Abstract
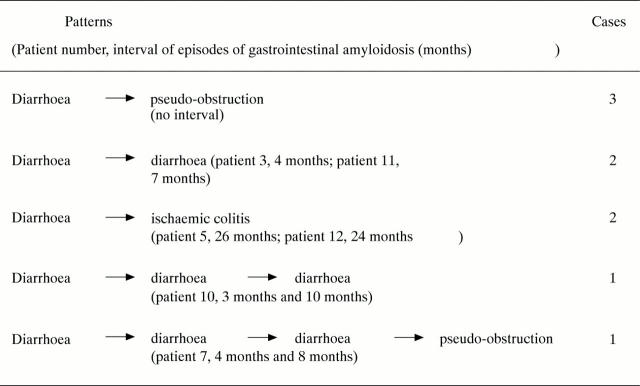
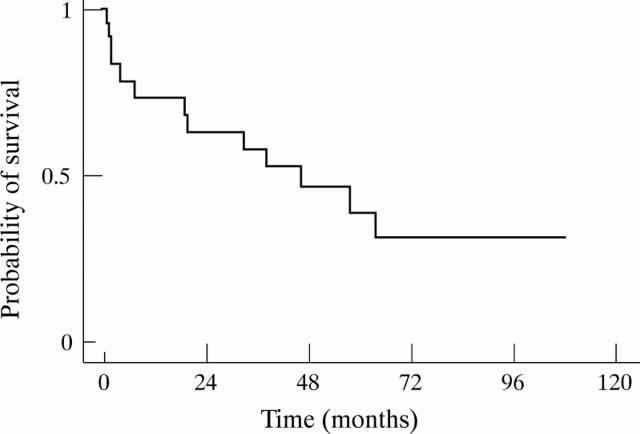
OBJECTIVE—To examine the clinical characteristics of intractable diarrhoea associated with secondary amyloidosis in rheumatoid arthritis (RA). METHODS—Of 179 RA patients with biopsy confirmed secondary amyloidosis, 24 cases (23 women and one man) with intractable diarrhoea lasting for more than one month were retrospectively evaluated. RESULTS—The mean (SD) duration of diarrhoea was 87 (64) days. Prodromal symptoms of gastrointestinal dysfunction (n = 21) and impaired peristalsis (n = 16) were observed. Laboratory data showed hypoproteinaemia (4.7 (0.85) g/dl) caused by malabsorption or protein loss and high values of C reactive protein (17.0 (9.3) mg/dl). Recurrence of intractable diarrhoea (n = 4) and transition from intractable diarrhoea to other gastrointestinal problems of amyloidosis (ischaemic colitis (n = 2) and intestinal pseudo-obstruction (n = 4)) were observed. In 19 patients (25 episodes) the duration of intravenous hyperalimentation at remission (18 episodes) was 68 (52) days. Corticosteroid pulse therapy was administered to 10 patients (11 times) and the time elapsed from the end of corticosteroid pulse therapy to the end of diarrhoea was 18 (14) days. One and five year survival rates after the onset of intractable diarrhoea were 73.4% and 38.9% . Seven of 13 patients (54%) had died as a result of infectious diseases. CONCLUSION—Intractable diarrhoea associated with secondary amyloidosis in RA is a serious clinical entity and the prognosis is poor. Although it is assumed that intravenous hyperalimentation treatment and corticosteroid pulse therapy are favourable regimens for intractable diarrhoea, the patients should be monitored for possible infectious complications.
Full Text
The Full Text of this article is available as a PDF (143.9 KB).
