Abstract
Objectives: To estimate the incidence of postinfectious joint complaints after Campylobacter jejuni/coli enteritis compared with enteritis caused by enterotoxigenic E coli (ETEC). To compare gastrointestinal symptoms, antibiotic treatment, and antibody levels among patients with and without joint symptoms.
Method: Questionnaires were sent to 210 consecutive patients with Campylobacter infection and an equal number of patients with E coli (ETEC). Blood samples for anti-Campylobacter antibodies were collected after two weeks, three months, six months, and two years.
Results: Twenty seven of 173 (16%) patients with Campylobacter and 10/177 (6%) with E coli (ETEC) reported joint symptoms (p=0.004). In the Campylobacter group duration of diarrhoea was a median of 13 days for patients with arthralgia and seven days for those without joint pain (p=0.0058). Patients with E coli had diarrhoea of longer duration than patients infected with Campylobacter (14 days v seven days; p=0.0005). E coli patients had fewer gastrointestinal symptoms than Campylobacter patients (p=0.0001). Fifty nine per cent of Campylobacter patients with joint pain had received antibiotic treatment because of enteritis compared with 26% with enteritis only (p=0.03). Campylobacter species and serotypes were equally distributed in both groups and there was no difference in anti-Campylobacter antibody levels between the groups.
Conclusion: There was a significantly increased risk of developing joint symptoms after contracting Campylobacter infection compared with E coli. Campylobacter patients with joint pain had more severe gastrointestinal symptoms and longer duration of diarrhoea. Antibiotic treatment does not seem to prevent reactive joint symptoms. Levels of anti-Campylobacter antibodies were the same in both groups.
Full Text
The Full Text of this article is available as a PDF (118.5 KB).
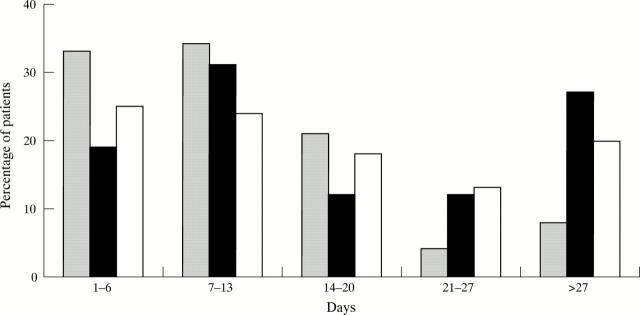
Figure 1 .
Duration of diarrhoea among 146 patients with Campylobacter enteritis (grey columns), 27 patients with Campylobacter ReA (black columns), and 167 patients with non-ReA E coli (ETEC) enteritis (white columns).
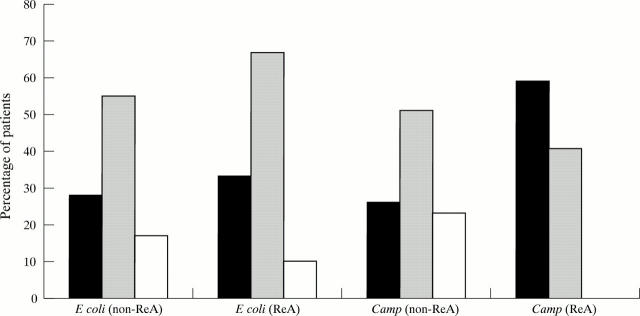
Figure 2 .
Individual gastrointestinal symptoms among 146 patients with Campylobacter enteritis (grey columns), 27 patients with Campylobacter ReA (black columns) (*p= 0.02, Campylobacter enteritis v Campylobacter ReA), and 167 patients with non ReA E coli (ETEC) enteritis (white columns) (**p= 0.0001, Campylobacter enteritis v E coli (ETEC) enteritis).
Figure 3 .
Proportions of patients treated with antibiotics for enteritis after infection with Campylobacter or E coli (ETEC). (Black columns, antibiotic treated; grey columns, untreated; white columns, don't remember). Campylobacter ReA v non-ReA; p=0.03.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Altekruse S. F., Stern N. J., Fields P. I., Swerdlow D. L. Campylobacter jejuni--an emerging foodborne pathogen. Emerg Infect Dis. 1999 Jan-Feb;5(1):28–35. doi: 10.3201/eid0501.990104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altekruse S. F., Swerdlow D. L., Stern N. J. Microbial food borne pathogens. Campylobacter jejuni. Vet Clin North Am Food Anim Pract. 1998 Mar;14(1):31–40. [PubMed] [Google Scholar]
- Asbury A. K. New concepts of Guillain-Barré syndrome. J Child Neurol. 2000 Mar;15(3):183–191. doi: 10.1177/088307380001500308. [DOI] [PubMed] [Google Scholar]
- Bremell T., Bjelle A., Svedhem A. Rheumatic symptoms following an outbreak of campylobacter enteritis: a five year follow up. Ann Rheum Dis. 1991 Dec;50(12):934–938. doi: 10.1136/ard.50.12.934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feldman R. A., Banatvala N. The frequency of culturing stools from adults with diarrhoea in Great Britain. Epidemiol Infect. 1994 Aug;113(1):41–44. doi: 10.1017/s095026880005144x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frydén A., Bengtsson A., Foberg U., Svenungsson B., Castor B., Kärnell A., Schvarcz R., Lindblom B., Kihlström E. Early antibiotic treatment of reactive arthritis associated with enteric infections: clinical and serological study. BMJ. 1990 Dec 8;301(6764):1299–1302. doi: 10.1136/bmj.301.6764.1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Granfors K., Viljanen M., Tiilikainen A., Toivanen A. Persistence of IgM, IgG, and IgA antibodies to Yersinia in yersinia arthritis. J Infect Dis. 1980 Apr;141(4):424–429. doi: 10.1093/infdis/141.4.424. [DOI] [PubMed] [Google Scholar]
