Abstract
Background: Perinatal asphyxia is associated with cardiac dysfunction secondary to myocardial ischaemia. Cardiac troponin I (cTnI) is a marker of myocardial necrosis. Raised concentrations in the blood are related to perinatal asphyxia and increased morbidity.
Objective: To assess porcine myocardial damage from enzyme release during hypoxaemia induced global ischaemia, and subsequent resuscitation with ambient air or 100% O2. To investigate whether CO2 level during resuscitation influences myocardial damage.
Design: Newborn piglets (12–36 hours) were exposed to hypoxaemia by ventilation with 8% O2 in nitrogen. When mean arterial blood pressure had fallen to 15 mm Hg, or base excess to < -20 mmol/l, the animals were randomly resuscitated by ventilation with either 21% O2 (group A, n = 29) or 100% O2 (group B, n = 29) for 30 minutes. Afterwards they were observed in ambient air for another 150 minutes. During resuscitation, the two groups were further divided into three subgroups with different CO2 levels.
Analysis: Blood samples were analysed for cTnI, myoglobin, and creatine kinase-myocardial band (CK-MB) at baseline and at the end of the study.
Results: cTnI increased more than 10-fold (p < 0.001) in all the groups. Myoglobin and CK-MB doubled in concentration.
Conclusion: The considerable increase in cTnI indicates seriously affected myocardium. Reoxygenation with 100% oxygen offered no biochemical benefit over ambient air. CK-MB and myoglobin were not reliable markers of myocardial damage. Normoventilation tended to produce better myocardial outcome than hyperventilation or hypoventilation.
Full Text
The Full Text of this article is available as a PDF (270.7 KB).
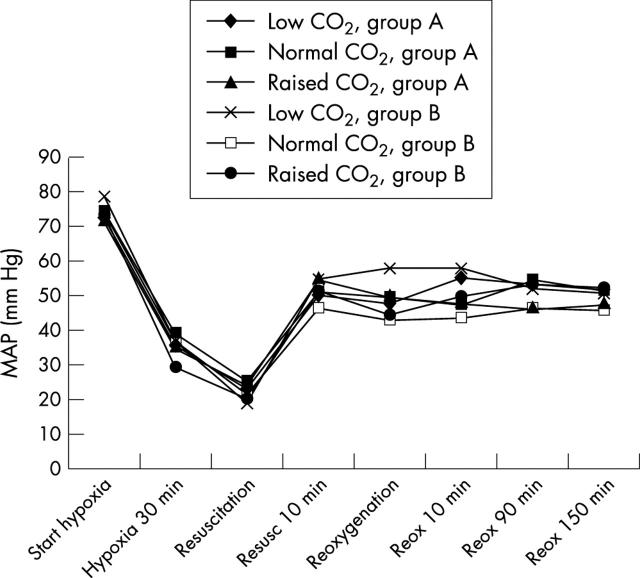
Figure 1 .
Mean arterial pressure (MAP). During hypoxaemia blood pressure decreased significantly, and during resuscitation it rose ending in a plateau about 20 mm Hg lower than at the start of the experiment.
Figure 2 .
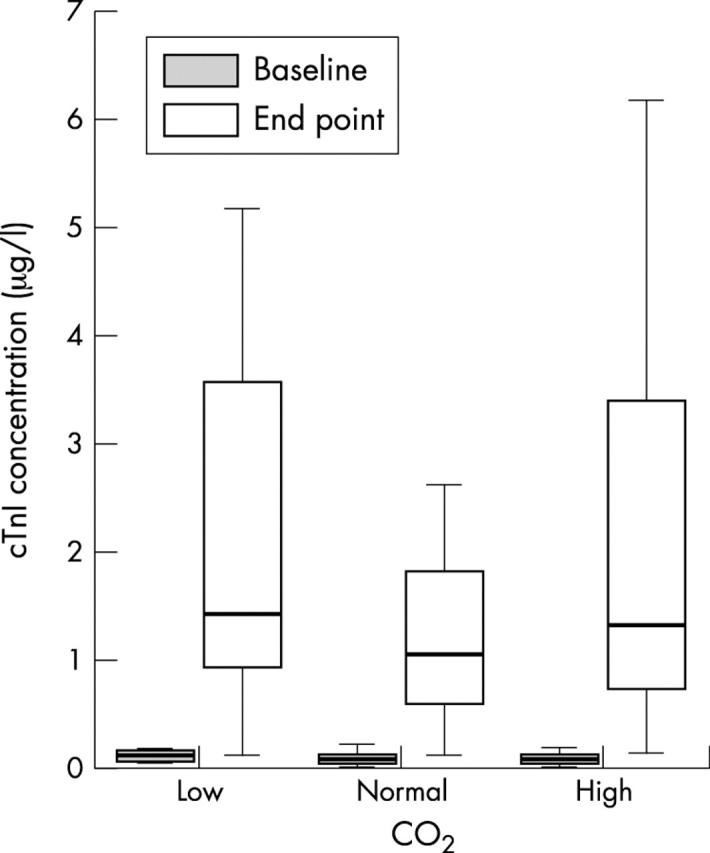
Cardiac troponin I (cTnI) related to CO2. cTnI release was significantly (p < 0.001) increased in all three groups resuscitated by the different ventilatory modes. cTnI release was lower in the normoventilated piglets than the piglets with high or low CO2 (NS).
