Abstract
Background: Retroperitoneal fibrosis (RPF) and inflammatory aneurysm of the abdominal aorta (IAAA) are regarded as two manifestations of the same disease, termed "chronic periaortitis".
Objective: To determine the optimal therapeutic and diagnostic approaches to IAAA.
Methods: The outcome of medical immunosuppressive and surgical treatment of 20 patients was examined. Measurements of the C reactive protein (CRP) were compared with contrast enhanced imaging studies in the follow up of the patients.
Results: The diameter of the periaortic mantle and its contrast enhancement improved in 13/15 (87%) patients given immunosuppressive treatment for a period of more than 6 months. Strong contrast enhancement was associated with a substantial rise in CRP, but no correlation between the CRP value and thickness of the fibrotic mass was found, even at intraindividual follow up.
Conclusions: Immunosuppressive treatment should be included in the first line treatment of patients with RPF and should be maintained long term. Imaging studies are better than CRP measurements in the evaluation of response to treatment.
Full Text
The Full Text of this article is available as a PDF (199.7 KB).
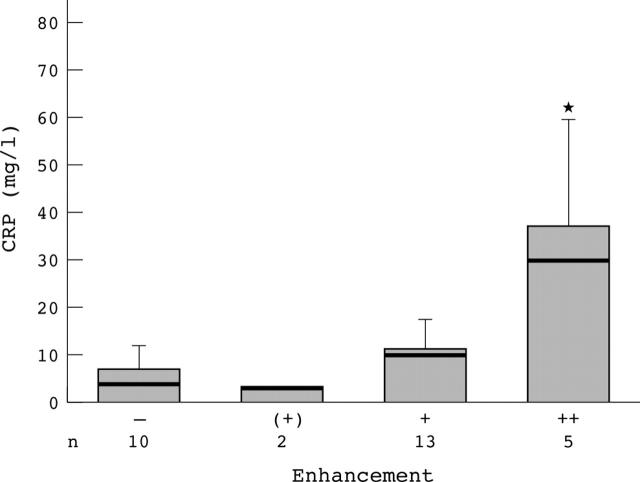
Figure 1.
Serial MRI study of RPF during immunosuppressive treatment. T1 weighted images of patient 2 after (A) 2, (B) 14, and (C) 26 months of immunosuppression, indicating the diameter of the periaortic mantle and gadolinium enhancement (absent "–", detectable "(+)", intermediate "+" and strong "++").
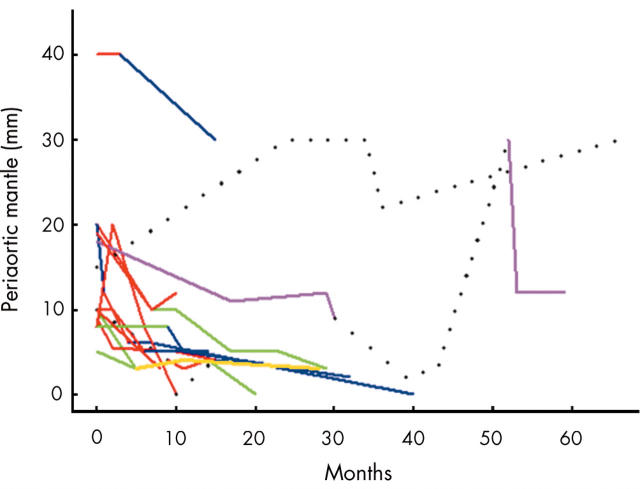
Figure 2.
Association of CRP values with the intensity of contrast enhancement. Significant increases (*p = 0.008) of CRP were detectable only with concomitant strong ("++") contrast enhancement. n = number of images. Bars represent means (SD). CRP medians are represented by the thick line within each bar.
