Abstract
Objectives: To assess, using standardised patients (SPs), how rheumatologists diagnose psoriatic arthritis, whether the diagnostic efficiency is influenced by specific characteristics of the rheumatologists, and to study the relationship with costs.
Methods: Twenty three rheumatologists were each visited by one of two SPs (one male, one female) presenting as a patient with psoriatic arthritis. SPs remained incognito for all meetings for the duration of the study. Immediately after the encounter, SPs completed case-specific checklists on the medical content of the encounter. Information on ordered laboratory and imaging tests was obtained from each hospital.
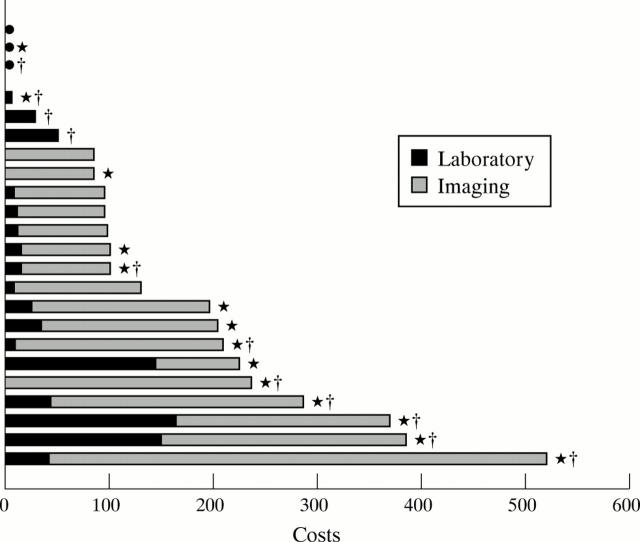
Results: Fourteen rheumatologists diagnosed psoriatic arthritis correctly. They inspected the skin for psoriatic lesions more often than those rheumatologists who established other diagnoses. Rheumatologists diagnosing psoriatic arthritis spent more on additional laboratory and imaging investigations. These were carried out after the diagnosis to confirm it and to record the extent and severity of the disease. No differences in type of practice, number of outpatients seen each week, working experience, or sex were found between rheumatologists who made the correct diagnosis and those who made other diagnoses. The correct diagnosis was more often missed by rheumatologists who saw the male SP, who presented with clear distal interphalangeal DIP joint arthritis only, causing confusion with osteoarthritis of the DIP joints.
Conclusion: There is a considerable amount of variation in the delivery of care among rheumatologists who see an SP with psoriatic arthritis. Rheumatologists focusing too much on the most prominent features (DIP joint arthritis) sometimes seem to forget "the hidden (skin) symptoms".
Full Text
The Full Text of this article is available as a PDF (104.6 KB).
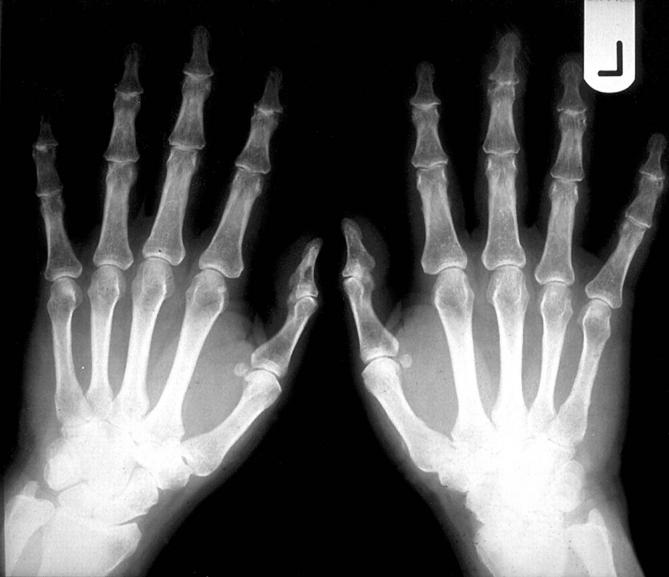
Figure 1 .
Radiograph of the hands of the male patient
Figure 2 .
Rheumatologists' costs spent for additional investigations. Every bar represents one rheumatologist; three rheumatologists (black circles) did not order any additional investigations.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barrows H. S. An overview of the uses of standardized patients for teaching and evaluating clinical skills. AAMC. Acad Med. 1993 Jun;68(6):443–453. doi: 10.1097/00001888-199306000-00002. [DOI] [PubMed] [Google Scholar]
- Davis D. A., Thomson M. A., Oxman A. D., Haynes R. B. Changing physician performance. A systematic review of the effect of continuing medical education strategies. JAMA. 1995 Sep 6;274(9):700–705. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- Gorter S., van der Linden S., Brauer J., van der Heijde D., Houben H., Rethans J. J., Scherpbier A., van der Vleuten C., Boonen A., Dinant H. Rhemulatologists' performance in dailiy practice. Arthritis Rheum. 2001 Feb;45(1):16–27. doi: 10.1002/1529-0131(200102)45:1<16::AID-ANR79>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- Gorter Simone L., Rethans Jan-Joost, Scherpbier Albert J.J.A., van Der Linden Sjef, van Santen-Hoeufft Marijke H.M., van Der Heijde Désirée M.F.M., Houben Harry H.M.L., van Der Vleuten Cees P.M. How to introduce incognito standardized patients into outpatient clinics of specialists in rheumatology. Med Teach. 2001 Mar;23(2):138–144. doi: 10.1080/014215931048. [DOI] [PubMed] [Google Scholar]
- Lomas J., Anderson G. M., Domnick-Pierre K., Vayda E., Enkin M. W., Hannah W. J. Do practice guidelines guide practice? The effect of a consensus statement on the practice of physicians. N Engl J Med. 1989 Nov 9;321(19):1306–1311. doi: 10.1056/NEJM198911093211906. [DOI] [PubMed] [Google Scholar]
- Rethans J. J., Westin S., Hays R. Methods for quality assessment in general practice. Fam Pract. 1996 Oct;13(5):468–476. doi: 10.1093/fampra/13.5.468. [DOI] [PubMed] [Google Scholar]