Abstract
OBJECTIVE—To determine the clinical characteristics of patients with "pure" remitting seronegative symmetrical synovitis with pitting oedema (RS3PE) syndrome, and to investigate its relation with polymyalgia rheumatica (PMR). Magnetic resonance imaging (MRI) was used to describe the anatomical structures affected by inflammation in pure RS3PE syndrome. METHODS—A prospective follow up study of 23 consecutive patients with pure RS3PE syndrome and 177 consecutive patients with PMR diagnosed over a five year period in two Italian secondary referral centres of rheumatology. Hands or feet MRI, or both, was performed at diagnosis in 7 of 23 patients. RESULTS—At inspection evidence of hand and/or foot tenosynovitis was present in all the 23 patients with pure RS3PE syndrome. Twenty one (12%) patients with PMR associated distal extremity swelling with pitting oedema. No significant differences in the sex, age at onset of disease, acute phase reactant values at diagnosis, frequency of peripheral synovitis and carpal tunnel syndrome and frequency of HLA-B7 antigen were present between patients with pure RS3PE and PMR. In both conditions no patient under 50 was observed, the disease frequency increased significantly with age and the highest frequency was present in the age group 70-79 years. Clinical symptoms for both conditions responded promptly to corticosteroids and no patient developed rheumatoid arthritis during the follow up. However, the patients with pure RS3PE syndrome were characterised by shorter duration of treatment, lower cumulative corticosteroid dose and lower frequency of systemic signs/symptoms and relapse/recurrence. Hands and feet MRI showed evidence of tenosynovitis in five patients and joint synovitis in three patients. CONCLUSION—The similarities of demographic, clinical, and MRI findings between RS3PE syndrome and PMR and the concurrence of the two syndromes suggest that these conditions may be part of the same disease and that the diagnostic labels of PMR and RS3PE syndrome may not indicate a real difference. The presence of distal oedema seems to indicate a better prognosis. Keywords: RS3PE; polymyalgia rheumatica; pitting oedema; magnetic resonance imaging
Full Text
The Full Text of this article is available as a PDF (206.0 KB).
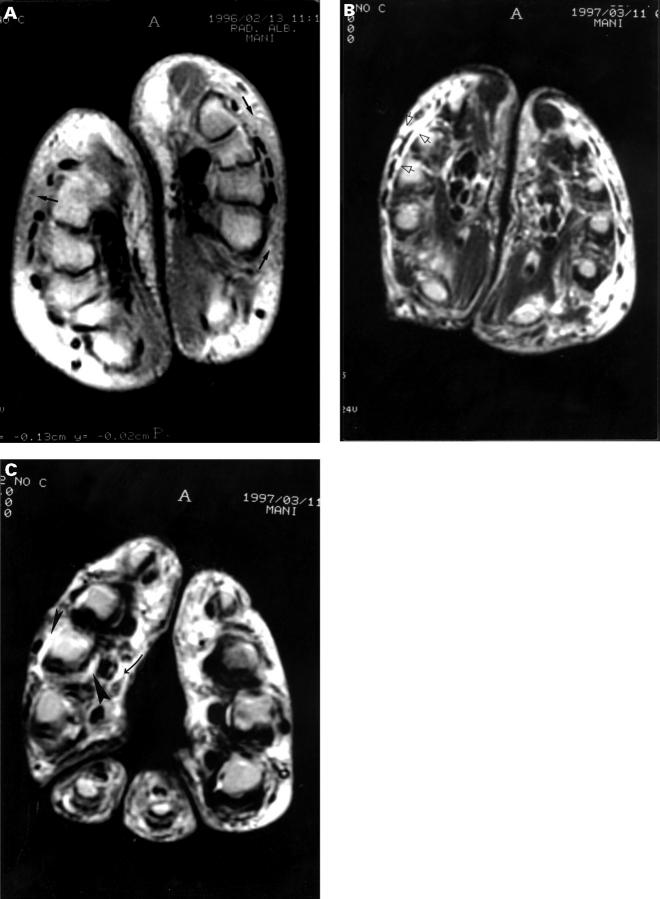
Figure 1 .