- Gumpel J. M., Martin C., Sanderson P. J. Reactive arthritis associated with campylobacter enteritis. Ann Rheum Dis. 1981 Feb;40(1):64–65. doi: 10.1136/ard.40.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inman R. D., Johnston M. E., Hodge M., Falk J., Helewa A. Postdysenteric reactive arthritis. A clinical and immunogenetic study following an outbreak of salmonellosis. Arthritis Rheum. 1988 Nov;31(11):1377–1383. doi: 10.1002/art.1780311106. [DOI] [PubMed] [Google Scholar]
- Kihlström E., Foberg U., Bengtsson A., Frydén A., Svenungsson B., Schvarcz R., Lindblom B., Castor B. Intestinal symptoms and serological response in patients with complicated and uncomplicated Yersinia enterocolitica infections. Scand J Infect Dis. 1992;24(1):57–63. doi: 10.3109/00365549209048401. [DOI] [PubMed] [Google Scholar]
- Kosunen T. U., Pönkä A., Kauranen O., Martio J., Pitkänen T., Hortling L., Aittoniemi S., Penttilä O., Koskimies S. Arthritis associated with Campylobacter jejuni enteritis. Scand J Rheumatol. 1981;10(2):77–80. doi: 10.3109/03009748109095276. [DOI] [PubMed] [Google Scholar]
- Lauhio A., Leirisalo-Repo M., Lähdevirta J., Saikku P., Repo H. Double-blind, placebo-controlled study of three-month treatment with lymecycline in reactive arthritis, with special reference to Chlamydia arthritis. Arthritis Rheum. 1991 Jan;34(1):6–14. doi: 10.1002/art.1780340103. [DOI] [PubMed] [Google Scholar]
- Locht H., Kihlström E., Lindström F. D. Reactive arthritis after Salmonella among medical doctors--study of an outbreak. J Rheumatol. 1993 May;20(5):845–848. [PubMed] [Google Scholar]
- Mäki-Ikola O., Leirisalo-Repo M., Kantele A., Toivanen P., Granfors K. Salmonella-specific antibodies in reactive arthritis. J Infect Dis. 1991 Dec;164(6):1141–1148. doi: 10.1093/infdis/164.6.1141. [DOI] [PubMed] [Google Scholar]
- Noer H. R. An "experimental" epidemic of Reiter's syndrome. JAMA. 1966 Nov 14;198(7):693–698. [PubMed] [Google Scholar]
- Pitkänen T., Pönkä A., Pettersson T., Kosunen T. U. Campylobacter enteritis in 188 hospitalized patients. Arch Intern Med. 1983 Feb;143(2):215–219. doi: 10.1001/archinte.1983.00350020033007. [DOI] [PubMed] [Google Scholar]
- Pönkä A., Pitkänen T., Sarna S., Kosunen T. U. Infection due to Campylobacter jejuni: a report of 524 outpatients. Infection. 1984 May-Jun;12(3):175–178. doi: 10.1007/BF01640893. [DOI] [PubMed] [Google Scholar]
- Samuel M. P., Zwillich S. H., Thomson G. T., Alfa M., Orr K. B., Brittain D. C., Miller J. R., Phillips P. E. Fast food arthritis--a clinico-pathologic study of post-Salmonella reactive arthritis. J Rheumatol. 1995 Oct;22(10):1947–1952. [PubMed] [Google Scholar]
- Sieper J., Fendler C., Laitko S., Sörensen H., Gripenberg-Lerche C., Hiepe F., Alten R., Keitel W., Groh A., Uksila J. No benefit of long-term ciprofloxacin treatment in patients with reactive arthritis and undifferentiated oligoarthritis: a three-month, multicenter, double-blind, randomized, placebo-controlled study. Arthritis Rheum. 1999 Jul;42(7):1386–1396. doi: 10.1002/1529-0131(199907)42:7<1386::AID-ANR12>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Strid M. A., Engberg J., Larsen L. B., Begtrup K., Mølbak K., Krogfelt K. A. Antibody responses to Campylobacter infections determined by an enzyme-linked immunosorbent assay: 2-year follow-up study of 210 patients. Clin Diagn Lab Immunol. 2001 Mar;8(2):314–319. doi: 10.1128/CDLI.8.2.314-319.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson G. T., Chiu B., De Rubeis D., Falk J., Inman R. D. Immunoepidemiology of post-Salmonella reactive arthritis in a cohort of women. Clin Immunol Immunopathol. 1992 Sep;64(3):227–232. doi: 10.1016/0090-1229(92)90204-2. [DOI] [PubMed] [Google Scholar]
- van de Putte L. B., Berden J. H., Boerbooms M. T., Muller W. H., Rasker J. J., Reynvaan-Groendijk A., van der Linden S. M. Reactive arthritis after Campylobacter jejuni enteritis. J Rheumatol. 1980 Jul-Aug;7(4):531–535. [PubMed] [Google Scholar]