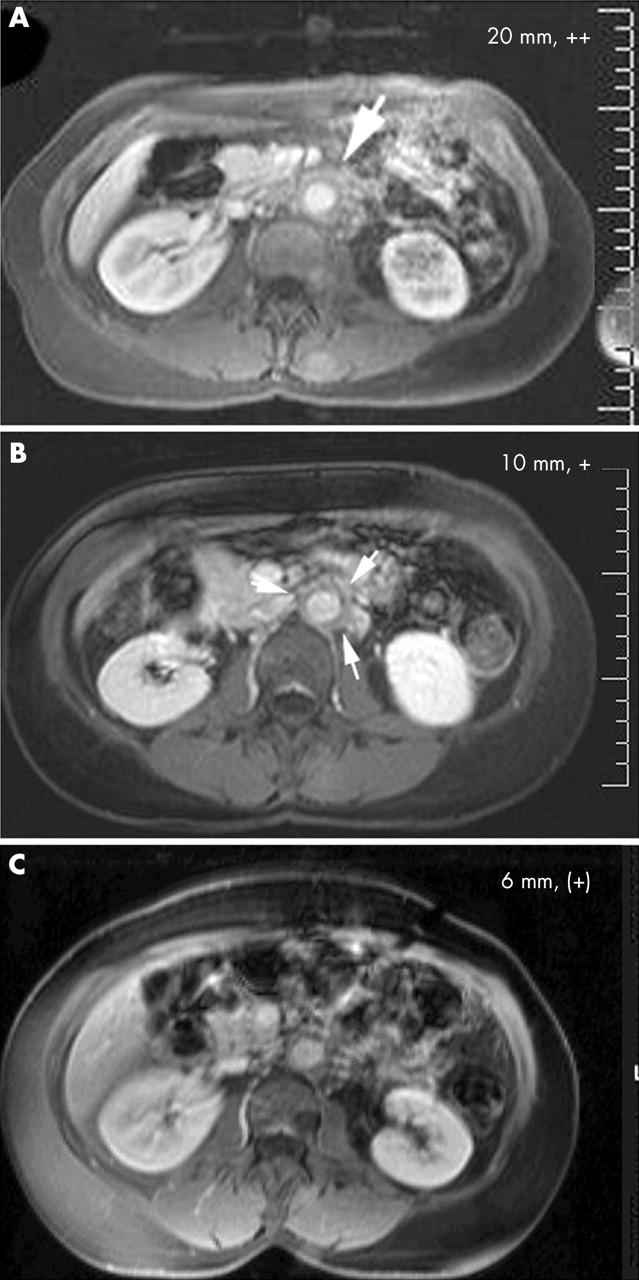
Figure 3.
Evolution of the periaortic mantle (thickness in mm) after the initiation of immunosuppressive treatment. Colours represent: AZA, green; CYC, red; MMF, purple; MTX, yellow; OCS, blue; no immunosuppression, black dots.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bachmann G., Bauer T., Rau W. S. MRT und CT in Diagnose und Verlaufskontrolle der idiopathischen (retroperitonealen) Fibrosen. Radiologe. 1995 Mar;35(3):200–207. [PubMed] [Google Scholar]
- Baker L. R., Mallinson W. J., Gregory M. C., Menzies E. A., Cattell W. R., Whitfield H. N., Hendry W. F., Wickham J. E., Joekes A. M. Idiopathic retroperitoneal fibrosis. A retrospective analysis of 60 cases. Br J Urol. 1987 Dec;60(6):497–503. doi: 10.1111/j.1464-410x.1987.tb05028.x. [DOI] [PubMed] [Google Scholar]
- Baskerville P. A., Blakeney C. G., Young A. E., Browse N. L. The diagnosis and treatment of peri-aortic fibrosis ('inflammatory' aneurysms). Br J Surg. 1983 Jun;70(6):381–385. doi: 10.1002/bjs.1800700623. [DOI] [PubMed] [Google Scholar]
- COSBIE ROSS J., TINCKLER L. F. Renal failure due to peri-ureteric fibrosis. Br J Surg. 1958 Jul;46(195):58–62. doi: 10.1002/bjs.18004619510. [DOI] [PubMed] [Google Scholar]
- Gans R. O., Hoorntje S. J., Rauwerda J. A., Luth W. J., van Hattum L. A., Donker A. J. The inflammatory abdominal aortic aneurysm. Prevalence, clinical features and diagnostic evaluation. Neth J Med. 1993 Oct;43(3-4):105–115. [PubMed] [Google Scholar]
- Gilkeson G. S., Allen N. B. Retroperitoneal fibrosis. A true connective tissue disease. Rheum Dis Clin North Am. 1996 Feb;22(1):23–38. doi: 10.1016/s0889-857x(05)70260-x. [DOI] [PubMed] [Google Scholar]
- Grotz W., von Zedtwitz I., Andre M., Schollmeyer P. Treatment of retroperitoneal fibrosis by mycophenolate mofetil and corticosteroids. Lancet. 1998 Oct 10;352(9135):1195–1195. doi: 10.1016/S0140-6736(05)60533-8. [DOI] [PubMed] [Google Scholar]
- Izzedine Hassane, Servais Aude, Launay-Vacher Vincent, Deray Gilbert. Retroperitoneal fibrosis due to Wegener's granulomatosis: a misdiagnosis as tuberculosis. Am J Med. 2002 Aug 1;113(2):164–166. doi: 10.1016/s0002-9343(02)01170-1. [DOI] [PubMed] [Google Scholar]