MRI of the hands of RS3PE syndrome. (A) Axial proton density section through the midpoint of the palm shows subcutaneous oedema in hand dorsum (black arrows). (B) Axial T2 weighted section through the midpoint of the palm shows fluid collection in the extensor synovial sheaths of the right hand (open arrows). (C) Axial T2 weighted section through the metacarpophalangeal joints shows fluid collection in the flexor synovial sheaths of the third digit of right hand (curved arrow) and joint effusion of the corresponding joint (large and small arrowheads).
Figure 2 .
MRI of the foot of RS3PE syndrome. (A) Sagittal T1 weighted section shows marked tenosynovitis of tibialis anterior tendon (black arrow). (B) Sagittal T2 weighted section shows marked tenosynovitis of tibialis anterior tendon (black arrow), ankle joint effusion extending into Kager's triangle (black/white arrow) and talonavicular joint effusion (black/white arrow). (C) Coronal T2 weighted section at the apex of the talus shows talonavicular joint effusion (black/white arrow), tenosynovitis of flexor hallucis longus tendon (double open arrowhead), tenosynovitis of flexor digitorum longus tendon (open arrowhead), tenosynovitis of tibialis posterior tendon (open white arrow) and tenosynovitis of peroneal tendons (black arrowhead). (D) Coronal T2 weighted section through the navicular bone shows marked tenosynovitis of tibialis anterior tendon (black arrow).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arnett F. C., Edworthy S. M., Bloch D. A., McShane D. J., Fries J. F., Cooper N. S., Healey L. A., Kaplan S. R., Liang M. H., Luthra H. S. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988 Mar;31(3):315–324. doi: 10.1002/art.1780310302. [DOI] [PubMed] [Google Scholar]
- Bhakta B. B., Pease C. T. Late-onset rheumatoid arthritis: is pitting oedema of the hands at onset a good prognostic indicator? Br J Rheumatol. 1997 Feb;36(2):214–219. doi: 10.1093/rheumatology/36.2.214. [DOI] [PubMed] [Google Scholar]
- Cantini F., Niccoli L., Olivieri I., Barozzi L., Pavlica P., Bozza A., Macchioni P. L., Padula A. A., Salvarani C. Remitting distal lower extremity swelling with pitting oedema in acute sarcoidosis. Ann Rheum Dis. 1997 Sep;56(9):565–566. doi: 10.1136/ard.56.9.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantini F., Olivieri I., Salvarani C. More on remitting seronegative symmetrical synovitis with pitting edema as paraneoplastic syndrome. J Rheumatol. 1998 Jan;25(1):188–189. [PubMed] [Google Scholar]
- Dougados M., van der Linden S., Juhlin R., Huitfeldt B., Amor B., Calin A., Cats A., Dijkmans B., Olivieri I., Pasero G. The European Spondylarthropathy Study Group preliminary criteria for the classification of spondylarthropathy. Arthritis Rheum. 1991 Oct;34(10):1218–1227. doi: 10.1002/art.1780341003. [DOI] [PubMed] [Google Scholar]
- Healey L. A. Long-term follow-up of polymyalgia rheumatica: evidence for synovitis. Semin Arthritis Rheum. 1984 May;13(4):322–328. doi: 10.1016/0049-0172(84)90012-x. [DOI] [PubMed] [Google Scholar]
- McCarty D. J., O'Duffy J. D., Pearson L., Hunter J. B. Remitting seronegative symmetrical synovitis with pitting edema. RS3PE syndrome. JAMA. 1985 Nov 15;254(19):2763–2767. [PubMed] [Google Scholar]
