Abstract
OBJECTIVE—To assess the efficacy and safety of sulphasalazine in reactive arthritis. METHODS—Double blind placebo controlled trial of six months duration comparing sulphasalazine 2-3 g per day (n = 37) with matching placebo (n = 42) in adults with active reactive arthritis (age 19-57 years, median 34). Treatment response was evaluated once a month by changes in erythrocyte sedimentation rate (ESR), pain, peripheral arthritis, tender iliosacral joints, entesopathy, extra-articular manifestations, and working ability. RESULTS—15 patients in the sulphasalazine group and eight in the placebo group withdrew from the study prematurely. Adverse events, primarily gastrointestinal, were the main reason for withdrawal in the actively treated group. Intention-to-treat analyses showed significant improvements over time in both groups in ESR, pain, and number of swollen joints (P < 0.01). Number of days on sick leave decreased significantly in the sulphasalazine group only (P < 0.01). No significant differences between the two groups were present after six months. Among the patients completing the trial according to protocol, persistent complete remission had occurred within two months in five (23%) of the actively treated, but in no placebo treated patients (P = 0.013). CONCLUSIONS—Sulphasalazine seemed to improve only the very short term outcome of reactive arthritis. The possible beneficial effect of the drug should also be weighed against the risk of adverse events. Although these were mainly mild, almost 25% of the patients in the actively treated group gave up treatment for this reason.
Full Text
The Full Text of this article is available as a PDF (136.9 KB).
Figure 1 .
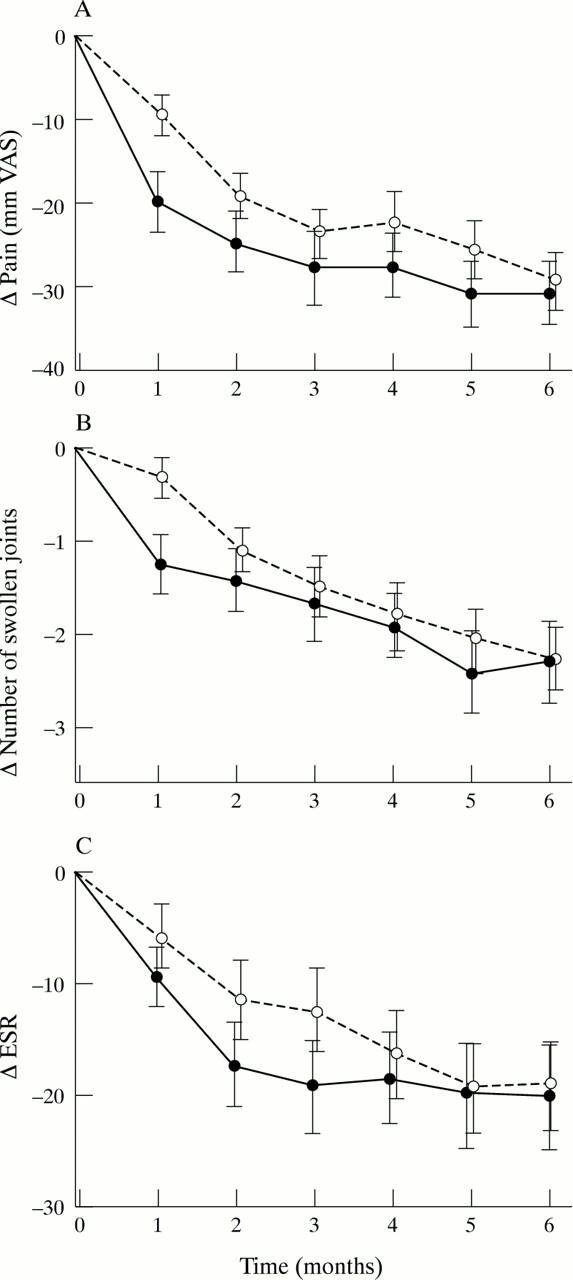
Changes over time in pain (A), number of swollen joints (B), and ESR (C) in patients treated with sulphasalazine (n = 37) and placebo (n = 42). Intention-to-treat analysis. Values are means, error bars = SEM. Decrease over time: P < 0.01 in both groups for all three variables. Difference between groups over time: NS. Sulphasalazine • ; placebo ∘
Figure 2 .