- Kaipiainen-Seppänen O., Jantunen E., Kuusisto J., Marin S. Retroperitoneal fibrosis with antineutrophil cytoplasmic antibodies. J Rheumatol. 1996 Apr;23(4):779–781. [PubMed] [Google Scholar]
- Koep L., Zuidema G. D. The clinical significance of retroperitoneal fibrosis. Surgery. 1977 Mar;81(3):250–257. [PubMed] [Google Scholar]
- Kohler H. P., Laeng R. H., Egger C., Streuli R. Systemische Fibrose (generalisierte Form des Morbus Ormond). Bericht über einen Fall, der mit Cyclophosphamid und Kortikosteroiden eine komplette Remission erlangte. Schweiz Med Wochenschr. 1995 Nov 4;125(44):2131–2136. [PubMed] [Google Scholar]
- Marcolongo Renzo, Tavolini Ivan Matteo, Laveder Francesco, Busa Moira, Noventa Franco, Bassi Pierfrancesco, Semenzato Gianpietro. Immunosuppressive therapy for idiopathic retroperitoneal fibrosis: a retrospective analysis of 26 cases. Am J Med. 2004 Feb 1;116(3):194–197. doi: 10.1016/j.amjmed.2003.08.033. [DOI] [PubMed] [Google Scholar]
- Marzano A., Trapani A., Leone N., Actis G. C., Rizzetto M. Treatment of idiopathic retroperitoneal fibrosis using cyclosporin. Ann Rheum Dis. 2001 Apr;60(4):427–428. doi: 10.1136/ard.60.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchinson M. J. Chronic periaortitis and periarteritis. Histopathology. 1984 Jul;8(4):589–600. doi: 10.1111/j.1365-2559.1984.tb02371.x. [DOI] [PubMed] [Google Scholar]
- Mulligan S. A., Holley H. C., Koehler R. E., Koslin D. B., Rubin E., Berland L. L., Kenney P. J. CT and MR imaging in the evaluation of retroperitoneal fibrosis. J Comput Assist Tomogr. 1989 Mar-Apr;13(2):277–281. doi: 10.1097/00004728-198903000-00018. [DOI] [PubMed] [Google Scholar]
- Nitecki S. S., Hallett J. W., Jr, Stanson A. W., Ilstrup D. M., Bower T. C., Cherry K. J., Jr, Gloviczki P., Pairolero P. C. Inflammatory abdominal aortic aneurysms: a case-control study. J Vasc Surg. 1996 May;23(5):860–869. doi: 10.1016/s0741-5214(96)70249-5. [DOI] [PubMed] [Google Scholar]
- Okada H., Takahira S., Sugahara S., Nakamoto H., Suzuki H. Retroperitoneal fibrosis and systemic lupus erythematosus. Nephrol Dial Transplant. 1999 May;14(5):1300–1302. doi: 10.1093/ndt/14.5.1300. [DOI] [PubMed] [Google Scholar]
- Owens L. V., Cance W. G., Huth J. F. Retroperitoneal fibrosis treated with tamoxifen. Am Surg. 1995 Sep;61(9):842–844. [PubMed] [Google Scholar]
