Abstract
OBJECTIVE—To assess the cost effectiveness of antibiotic prophylaxis for haematogenous bacterial arthritis in patients with joint disease. METHODS—In a decision analysis, data from a prospective study on bacterial arthritis in 4907 patients with joint disease were combined with literature data to assess risks and benefits of antibiotic prophylaxis. Effectiveness and cost effectiveness calculations were performed on antibiotic prophylaxis for various patient groups. Grouping was based on (a) type of event leading to transient bacteraemia—that is, infections (dermal, respiratory/urinary tract) and invasive medical procedures—and (b) the patient's susceptibility to bacterial arthritis which was increased in the presence of rheumatoid arthritis, large joint prostheses, comorbidity, and old age. RESULTS—Of the patients with joint disease, 59% had no characteristics that increased susceptibility to bacterial arthritis, and 31% had one. For dermal infections, the effectiveness of antibiotic prophylaxis was maximally 35 quality adjusted life days (QALDs) and the cost effectiveness maximally $52 000 per quality adjusted life year (QALY). For other infections, the effectiveness of prophylaxis was lower and the cost effectiveness higher. Prophylaxis for invasive medical procedures seemed to be acceptable only in patients with high susceptibility: 1 QALD at a cost of $1300/QALY; however, the results were influenced substantially when the level of efficacy of the prophylaxis or cost of prophylactic antibiotics was changed. CONCLUSION—Prophylaxis seems to be indicated only for dermal infections, and for infections of the urinary and respiratory tract in patients with increased susceptibility to bacterial arthritis. Prophylaxis for invasive medical procedures, such as dental treatment, may only be indicated for patients with joint disease who are highly susceptible.
Full Text
The Full Text of this article is available as a PDF (109.5 KB).
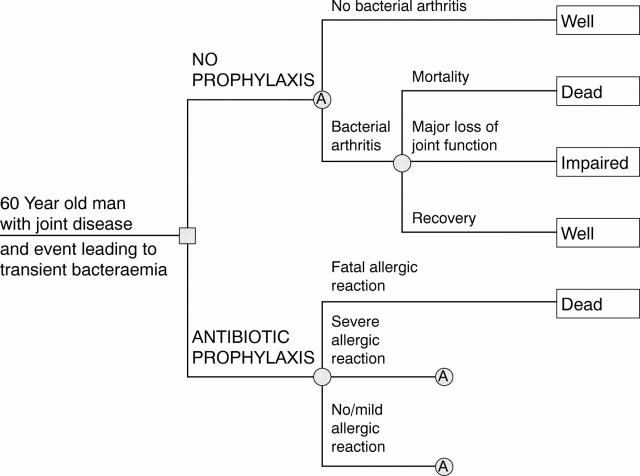
Figure 1 .
Decision tree for prophylactic management with antibiotics of a 60 year old man with joint disease who is confronted with an event leading to transient bacteraemia. The chronological order of events is from left to right. The decision node is represented by a square, chance nodes by circles, and health outcomes are indicated by rectangles. Subtree A is to be inserted in the two lower branches. Quantification of these subtrees differs.
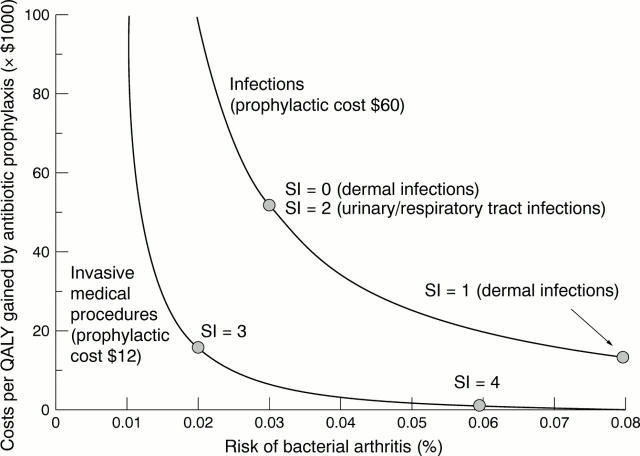
Figure 2 .
