Abstract
OBJECTIVE—To assist in the interpretation of the Stanford Health Assessment Questionnaire (HAQ) score changes for individual patients with rheumatoid arthritis (RA), by determining the minimum size of score change that can confidently be considered to reflect a significant change in disability from the patient's perspective. METHOD—HAQ score changes were calculated for 40 clinic patients with RA who had reported no change to health in general over two months. These were considered to reflect both inconsistencies in questionnaire completion and any true but minor changes not considered significant enough by the patients to represent a change to their health in general. HAQ score changes over one year were also calculated for 207 clinic patients with RA. RESULTS—The range within which 95% of score changes would be expected to lie in the absence of significant change was estimated as ±0.48 points (±2SD of the score changes) and 80% within ±0.31 points (±1.29SD). A χ2 test showed no significant association between an HAQ score increase of >0.31 over one year and decline in health related to arthritis reported by the patient over the same period. CONCLUSION—As a general guideline, an HAQ score needs to change by 0.48 points or more for 95% confidence that it reflects significant change (0.31 for 80% confidence). Although the value of HAQ as a group outcome measure is well established, this study questions the usefulness of monitoring individual HAQ scores in a clinical setting.
Full Text
The Full Text of this article is available as a PDF (87.6 KB).
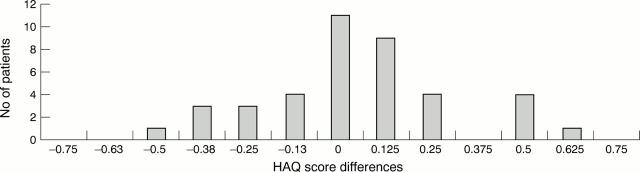
Figure 1 .
Health Assessment Questionnaire (HAQ) score differences over two months—40 patients with rheumatoid arthritis reporting no change in health in general.
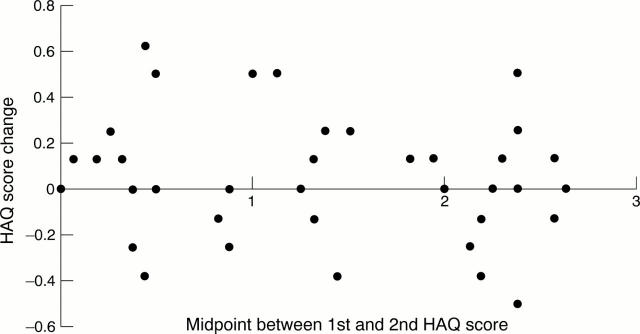
Figure 2 .
Size and direction of Health Assessment Questionnaire (HAQ) score change was not related to position on the scale. HAQ score changes over two months (with no patient perceived change in health in general) plotted against the midpoint between the two scores of each subject.
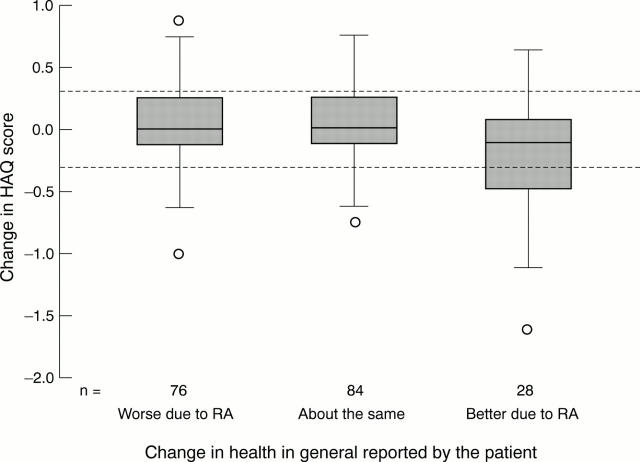
Figure 3 .
Box plots of annual Health Assessment Questionnaire (HAQ) score changes for patients with rheumatoid arthritis (RA) attending for routine outcome assessment (excluding 19 who reported change not related to their arthritis). The box plots show the median, the upper and lower quartiles (upper and lower edges of the box), the range excluding outliers (whiskers), and outliers (small circles). The dashed lines indicate the calculated limits within which 80% of differences would be expected to lie based on the score changes over two months for no patient perceived change in health in general.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bland J. M., Altman D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- Carr A. J. Margaret Holroyd Prize Essay. A patient-centred approach to evaluation and treatment in rheumatoid arthritis: the development of a clinical tool to measure patient-perceived handicap. Br J Rheumatol. 1996 Oct;35(10):921–932. doi: 10.1093/rheumatology/35.10.921. [DOI] [PubMed] [Google Scholar]
- Hawley D. J., Wolfe F. Sensitivity to change of the health assessment questionnaire (HAQ) and other clinical and health status measures in rheumatoid arthritis: results of short-term clinical trials and observational studies versus long-term observational studies. Arthritis Care Res. 1992 Sep;5(3):130–136. doi: 10.1002/art.1790050304. [DOI] [PubMed] [Google Scholar]
- Kazis L. E., Anderson J. J., Meenan R. F. Health status as a predictor of mortality in rheumatoid arthritis: a five-year study. J Rheumatol. 1990 May;17(5):609–613. [PubMed] [Google Scholar]
- Long A. F., Scott D. L. Measuring health status and outcomes in rheumatoid arthritis within routine clinical practice. Br J Rheumatol. 1994 Jul;33(7):682–685. doi: 10.1093/rheumatology/33.7.682. [DOI] [PubMed] [Google Scholar]
- Pincus T. Documenting quality management in rheumatic disease: are patient questionnaires the best (and only) method? Arthritis Care Res. 1996 Oct;9(5):339–348. doi: 10.1002/1529-0131(199610)9:5<339::aid-anr1790090502>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Ruta D. A., Garratt A. M., Leng M., Russell I. T., MacDonald L. M. A new approach to the measurement of quality of life. The Patient-Generated Index. Med Care. 1994 Nov;32(11):1109–1126. doi: 10.1097/00005650-199411000-00004. [DOI] [PubMed] [Google Scholar]
- Till S. H., Amos R. S. Neurofibromatosis masquerading as monoarticular juvenile arthritis. Br J Rheumatol. 1997 Feb;36(2):286–288. doi: 10.1093/rheumatology/36.2.286. [DOI] [PubMed] [Google Scholar]
- Wiles N., Barrett J., Barrett E., Silman A., Symmons D. Disability in patients with early inflammatory polyarthritis cannot be "tracked" from year to year: an examination of the hypothesis underlying percentile reference charts. J Rheumatol. 1999 Apr;26(4):800–804. [PubMed] [Google Scholar]