375. [Google Scholar]
- Zlotnick C, Kohn R, Keitner G, Della Grotta SA. The relationship between quality of interpersonal relationships and major depressive disorder: findings from the National Comorbidity Survey. Journal of Affective Disorders. 2000;59:205–215. doi: 10.1016/s0165-0327(99)00153-6. [DOI] [PubMed] [Google Scholar]