Abstract
Objective: To assess methods to calculate achieving and sustaining remission in a double blind randomised trial in patients with RA who received etanercept, methotrexate, or an etanercept/methotrexate combination.
Methods: Remission was defined as DAS <1.6, DAS28 <2.6, and ACR70 response. Sustaining remission was analysed in three ways: (a) analysis of sustained DAS remission, DAS28 remission, or ACR70 response continuously for 6 months; (b) analysis of sustained remission appraised through a continuity rewarded scoring system, which is the weighted sum of all intervals in the study in which patients are in DAS or DAS28 remission; or (c) longitudinal modelling of remission odds using generalised estimating equations.
Results: Significantly more patients treated with the etanercept/methotrexate combination reached DAS remission (37%) than those treated with either methotrexate (14%) or etanercept (18%) alone (p<0.01). Results for DAS28 and for the ACR70 response were similar. Agreement between DAS remission and DAS28 remission was good, but agreement between either of these and the ACR70 response was less. Patients in DAS or DAS28 remission had a lower level of disease activity (fewer active joints, lower ESR) than those achieving ACR70 response; the converse was seen using pain VAS. The three methods were comparable for sustainability of remission and showed significant advantage for combination therapy, which increased the number and durability of remission periods.
Conclusions: DAS and DAS28 remission results were similar for assessing achieving and sustaining remission in RA, frequently differing from patients classified as ACR70 responders. The three methods of examining duration of remission produced comparable results.
Full Text
The Full Text of this article is available as a PDF (144.7 KB).
Figure 1.
Tender joint count distribution among patients in DAS remission, DAS28 remission, and fulfilling ACR70 response. Mean (SD) tender joint counts for DAS remission, DAS28 remission, and ACR70 responders were 0.4 (1.2), 1.2 (2.4), and 1.8 (2.5), respectively. Medians (25%–75% interquartile range (IQR)) for DAS remission, DAS28 remission, and ACR70 responders were 0 (0–0), 0 (0–2), and 1 (0–3), respectively.
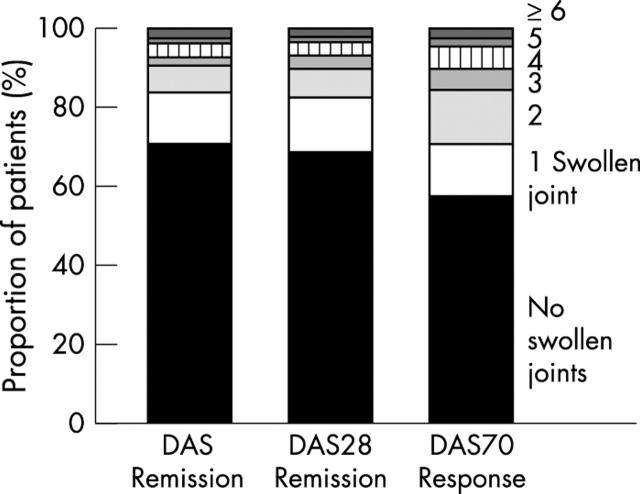
Figure 4.
Pain visual analogue scale (VAS) for patients in DAS remission, DAS28 remission and fulfilling ACR70 response, ordered from the lowest to the highest value and expressed as the cumulative probability. Means (SD) for DAS remission, DAS28 remission, and ACR70 responders were 11.5 (12.3), 11.8 (11.3), and 9.0 (8.6), respectively. Medians (25%–75% IQR) for DAS remission, DAS28 remission, and ACR70 responders were 8.0 (2–17), 10 (2–18), and 8 (2–13), respectively.
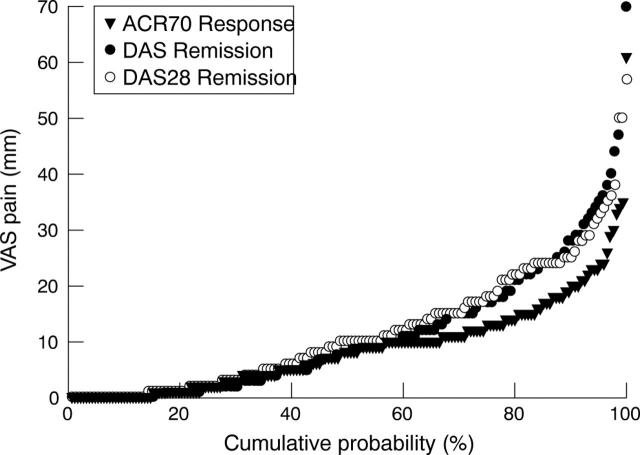
Figure 2.
Swollen joint count distribution among patients in DAS remission, DAS28 remission, and fulfilling ACR70 response. Mean (SD) swollen joint count for DAS remission, DAS28 remission, and ACR70 responders were 0.8 (1.6), 0.8 (1.6), and 1.1 (1.8), respectively. Medians (25%–75% IQR) for DAS remission, DAS28 remission, and ACR70 responders were 0 (0–1), 0 (0–1), and 0 (0–2), respectively.
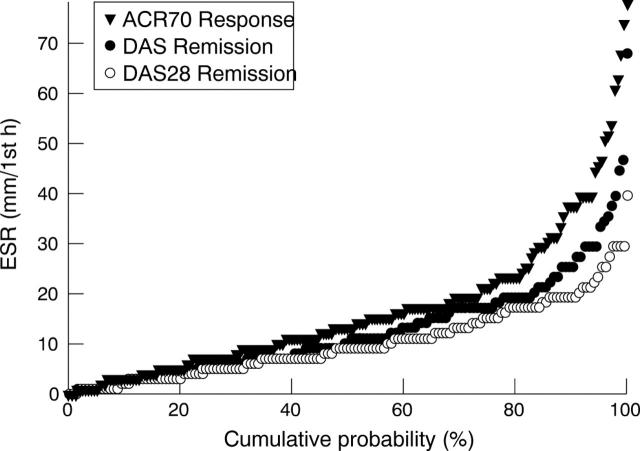
Figure 3.