- Olivieri I., Padula A., Favaro L., Oranges G. S., Ferri S. RS3PE syndrome with unilateral involvement. J Rheumatol. 1994 Feb;21(2):372–372. [PubMed] [Google Scholar]
- Olivieri I., Padula A., Favaro L., Pierro A., Oranges G. S., Ferri S. Dactylitis with pitting oedema of the hand in longstanding ankylosing spondylitis. Clin Rheumatol. 1995 Nov;14(6):701–704. doi: 10.1007/BF02207940. [DOI] [PubMed] [Google Scholar]
- Olivieri I., Padula A., Pierro A., Favaro L., Oranges G. S., Ferri S. Late onset undifferentiated seronegative spondyloarthropathy. J Rheumatol. 1995 May;22(5):899–903. [PubMed] [Google Scholar]
- Olivieri I., Salvarani C., Cantini F., Barozzi L., Macchioni L., Pavlica P. Distal extremity swelling with pitting edema in polymyalgia rheumatica: a case studied with MRI. Clin Exp Rheumatol. 1997 Nov-Dec;15(6):710–711. [PubMed] [Google Scholar]
- Olivieri I., Salvarani C., Cantini F. Remitting distal extremity swelling with pitting edema: a distinct syndrome or a clinical feature of different inflammatory rheumatic diseases? J Rheumatol. 1997 Feb;24(2):249–252. [PubMed] [Google Scholar]
- Olivo D., Mattace R. Concurrence of benign edematous polysynovitis in the elderly (RS3PE syndrome) and endometrial adenocarcinoma. Scand J Rheumatol. 1997;26(1):67–68. doi: 10.3109/03009749709065669. [DOI] [PubMed] [Google Scholar]
- Pariser K. M., Canoso J. J. Remitting, seronegative (A) symmetrical synovitis with pitting edema--two cases of RS3PE syndrome. J Rheumatol. 1991 Aug;18(8):1260–1262. [PubMed] [Google Scholar]
- Russell E. B., Hunter J. B., Pearson L., McCarty D. J. Remitting, seronegative, symmetrical synovitis with pitting edema--13 additional cases. J Rheumatol. 1990 May;17(5):633–639. [PubMed] [Google Scholar]
- Salvarani C., Cantini F., Macchioni P., Olivieri I., Niccoli L., Padula A., Boiardi L. Distal musculoskeletal manifestations in polymyalgia rheumatica: a prospective followup study. Arthritis Rheum. 1998 Jul;41(7):1221–1226. doi: 10.1002/1529-0131(199807)41:7<1221::AID-ART12>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- Salvarani C., Cantini F., Olivieri I., Barozzi L., Macchioni L., Niccoli L., Padula A., De Matteis M., Pavlica P. Proximal bursitis in active polymyalgia rheumatica. Ann Intern Med. 1997 Jul 1;127(1):27–31. doi: 10.7326/0003-4819-127-1-199707010-00005. [DOI] [PubMed] [Google Scholar]
- Salvarani C., Gabriel S., Hunder G. G. Distal extremity swelling with pitting edema in polymyalgia rheumatica. Report on nineteen cases. Arthritis Rheum. 1996 Jan;39(1):73–80. doi: 10.1002/art.1780390110. [DOI] [PubMed] [Google Scholar]
- Schaeverbeke T., Fatout E., Marcé S., Vernhes J. P., Hallé O., Antoine J. F., Lequen L., Bannwarth B., Dehais J. Remitting seronegative symmetrical synovitis with pitting oedema: disease or syndrome? Ann Rheum Dis. 1995 Aug;54(8):681–684. doi: 10.1136/ard.54.8.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TERASAKI P. I., MCCLELLAND J. D. MICRODROPLET ASSAY OF HUMAN SERUM CYTOTOXINS. Nature. 1964 Dec 5;204:998–1000. doi: 10.1038/204998b0. [DOI] [PubMed] [Google Scholar]
- Tada Y., Sato H., Yoshizawa S., Kimura H., Kitamura M., Kusaba T., Nagasawa K. Remitting seronegative symmetrical synovitis with pitting edema associated with gastric carcinoma. J Rheumatol. 1997 May;24(5):974–975. [PubMed] [Google Scholar]