Number of patients in persistent complete remission (for definition see text) in patients treated with sulphasalazine (n = 22) and placebo (n = 34). Completer analysis. Sulphasalazine • ; placebo ∘ . *P = 0.013
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dougados M., Maetzel A., Mijiyawa M., Amor B. Evaluation of sulphasalazine in the treatment of spondyloarthropathies. Ann Rheum Dis. 1992 Aug;51(8):955–958. doi: 10.1136/ard.51.8.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougados M., vam der Linden S., Leirisalo-Repo M., Huitfeldt B., Juhlin R., Veys E., Zeidler H., Kvien T. K., Olivieri I., Dijkmans B. Sulfasalazine in the treatment of spondylarthropathy. A randomized, multicenter, double-blind, placebo-controlled study. Arthritis Rheum. 1995 May;38(5):618–627. doi: 10.1002/art.1780380507. [DOI] [PubMed] [Google Scholar]
- Dougados M., van der Linden S., Juhlin R., Huitfeldt B., Amor B., Calin A., Cats A., Dijkmans B., Olivieri I., Pasero G. The European Spondylarthropathy Study Group preliminary criteria for the classification of spondylarthropathy. Arthritis Rheum. 1991 Oct;34(10):1218–1227. doi: 10.1002/art.1780341003. [DOI] [PubMed] [Google Scholar]
- McConkey B., Amos R. S., Durham S., Forster P. J., Hubball S., Walsh L. Sulphasalazine in rheumatoid arthritis. Br Med J. 1980 Feb 16;280(6212):442–444. doi: 10.1136/bmj.280.6212.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielants H., Veys E. M., Cuvelier C., De Vos M., Botelberghe L. HLA-B27 related arthritis and bowel inflammation. Part 2. Ileocolonoscopy and bowel histology in patients with HLA-B27 related arthritis. J Rheumatol. 1985 Apr;12(2):294–298. [PubMed] [Google Scholar]
- Mielants H., Veys E. M., Goemaere S., Goethals K., Cuvelier C., De Vos M. Gut inflammation in the spondyloarthropathies: clinical, radiologic, biologic and genetic features in relation to the type of histology. A prospective study. J Rheumatol. 1991 Oct;18(10):1542–1551. [PubMed] [Google Scholar]
- Mielants H., Veys E. M. HLA-B27 related arthritis and bowel inflammation. Part 1. Sulfasalazine (salazopyrin) in HLA-B27 related reactive arthritis. J Rheumatol. 1985 Apr;12(2):287–293. [PubMed] [Google Scholar]
- Mielants H., Veys E. M., Joos R., Cuvelier C., De Vos M. Repeat ileocolonoscopy in reactive arthritis. J Rheumatol. 1987 Jun;14(3):456–458. [PubMed] [Google Scholar]
- Mielants H., Veys E. M., Joos R. Sulphasalazine (Salazopyrin) in the treatment of enterogenic reactive synovitis and ankylosing spondylitis with peripheral arthritis. Clin Rheumatol. 1986 Jan;5(1):80–83. doi: 10.1007/BF02030973. [DOI] [PubMed] [Google Scholar]
- Peppercorn M. A. Sulfasalazine. Pharmacology, clinical use, toxicity, and related new drug development. Ann Intern Med. 1984 Sep;101(3):377–386. doi: 10.7326/0003-4819-101-3-377. [DOI] [PubMed] [Google Scholar]
- Pullar T., Capell H. A. Sulphasalazine: a 'new' antirheumatic drug. Br J Rheumatol. 1984 Feb;23(1):26–34. doi: 10.1093/rheumatology/23.1.26. [DOI] [PubMed] [Google Scholar]
- Stroehmann I., Wüstenhagen E., Martini M. Die Therapie seronegativer Oligoarthritiden mit Salazopyrin. Z Rheumatol. 1987 Mar-Apr;46(2):79–82. [PubMed] [Google Scholar]
- Willkens R. F., Arnett F. C., Bitter T., Calin A., Fisher L., Ford D. K., Good A. E., Masi A. T. Reiter's syndrome. Evaluation of preliminary criteria for definite disease. Arthritis Rheum. 1981 Jun;24(6):844–849. doi: 10.1002/art.1780240612. [DOI] [PubMed] [Google Scholar]