Erythrocyte sedimentation rate (ESR) for individual patients in DAS remission, DAS28 remission, and fulfilling ACR70 response, ordered from the lowest to the highest value and expressed as the cumulative probability. Means (SD) for DAS remission, DAS28 remission, and ACR70 responders were 13.6 (10.5), 11.2 (7.3), and 17.7 (14.4), respectively. Medians (25%–75% IQR) for DAS remission, DAS28 remission, and ACR70 responders were 11 (6–18), 10 (6–16), and 14 (8–22), respectively.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cooper N. J. Economic burden of rheumatoid arthritis: a systematic review. Rheumatology (Oxford) 2000 Jan;39(1):28–33. doi: 10.1093/rheumatology/39.1.28. [DOI] [PubMed] [Google Scholar]
- Felson D. T., Anderson J. J., Boers M., Bombardier C., Chernoff M., Fried B., Furst D., Goldsmith C., Kieszak S., Lightfoot R. The American College of Rheumatology preliminary core set of disease activity measures for rheumatoid arthritis clinical trials. The Committee on Outcome Measures in Rheumatoid Arthritis Clinical Trials. Arthritis Rheum. 1993 Jun;36(6):729–740. doi: 10.1002/art.1780360601. [DOI] [PubMed] [Google Scholar]
- Fransen J., Creemers M. C. W., Van Riel P. L. C. M. Remission in rheumatoid arthritis: agreement of the disease activity score (DAS28) with the ARA preliminary remission criteria. Rheumatology (Oxford) 2004 Jul 6;43(10):1252–1255. doi: 10.1093/rheumatology/keh297. [DOI] [PubMed] [Google Scholar]
- Gabriel S., Tugwell P., O'Brien B., Yelin E., Drummond M., Ruff B., Brooks P., Bombardier C., Boers M. Report of the OMERACT task force on economic evaluation. Outcome Measures in Rheumatology. J Rheumatol. 1999 Jan;26(1):203–206. [PubMed] [Google Scholar]
- Klareskog Lars, van der Heijde Désirée, de Jager Julien P., Gough Andrew, Kalden Joachim, Malaise Michel, Martín Mola Emilio, Pavelka Karel, Sany Jacques, Settas Lucas. Therapeutic effect of the combination of etanercept and methotrexate compared with each treatment alone in patients with rheumatoid arthritis: double-blind randomised controlled trial. Lancet. 2004 Feb 28;363(9410):675–681. doi: 10.1016/S0140-6736(04)15640-7. [DOI] [PubMed] [Google Scholar]
- Kvien Tore K. Epidemiology and burden of illness of rheumatoid arthritis. Pharmacoeconomics. 2004;22(2 Suppl 1):1–12. doi: 10.2165/00019053-200422001-00002. [DOI] [PubMed] [Google Scholar]
- Lee D. M., Weinblatt M. E. Rheumatoid arthritis. Lancet. 2001 Sep 15;358(9285):903–911. doi: 10.1016/S0140-6736(01)06075-5. [DOI] [PubMed] [Google Scholar]
- Molenaar Esmeralda T. H., Voskuyl Alexandre E., Dinant Huib J., Bezemer P. Dick, Boers Maarten, Dijkmans Ben A. C. Progression of radiologic damage in patients with rheumatoid arthritis in clinical remission. Arthritis Rheum. 2004 Jan;50(1):36–42. doi: 10.1002/art.11481. [DOI] [PubMed] [Google Scholar]
- Navarro-Cano Gregorio, Del Rincón Inmaculada, Pogosian Samvel, Roldán José F., Escalante Agustín. Association of mortality with disease severity in rheumatoid arthritis, independent of comorbidity. Arthritis Rheum. 2003 Sep;48(9):2425–2433. doi: 10.1002/art.11127. [DOI] [PubMed] [Google Scholar]
- Pinals R. S., Masi A. T., Larsen R. A. Preliminary criteria for clinical remission in rheumatoid arthritis. Arthritis Rheum. 1981 Oct;24(10):1308–1315. doi: 10.1002/art.1780241012. [DOI] [PubMed] [Google Scholar]
- Prevoo M. L., van Gestel A. M., van T Hof M. A., van Rijswijk M. H., van de Putte L. B., van Riel P. L. Remission in a prospective study of patients with rheumatoid arthritis. American Rheumatism Association preliminary remission criteria in relation to the disease activity score. Br J Rheumatol. 1996 Nov;35(11):1101–1105. doi: 10.1093/rheumatology/35.11.1101. [DOI] [PubMed] [Google Scholar]
- van Gestel A. M., Anderson J. J., van Riel P. L., Boers M., Haagsma C. J., Rich B., Wells G., Lange M. L., Felson D. T. ACR and EULAR improvement criteria have comparable validity in rheumatoid arthritis trials. American College of Rheumatology European League of Associations for Rheumatology. J Rheumatol. 1999 Mar;26(3):705–711. [PubMed] [Google Scholar]
- van Riel P. L., van Gestel A. M. Clinical outcome measures in rheumatoid arthritis. Ann Rheum Dis. 2000 Nov;59 (Suppl 1):i28–i31. doi: 10.1136/ard.59.suppl_1.i28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Heijde D. M., van 't Hof M., van Riel P. L., van de Putte L. B. Development of a disease activity score based on judgment in clinical practice by rheumatologists. J Rheumatol. 1993 Mar;20(3):579–581. [PubMed] [Google Scholar]