Abstract
Objectives: Takayasu's arteritis (TA) is a rare disease, in which early diagnosis and assessment of treatment efficacy remain a problem. Signs and symptoms may be non-specific and conventional blood tests unreliable, with vascular inflammation often persisting in the face of a normal acute phase response. The current "gold standard" investigation, x ray angiography, is invasive and only identifies late, structural changes in vessels. Recently, non-invasive imaging methods have shown promise in the assessment of patients with TA.
Methods: The invasive and non-invasive imaging performed on all patients in the rheumatology department at the Hammersmith Hospital between May 1996 and May 2002 who fulfilled the ACR criteria for TA were reviewed. All patients were clinically active at diagnosis and were treated with high dose oral prednisolone and additional oral or intravenous immunosuppression.
Results: Non-invasive imaging methods ([18F]fluorodeoxyglucose positron emission tomography ([18F]FDG-PET) and magnetic resonance imaging (MRI)) provided important additional information about disease activity ([18F]FDG-PET) and progression of vessel wall thickening (MRI) when compared with x ray angiography.
Conclusions: Non-invasive imaging methods provide useful additional information towards the diagnosis and management of TA. Such techniques may allow earlier diagnosis and more accurate assessment of response to treatment than conventional clinical assessment and/or angiography. Non-invasive imaging is likely to be useful in the management of other large vessel vasculitides.
Full Text
The Full Text of this article is available as a PDF (137.5 KB).
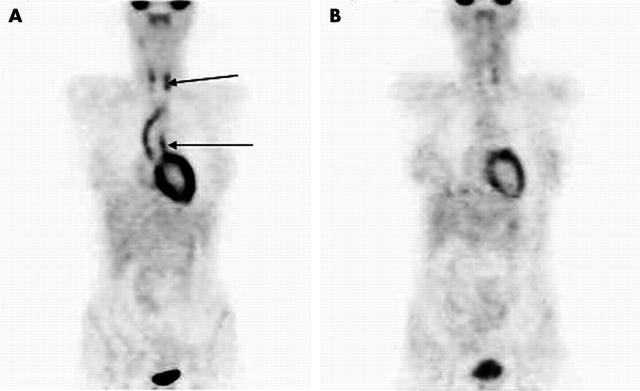
Figure 1.
(A) [18F]FDG-PET scan of patient 5 with active TA at diagnosis. Note the markedly abnormal uptake of [18F]FDG in the aortic arch and carotid arteries (arrows). (B) [18F]FDG-PET scan of the same patient in remission after treatment with prednisolone and intravenous cyclophosphamide. Note almost complete resolution of abnormal [18F]FDG uptake in these areas.
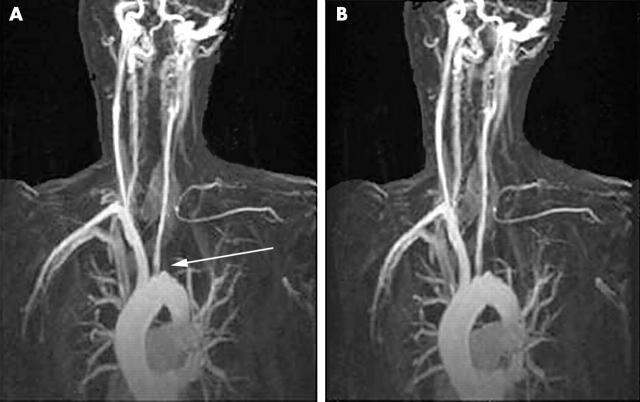
Figure 2.
(A) Magnetic resonance angiography (MRA) image from patient 5 with active TA at diagnosis. There is complete occlusion of the left subclavian artery at its origin (arrow) with numerous collaterals evident and an ostial stenosis of the left common carotid artery. (B) MRA image from the same patient in remission. No significant progression of the lesions found on the baseline MRA is seen.
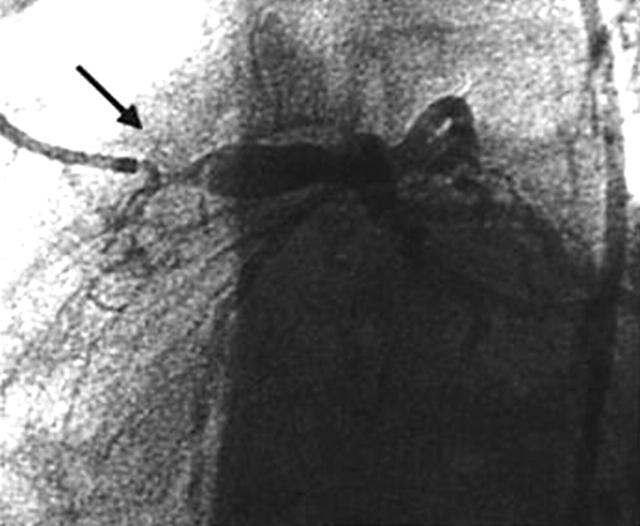
Figure 3.
