Abstract
Objective: To compare the economic burden to society incurred by patients with RA, OA, or high blood pressure (HBP) in Ontario, Canada.
Methods: Consecutive subjects recruited by 52 rheumatologists (RA) and 76 family physicians (OA and HBP) were interviewed at baseline and 3 months. Information was collected on demographics, health status, and any comorbidities. A detailed, open ended resource utilisation questionnaire inquired about the use of medical and non-medical resources and patient and care giver losses of time and related expenses. Annual costs were derived as recommended by national costing guidelines and converted to American dollars (year 2000). Statistical comparisons were made using ordinary least squares regression on raw and log transformed costs, and generalised linear modelling with adjustment for age, sex, educational attainment, and presence of comorbidities.
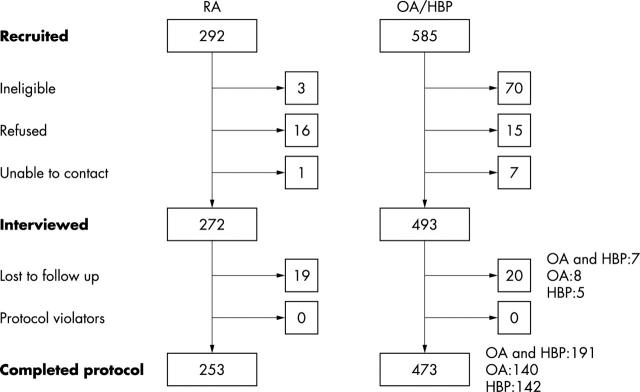
Results: Baseline and 3 month interviews were completed by 253/292 (86.6%) patients with RA and 473/585 (80.9%) patients with OA and/or HBP. Baseline and total annual disease costs for RA (n = 253), OA and HBP (n = 191), OA (n = 140), and HBP (n = 142), respectively, were $9300, $4900, $5700, and US$3900. Indirect costs related to RA were up to five times higher than indirect costs incurred by patients with OA or HBP, or both. The presence of comorbidities was associated with disease costs for all diagnoses, cancelling out potential effects of age or sex.
Conclusion: The economic burden incurred by RA significantly exceeds that related to OA and HBP, while differences between patients with a diagnosis of OA without HBP or a diagnosis of HBP alone were non-significant, largely owing to the influence of comorbidities.
Full Text
The Full Text of this article is available as a PDF (281.0 KB).
Figure 1 .
Recruitment flow diagram of patients with rheumatoid arthritis (RA), osteoarthritis (OA), or high blood pressure (HBP).
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bloom B. S., Bruno D. J., Maman D. Y., Jayadevappa R. Usefulness of US cost-of-illness studies in healthcare decision making. Pharmacoeconomics. 2001;19(2):207–213. doi: 10.2165/00019053-200119020-00007. [DOI] [PubMed] [Google Scholar]
- Chang B. H., Pocock S. Analyzing data with clumping at zero. An example demonstration. J Clin Epidemiol. 2000 Oct;53(10):1036–1043. doi: 10.1016/s0895-4356(00)00223-7. [DOI] [PubMed] [Google Scholar]
- Clarke A. E., Penrod J., St Pierre Y., Petri M. A., Manzi S., Isenberg D. A., Gordon C., Senecal J. L., Fortin P. R., Sutcliffe N. Underestimating the value of women: assessing the indirect costs of women with systemic lupus erythematosus. Tri-Nation Study Group. J Rheumatol. 2000 Nov;27(11):2597–2604. [PubMed] [Google Scholar]
- Clarke A. E., Zowall H., Levinton C., Assimakopoulos H., Sibley J. T., Haga M., Shiroky J., Neville C., Lubeck D. P., Grover S. A. Direct and indirect medical costs incurred by Canadian patients with rheumatoid arthritis: a 12 year study. J Rheumatol. 1997 Jun;24(6):1051–1060. [PubMed] [Google Scholar]
- Fautrel Bruno, Guillemin Francis. Cost of illness studies in rheumatic diseases. Curr Opin Rheumatol. 2002 Mar;14(2):121–126. doi: 10.1097/00002281-200203000-00008. [DOI] [PubMed] [Google Scholar]
- Fries J. F., Spitz P. W., Young D. Y. The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. J Rheumatol. 1982 Sep-Oct;9(5):789–793. [PubMed] [Google Scholar]
- Fries J. F., Spitz P., Kraines R. G., Holman H. R. Measurement of patient outcome in arthritis. Arthritis Rheum. 1980 Feb;23(2):137–145. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- Gabriel S. E., Crowson C. S., O'Fallon W. M. Costs of osteoarthritis: estimates from a geographically defined population. J Rheumatol Suppl. 1995 Feb;43:23–25. [PubMed] [Google Scholar]
- Kobelt G., Eberhardt K., Jönsson L., Jönsson B. Economic consequences of the progression of rheumatoid arthritis in Sweden. Arthritis Rheum. 1999 Feb;42(2):347–356. doi: 10.1002/1529-0131(199902)42:2<347::AID-ANR18>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- Koopmanschap M. A. Cost-of-illness studies. Useful for health policy? Pharmacoeconomics. 1998 Aug;14(2):143–148. doi: 10.2165/00019053-199814020-00001. [DOI] [PubMed] [Google Scholar]
- Koopmanschap M. A., van Ineveld B. M. Towards a new approach for estimating indirect costs of disease. Soc Sci Med. 1992 May;34(9):1005–1010. doi: 10.1016/0277-9536(92)90131-9. [DOI] [PubMed] [Google Scholar]
- Lawrence R. C., Helmick C. G., Arnett F. C., Deyo R. A., Felson D. T., Giannini E. H., Heyse S. P., Hirsch R., Hochberg M. C., Hunder G. G. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998 May;41(5):778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- Manning W. G., Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001 Jul;20(4):461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- Ruof J., Merkesdal S., Huelsemann J. L., Schoeffski O., Maetzel A., Mau W., Zeidler H. Cost assessment instrument in rheumatology: evaluation of applied instrument characteristics. J Rheumatol. 2001 Mar;28(3):662–665. [PubMed] [Google Scholar]
- Rutten-van Mölken M. P., van Doorslaer E. K., van Vliet R. C. Statistical analysis of cost outcomes in a randomized controlled clinical trial. Health Econ. 1994 Sep-Oct;3(5):333–345. doi: 10.1002/hec.4730030507. [DOI] [PubMed] [Google Scholar]
- Stewart A. L., Hays R. D., Ware J. E., Jr The MOS short-form general health survey. Reliability and validity in a patient population. Med Care. 1988 Jul;26(7):724–735. doi: 10.1097/00005650-198807000-00007. [DOI] [PubMed] [Google Scholar]