- Parums D. V., Brown D. L., Mitchinson M. J. Serum antibodies to oxidized low-density lipoprotein and ceroid in chronic periaortitis. Arch Pathol Lab Med. 1990 Apr;114(4):383–387. [PubMed] [Google Scholar]
- Parums D. V., Dunn D. C., Dixon A. K., Mitchinson M. J. Characterization of inflammatory cells in a patient with chronic periaortitis. Am J Cardiovasc Pathol. 1990;3(2):121–129. [PubMed] [Google Scholar]
- Scavalli A. S., Spadaro A., Riccieri V., Ricciuti G. P., Taccari E., Marini M., Zoppini A. Long-term follow-up of low-dose methotrexate therapy in one case of idiopathic retroperitoneal fibrosis. Clin Rheumatol. 1995 Jul;14(4):481–484. doi: 10.1007/BF02207688. [DOI] [PubMed] [Google Scholar]
- Tennant W. G., Hartnell G. G., Baird R. N., Horrocks M. Radiologic investigation of abdominal aortic aneurysm disease: comparison of three modalities in staging and the detection of inflammatory change. J Vasc Surg. 1993 Apr;17(4):703–709. [PubMed] [Google Scholar]
- Uibu Toomas, Oksa Panu, Auvinen Anssi, Honkanen Eero, Metsärinne Kaj, Saha Heikki, Uitti Jukka, Roto Pekka. Asbestos exposure as a risk factor for retroperitoneal fibrosis. Lancet. 2004 May 1;363(9419):1422–1426. doi: 10.1016/S0140-6736(04)16100-X. [DOI] [PubMed] [Google Scholar]
- Vaglio A., Manenti L., Allegri L., Ferrozzi F., Corradi D., Buzio C. ANCA-positive periaortic vasculitis: does it fall within the spectrum of vasculitis? J Intern Med. 2002 Mar;251(3):268–271. doi: 10.1046/j.1365-2796.2002.00948.x. [DOI] [PubMed] [Google Scholar]
- Wagenknecht L. V., Auvert J. Symptoms and diagnosis of retroperitoneal fibrosis. Analysis of 31 cases. Urol Int. 1971;26(3):185–195. doi: 10.1159/000279729. [DOI] [PubMed] [Google Scholar]
- Wagenknecht L. V., Hardy J. C. Value of various treatments for retroperitoneal fibrosis. Eur Urol. 1981;7(4):193–200. doi: 10.1159/000473218. [DOI] [PubMed] [Google Scholar]
- Walker D. I., Bloor K., Williams G., Gillie I. Inflammatory aneurysms of the abdominal aorta. Br J Surg. 1972 Aug;59(8):609–614. doi: 10.1002/bjs.1800590807. [DOI] [PubMed] [Google Scholar]
- von Fritschen U., Malzfeld E., Clasen A., Kortmann H. Inflammatory abdominal aortic aneurysm: A postoperative course of retroperitoneal fibrosis. J Vasc Surg. 1999 Dec;30(6):1090–1098. doi: 10.1016/s0741-5214(99)70048-0. [DOI] [PubMed] [Google Scholar]