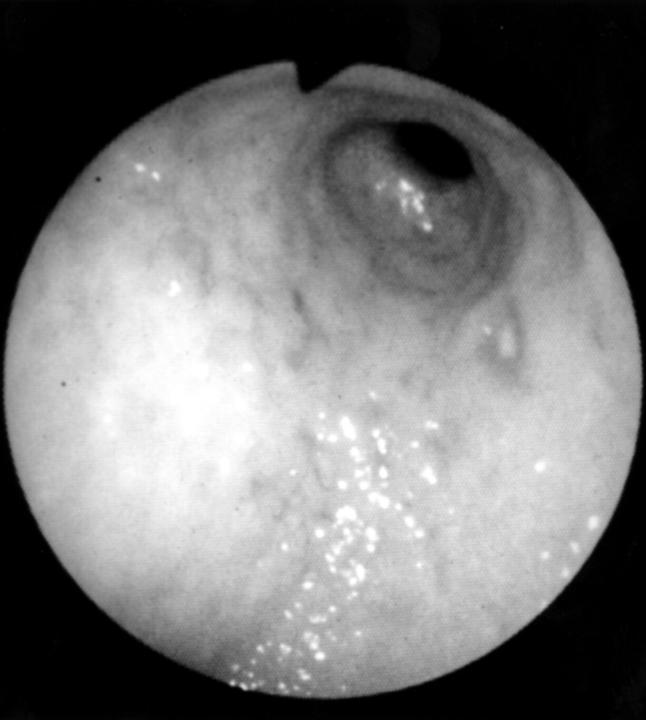
Figure 1 .
Multiple erosions, redness, and coarse irregular elevated mucosa are seen in the antrum of the stomach.
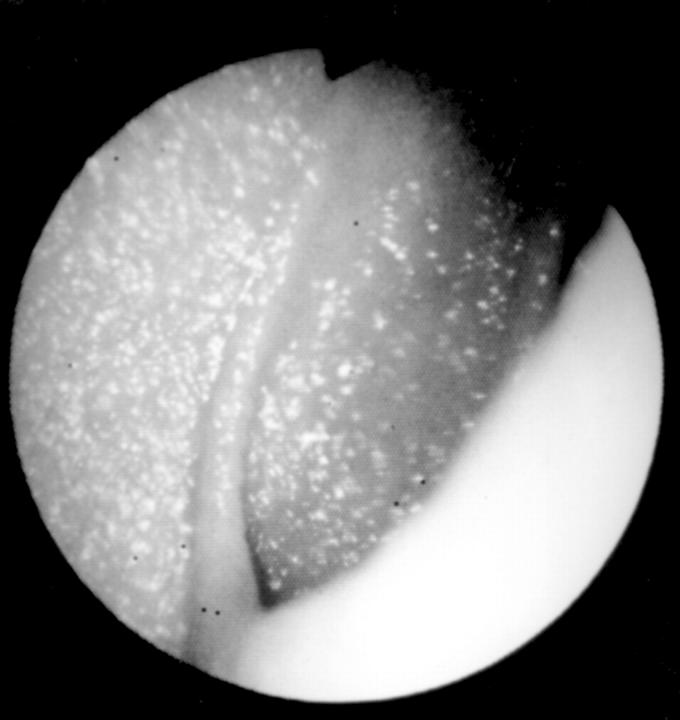
Figure 2 .
Endoscopy shows fine granular elevations in the second portion of the duodenum.
Figure 3 .
Patterns of relapse of intractable diarrhoea and transition from intractable diarrhoea to other types of gastrointestinal manifestations of amyloidosis (ischaemic colitis or intestinal pseudo-obstruction ).
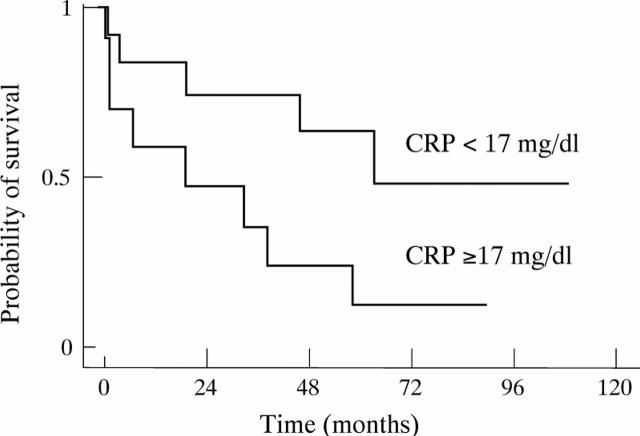
Figure 4 .