Sensitivity analysis: cost per quality adjusted life year (QALY) gained by antibiotic prophylaxis as a function of the risk of bacterial arthritis for infections (prophylactic cost $60) and invasive medical procedures (prophylactic cost $12). For some of the risk situations presented in table 4, the risk of bacterial arthritis lies within the depicted range. These risk situations are represented as dots. For example, the risk of bacterial arthritis for patients with low susceptibility to bacterial arthritis (SI = 0) was 0.03% in the case of dermal infection (see table 4). For this risk situation, antibiotic prophylaxis costs $52 000 per QALY gained by prophylaxis (see table 5).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahlberg A., Carlsson A. S., Lindberg L. Hematogenous infection in total joint replacement. Clin Orthop Relat Res. 1978 Nov-Dec;(137):69–75. [PubMed] [Google Scholar]
- Averns H. L., Kerry R. Role of prophylactic antibiotics in the prevention of late infection of prosthetic joints. Results of a questionnaire and review of the literature. Br J Rheumatol. 1995 Apr;34(4):380–382. doi: 10.1093/rheumatology/34.4.380. [DOI] [PubMed] [Google Scholar]
- BATSON J. M. Anaphylactoid reactions to oral administration of penicillin. N Engl J Med. 1960 Mar 24;262:590–595. doi: 10.1056/NEJM196003242621202. [DOI] [PubMed] [Google Scholar]
- Blackburn W. D., Jr, Alarcón G. S. Prosthetic joint infections. A role for prophylaxis. Arthritis Rheum. 1991 Jan;34(1):110–117. doi: 10.1002/art.1780340118. [DOI] [PubMed] [Google Scholar]
- Bor D. H., Himmelstein D. U. Endocarditis prophylaxis for patients with mitral valve prolapse. A quantitative analysis. Am J Med. 1984 Apr;76(4):711–717. doi: 10.1016/0002-9343(84)90300-0. [DOI] [PubMed] [Google Scholar]
- Cawson R. A. Antibiotic prophylaxis for dental treatment. BMJ. 1992 Apr 11;304(6832):933–934. doi: 10.1136/bmj.304.6832.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cioffi G. A., Terezhalmy G. T., Taybos G. M. Total joint replacement: a consideration for antimicrobial prophylaxis. Oral Surg Oral Med Oral Pathol. 1988 Jul;66(1):124–129. doi: 10.1016/0030-4220(88)90079-5. [DOI] [PubMed] [Google Scholar]
- Clemens J. D., Ransohoff D. F. A quantitative assessment of pre-dental antibiotic prophylaxis for patients with mitral-valve prolapse. J Chronic Dis. 1984;37(7):531–544. doi: 10.1016/0021-9681(84)90004-3. [DOI] [PubMed] [Google Scholar]
- Erffmeyer J. E. Adverse reactions to penicillin. Part I. Ann Allergy. 1981 Oct;47(4):288–293. [PubMed] [Google Scholar]
- Essink-Bot M. L., Bonsel G. J., van der Maas P. J. Valuation of health states by the general public: feasibility of a standardized measurement procedure. Soc Sci Med. 1990;31(11):1201–1206. doi: 10.1016/0277-9536(90)90124-b. [DOI] [PubMed] [Google Scholar]
- Fitzgerald R. H., Jr, Nolan D. R., Ilstrup D. M., Van Scoy R. E., Washington J. A., 2nd, Coventry M. B. Deep wound sepsis following total hip arthroplasty. J Bone Joint Surg Am. 1977 Oct;59(7):847–855. [PubMed] [Google Scholar]
- Goldenberg D. L. Infectious arthritis complicating rheumatoid arthritis and other chronic rheumatic disorders. Arthritis Rheum. 1989 Apr;32(4):496–502. doi: 10.1002/anr.1780320422. [DOI] [PubMed] [Google Scholar]
- Grant A., Hoddinott C. Joint replacement, dental surgery, and antibiotic prophylaxis. BMJ. 1992 Apr 11;304(6832):959–959. doi: 10.1136/bmj.304.6832.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grogan T. J., Dorey F., Rollins J., Amstutz H. C. Deep sepsis following total knee arthroplasty. Ten-year experience at the University of California at Los Angeles Medical Center. J Bone Joint Surg Am. 1986 Feb;68(2):226–234. [PubMed] [Google Scholar]
- Ho G., Jr Bacterial arthritis. Curr Opin Rheumatol. 1991 Aug;3(4):603–609. doi: 10.1097/00002281-199108000-00009. [DOI] [PubMed] [Google Scholar]
- Ho G., Jr Bacterial arthritis. Curr Opin Rheumatol. 1993 Jul;5(4):449–453. doi: 10.1097/00002281-199305040-00008. [DOI] [PubMed] [Google Scholar]
- Idsoe O., Guthe T., Willcox R. R., de Weck A. L. Nature and extent of penicillin side-reactions, with particular reference to fatalities from anaphylactic shock. Bull World Health Organ. 1968;38(2):159–188. [PMC free article] [PubMed] [Google Scholar]
- Imperiale T. F., Horwitz R. I. Does prophylaxis prevent postdental infective endocarditis? A controlled evaluation of protective efficacy. Am J Med. 1990 Feb;88(2):131–136. doi: 10.1016/0002-9343(90)90461-l. [DOI] [PubMed] [Google Scholar]