Coronary angiography image from patient number 5 with active TA at diagnosis. A tight stenosis can be seen at the origin of the left main stem coronary artery (arrow). Shortly after this image was recorded, she had a VF cardiac arrest and the left main stem was found to have occluded. After resuscitation, the left main stem was rapidly re-opened with the insertion of a coronary stent without further complication.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arend W. P., Michel B. A., Bloch D. A., Hunder G. G., Calabrese L. H., Edworthy S. M., Fauci A. S., Leavitt R. Y., Lie J. T., Lightfoot R. W., Jr The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis. Arthritis Rheum. 1990 Aug;33(8):1129–1134. doi: 10.1002/art.1780330811. [DOI] [PubMed] [Google Scholar]
- Belhocine Tarik, Blockmans Daniel, Hustinx Roland, Vandevivere Johan, Mortelmans Luc. Imaging of large vessel vasculitis with (18)FDG PET: illusion or reality? A critical review of the literature data. Eur J Nucl Med Mol Imaging. 2003 Jun 17;30(9):1305–1313. doi: 10.1007/s00259-003-1209-y. [DOI] [PubMed] [Google Scholar]
- Blockmans D., Maes A., Stroobants S., Nuyts J., Bormans G., Knockaert D., Bobbaers H., Mortelmans L. New arguments for a vasculitic nature of polymyalgia rheumatica using positron emission tomography. Rheumatology (Oxford) 1999 May;38(5):444–447. doi: 10.1093/rheumatology/38.5.444. [DOI] [PubMed] [Google Scholar]
- Hall S., Barr W., Lie J. T., Stanson A. W., Kazmier F. J., Hunder G. G. Takayasu arteritis. A study of 32 North American patients. Medicine (Baltimore) 1985 Mar;64(2):89–99. [PubMed] [Google Scholar]
- Hoffman G. S., Ahmed A. E. Surrogate markers of disease activity in patients with Takayasu arteritis. A preliminary report from The International Network for the Study of the Systemic Vasculitides (INSSYS). Int J Cardiol. 1998 Oct 1;66 (Suppl 1):S191–S195. doi: 10.1016/s0167-5273(98)00181-8. [DOI] [PubMed] [Google Scholar]
- Kerr G. S., Hallahan C. W., Giordano J., Leavitt R. Y., Fauci A. S., Rottem M., Hoffman G. S. Takayasu arteritis. Ann Intern Med. 1994 Jun 1;120(11):919–929. doi: 10.7326/0003-4819-120-11-199406010-00004. [DOI] [PubMed] [Google Scholar]
- Marcos H. B., Choyke P. L. Magnetic resonance angiography of the kidney. Semin Nephrol. 2000 Sep;20(5):450–455. [PubMed] [Google Scholar]
- Matsunaga N., Hayashi K., Sakamoto I., Matsuoka Y., Ogawa Y., Honjo K., Takano K. Takayasu arteritis: MR manifestations and diagnosis of acute and chronic phase. J Magn Reson Imaging. 1998 Mar-Apr;8(2):406–414. doi: 10.1002/jmri.1880080221. [DOI] [PubMed] [Google Scholar]
- Meller J., Grabbe E., Becker W., Vosshenrich R. Value of F-18 FDG hybrid camera PET and MRI in early takayasu aortitis. Eur Radiol. 2002 Jun 29;13(2):400–405. doi: 10.1007/s00330-002-1518-8. [DOI] [PubMed] [Google Scholar]
- Meller J., Strutz F., Siefker U., Scheel A., Sahlmann C. O., Lehmann K., Conrad M., Vosshenrich R. Early diagnosis and follow-up of aortitis with [(18)F]FDG PET and MRI. Eur J Nucl Med Mol Imaging. 2003 Apr 4;30(5):730–736. doi: 10.1007/s00259-003-1144-y. [DOI] [PubMed] [Google Scholar]
- Tso Elisa, Flamm Scott D., White Richard D., Schvartzman Paulo R., Mascha Edward, Hoffman Gary S. Takayasu arteritis: utility and limitations of magnetic resonance imaging in diagnosis and treatment. Arthritis Rheum. 2002 Jun;46(6):1634–1642. doi: 10.1002/art.10251. [DOI] [PubMed] [Google Scholar]
- Zhuang Hongming, Alavi Abass. 18-fluorodeoxyglucose positron emission tomographic imaging in the detection and monitoring of infection and inflammation. Semin Nucl Med. 2002 Jan;32(1):47–59. doi: 10.1053/snuc.2002.29278. [DOI] [PubMed] [Google Scholar]