Survival rate of the 24 rheumatoid arthritis patients with intractable diarrhoea associated with secondary amyloidosis.
Figure 5 .
Survival of the 24 rheumatoid arthritis patients with intractable diarrhoea associated with secondary amyloidosis, according to C reactive protein (CRP) ≥17 mg/dl or CRP <17 mg/dl.
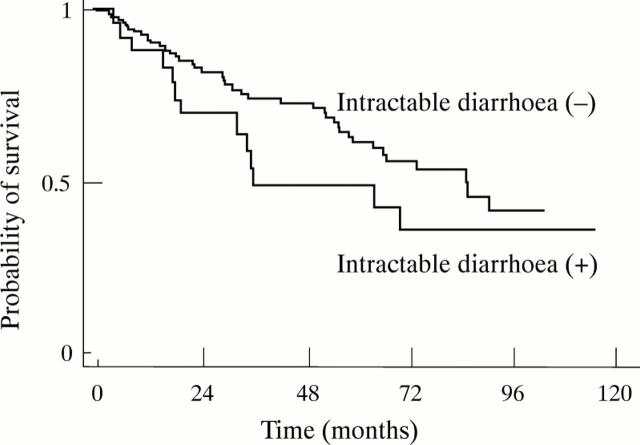
Figure 6 .
Survival of 179 patients with rheumatoid arthritis associated with secondary amyloidosis, according to the presence or absence of intractable diarrhoea.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arnett F. C., Edworthy S. M., Bloch D. A., McShane D. J., Fries J. F., Cooper N. S., Healey L. A., Kaplan S. R., Liang M. H., Luthra H. S. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988 Mar;31(3):315–324. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- Battle W. M., Rubin M. R., Cohen S., Snape W. J., Jr Gastrointestinal-motility dysfunction in amyloidosis. N Engl J Med. 1979 Jul 5;301(1):24–25. doi: 10.1056/NEJM197907053010105. [DOI] [PubMed] [Google Scholar]
- Browning M. J., Banks R. A., Tribe C. R., Hollingworth P., Kingswood C., Mackenzie J. C., Bacon P. A. Ten years' experience of an amyloid clinic--a clinicopathological survey. Q J Med. 1985 Mar;54(215):213–227. [PubMed] [Google Scholar]
- Falck H. M., Maury C. P., Teppo A. M., Wegelius O. Correlation of persistently high serum amyloid A protein and C-reactive protein concentrations with rapid progression of secondary amyloidosis. Br Med J (Clin Res Ed) 1983 Apr 30;286(6375):1391–1393. doi: 10.1136/bmj.286.6375.1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friman C., Pettersson T. Amyloidosis. Curr Opin Rheumatol. 1996 Jan;8(1):62–71. doi: 10.1097/00002281-199601000-00012. [DOI] [PubMed] [Google Scholar]
- Gertz M. A., Kyle R. A. Secondary systemic amyloidosis: response and survival in 64 patients. Medicine (Baltimore) 1991 Jul;70(4):246–256. [PubMed] [Google Scholar]
- Gilat T., Spiro H. M. Amyloidosis and the gut. Am J Dig Dis. 1968 Jul;13(7):619–633. doi: 10.1007/BF02232969. [DOI] [PubMed] [Google Scholar]
- Glenner G. G. Amyloid deposits and amyloidosis. The beta-fibrilloses (first of two parts). N Engl J Med. 1980 Jun 5;302(23):1283–1292. doi: 10.1056/NEJM198006053022305. [DOI] [PubMed] [Google Scholar]
- Hashimoto M., Shingu M., Yoshikawa Y., Nonaka S., Wada T., Ichibanngase Y., Nobunaga M. [Amyloidosis of the small intestine secondary to rheumatoid arthritis and juvenile rheumatoid arthritis: report of two cases]. Ryumachi. 1995 Feb;35(1):100–106. [PubMed] [Google Scholar]