- Jacobson J. J., Schweitzer S., DePorter D. J., Lee J. J. Antibiotic prophylaxis for dental patients with joint prostheses? A decision analysis. Int J Technol Assess Health Care. 1990;6(4):569–587. doi: 10.1017/s0266462300004220. [DOI] [PubMed] [Google Scholar]
- Kaandorp C. J., Dinant H. J., van de Laar M. A., Moens H. J., Prins A. P., Dijkmans B. A. Incidence and sources of native and prosthetic joint infection: a community based prospective survey. Ann Rheum Dis. 1997 Aug;56(8):470–475. doi: 10.1136/ard.56.8.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaandorp C. J., Krijnen P., Moens H. J., Habbema J. D., van Schaardenburg D. The outcome of bacterial arthritis: a prospective community-based study. Arthritis Rheum. 1997 May;40(5):884–892. doi: 10.1002/art.1780400516. [DOI] [PubMed] [Google Scholar]
- Kaandorp C. J., Van Schaardenburg D., Krijnen P., Habbema J. D., van de Laar M. A. Risk factors for septic arthritis in patients with joint disease. A prospective study. Arthritis Rheum. 1995 Dec;38(12):1819–1825. doi: 10.1002/art.1780381215. [DOI] [PubMed] [Google Scholar]
- Koopmanschap M. A., Lubbe K. T., van Oortmarssen G. J., van Agt H. M., van Ballegooijen M., Habbema J. K. Economic aspects of cervical cancer screening. Soc Sci Med. 1990;30(10):1081–1087. doi: 10.1016/0277-9536(90)90294-3. [DOI] [PubMed] [Google Scholar]
- Lattimer G. L., Keblish P. A., Dickson T. B., Jr, Vernick C. G., Finnegan W. J. Hematogenous infection in total joint replacement. Recommendations for prophylactic antibiotics. JAMA. 1979 Nov 16;242(20):2213–2214. [PubMed] [Google Scholar]
- Meijers K. A., Dijkmans B. A., Hermans J., van den Broek P. J., Cats A. Non-gonococcal infectious arthritis: a retrospective study. J Infect. 1987 Jan;14(1):13–20. doi: 10.1016/s0163-4453(87)90704-3. [DOI] [PubMed] [Google Scholar]
- Neu H. C., Wilson A. P., Grüneberg R. N. Amoxycillin/clavulanic acid: a review of its efficacy in over 38,500 patients from 1979 to 1992. J Chemother. 1993 Apr;5(2):67–93. doi: 10.1080/1120009x.1993.11739213. [DOI] [PubMed] [Google Scholar]
- Newman J. H. Review of septic arthritis throughout the antibiotic era. Ann Rheum Dis. 1976 Jun;35(3):198–205. doi: 10.1136/ard.35.3.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norden C. W. Antibiotic prophylaxis in orthopedic surgery. Rev Infect Dis. 1991 Sep-Oct;13 (Suppl 10):S842–S846. doi: 10.1093/clinids/13.supplement_10.s842. [DOI] [PubMed] [Google Scholar]
- Norden C. W. Prevention of bone and joint infections. Am J Med. 1985 Jun 28;78(6B):229–232. doi: 10.1016/0002-9343(85)90390-0. [DOI] [PubMed] [Google Scholar]
- Norfleet R. G. Infective endocarditis and infections of orthopedic and vascular prostheses following gastrointestinal endoscopy and dilation. Gastrointest Endosc. 1990 Sep-Oct;36(5):546–547. doi: 10.1016/s0016-5107(90)71153-4. [DOI] [PubMed] [Google Scholar]
- Poss R., Thornhill T. S., Ewald F. C., Thomas W. H., Batte N. J., Sledge C. B. Factors influencing the incidence and outcome of infection following total joint arthroplasty. Clin Orthop Relat Res. 1984 Jan-Feb;(182):117–126. [PubMed] [Google Scholar]
- Rudolph A. H., Price E. V. Penicillin reactions among patients in venereal disease clinics. A national survey. JAMA. 1973 Jan 29;223(5):499–501. [PubMed] [Google Scholar]
- Sørensen H. T., Nielsen B., Ostergaard Nielsen J. Anaphylactic shock occurring outside hospitals. Allergy. 1989 May;44(4):288–290. doi: 10.1111/j.1398-9995.1989.tb01071.x. [DOI] [PubMed] [Google Scholar]
- Thyne G. M., Ferguson J. W. Antibiotic prophylaxis during dental treatment in patients with prosthetic joints. J Bone Joint Surg Br. 1991 Mar;73(2):191–194. doi: 10.1302/0301-620X.73B2.2005136. [DOI] [PubMed] [Google Scholar]
- Tsevat J., Durand-Zaleski I., Pauker S. G. Cost-effectiveness of antibiotic prophylaxis for dental procedures in patients with artificial joints. Am J Public Health. 1989 Jun;79(6):739–743. doi: 10.2105/ajph.79.6.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L. P., Bradley J. D., Hugenberg S. T., Brandt K. D. Predictors of mortality in non-post-operative patients with septic arthritis. Scand J Rheumatol. 1992;21(3):142–144. doi: 10.3109/03009749209095087. [DOI] [PubMed] [Google Scholar]
- de Koning H. J., van Ineveld B. M., van Oortmarssen G. J., de Haes J. C., Collette H. J., Hendriks J. H., van der Maas P. J. Breast cancer screening and cost-effectiveness; policy alternatives, quality of life considerations and the possible impact of uncertain factors. Int J Cancer. 1991 Oct 21;49(4):531–537. doi: 10.1002/ijc.2910490410. [DOI] [PubMed] [Google Scholar]