- Hazenberg B. P., van Rijswijk M. H. Clinical and therapeutic aspects of AA amyloidosis. Baillieres Clin Rheumatol. 1994 Aug;8(3):661–690. doi: 10.1016/s0950-3579(05)80121-9. [DOI] [PubMed] [Google Scholar]
- Husby G. Amyloidosis and rheumatoid arthritis. Clin Exp Rheumatol. 1985 Apr-Jun;3(2):173–180. [PubMed] [Google Scholar]
- Ishikawa Y., Ishii T., Masuda S., Asuwa N., Kiguchi H. Multiple penetrating colonic ulcers in secondary amyloidosis caused by rheumatoid arthritis. Acta Pathol Jpn. 1993 Jan-Feb;43(1-2):59–64. doi: 10.1111/j.1440-1827.1993.tb02915.x. [DOI] [PubMed] [Google Scholar]
- Janssen S., Van Rijswijk M. H., Meijer S., Ruinen L., Van der Hem G. K. Systemic amyloidosis: a clinical survey of 144 cases. Neth J Med. 1986;29(11):376–385. [PubMed] [Google Scholar]
- Kawaguchi M., Koizumi F., Shimao M., Hirose S. Protein-losing enteropathy due to secondary amyloidosis of the gastrointestinal tract. Acta Pathol Jpn. 1993 Jun;43(6):333–339. doi: 10.1111/j.1440-1827.1993.tb02576.x. [DOI] [PubMed] [Google Scholar]
- Kobayashi H., Tada S., Fuchigami T., Okuda Y., Takasugi K., Matsumoto T., Iida M., Aoyagi K., Iwashita A., Daimaru Y. Secondary amyloidosis in patients with rheumatoid arthritis: diagnostic and prognostic value of gastroduodenal biopsy. Br J Rheumatol. 1996 Jan;35(1):44–49. doi: 10.1093/rheumatology/35.1.44. [DOI] [PubMed] [Google Scholar]
- Lansbury J. Clinical appraisal of the activity index as a measure of rheumatoid activity. Arthritis Rheum. 1968 Aug;11(4):599–604. doi: 10.1002/art.1780110411. [DOI] [PubMed] [Google Scholar]
- Legge D. A., Wollaeger E. E., Carlson H. C. Intestinal pseudo-obstruction in systemic amyloidosis. Gut. 1970 Sep;11(9):764–767. doi: 10.1136/gut.11.9.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuda Y., Takasugi K., Oyama T., Onuma M., Oyama H. [Amyloidosis in rheumatoid arthritis--clinical study of 124 histologically proven cases]. Ryumachi. 1994 Dec;34(6):939–946. [PubMed] [Google Scholar]
- Pettersson T., Wegelius O. Biopsy diagnosis of amyloidosis in rheumatoid arthritis. Malabsorption caused by intestinal amyloid deposits. Gastroenterology. 1972 Jan;62(1):22–27. [PubMed] [Google Scholar]
- Tada S., Iida M., Iwashita A., Matsui T., Fuchigami T., Yamamoto T., Yao T., Fujishima M. Endoscopic and biopsy findings of the upper digestive tract in patients with amyloidosis. Gastrointest Endosc. 1990 Jan-Feb;36(1):10–14. doi: 10.1016/s0016-5107(90)70913-3. [DOI] [PubMed] [Google Scholar]
- Tiitinen S., Kaarela K., Helin H., Kautiainen H., Isomäki H. Amyloidosis--incidence and early risk factors in patients with rheumatoid arthritis. Scand J Rheumatol. 1993;22(4):158–161. doi: 10.3109/03009749309099264. [DOI] [PubMed] [Google Scholar]