Figure 3 .
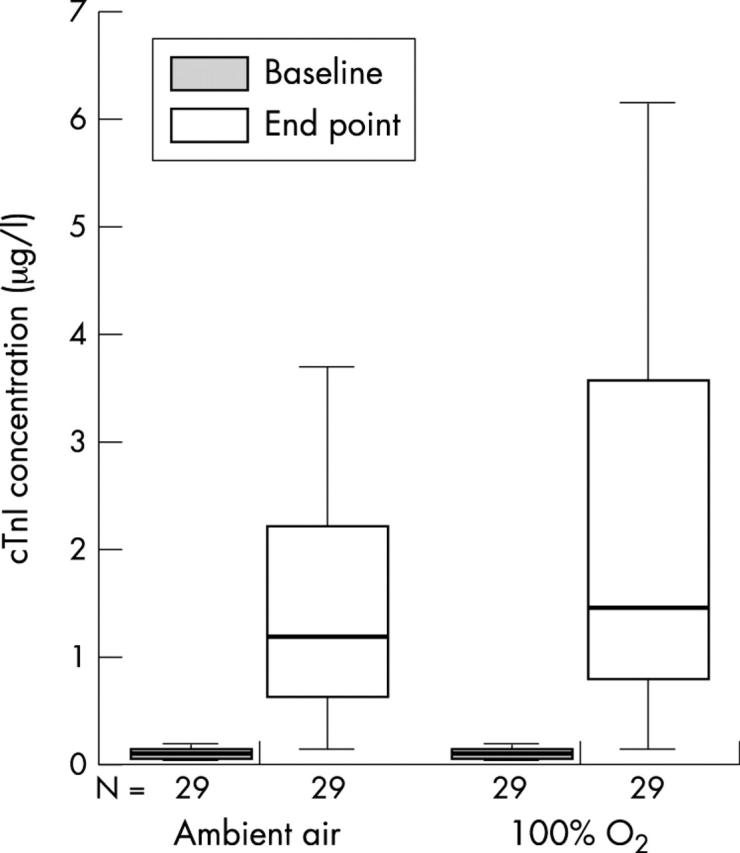
Cardiac troponin I (cTnI) related to O2. There was an increase in cTnI from baseline to end point (p < 0.001) confirming serious cardiac involvement. There were no significant differences between the groups resuscitated with ambient air and 100% O2.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Apple F. S. The specificity of biochemical markers of cardiac damage: a problem solved. Clin Chem Lab Med. 1999 Nov-Dec;37(11-12):1085–1089. doi: 10.1515/CCLM.1999.158. [DOI] [PubMed] [Google Scholar]
- Clark S. J., Newland P., Yoxall C. W., Subhedar N. V. Cardiac troponin T in cord blood. Arch Dis Child Fetal Neonatal Ed. 2001 Jan;84(1):F34–F37. doi: 10.1136/fn.84.1.F34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammerman C., Kaplan M. Ischemia and reperfusion injury. The ultimate pathophysiologic paradox. Clin Perinatol. 1998 Sep;25(3):757–777. [PubMed] [Google Scholar]
- Haney M. F., Johansson G., Häggmark S., Biber B. Heart-lung interactions during positive pressure ventilation: left ventricular pressure-volume momentary response to airway pressure elevation. Acta Anaesthesiol Scand. 2001 Jul;45(6):702–709. doi: 10.1034/j.1399-6576.2001.045006702.x. [DOI] [PubMed] [Google Scholar]
- Hirsch R., Landt Y., Porter S., Canter C. E., Jaffe A. S., Ladenson J. H., Grant J. W., Landt M. Cardiac troponin I in pediatrics: normal values and potential use in the assessment of cardiac injury. J Pediatr. 1997 Jun;130(6):872–877. doi: 10.1016/s0022-3476(97)70271-3. [DOI] [PubMed] [Google Scholar]
- Jaffe A. S., Ravkilde J., Roberts R., Naslund U., Apple F. S., Galvani M., Katus H. It's time for a change to a troponin standard. Circulation. 2000 Sep 12;102(11):1216–1220. doi: 10.1161/01.cir.102.11.1216. [DOI] [PubMed] [Google Scholar]
- Jedeikin R., Makela S. K., Shennan A. T., Rowe R. D., Ellis G. Creatine kinase isoenzymes in serum from cord blood and the blood of healthy full-term infants during the first three postnatal days. Clin Chem. 1982 Feb;28(2):317–322. [PubMed] [Google Scholar]
- Kutzsche S., Ilves P., Kirkeby O. J., Saugstad O. D. Hydrogen peroxide production in leukocytes during cerebral hypoxia and reoxygenation with 100% or 21% oxygen in newborn piglets. Pediatr Res. 2001 Jun;49(6):834–842. doi: 10.1203/00006450-200106000-00020. [DOI] [PubMed] [Google Scholar]
- Lefkowitz William. Oxygen and resuscitation: beyond the myth. Pediatrics. 2002 Mar;109(3):517–519. doi: 10.1542/peds.109.3.517. [DOI] [PubMed] [Google Scholar]
- Levine C. R., Davis J. M. Resuscitation with 100% oxygen: should we change our ways? Pediatr Res. 2001 Oct;50(4):432–432. doi: 10.1203/00006450-200110000-00002. [DOI] [PubMed] [Google Scholar]
- Lipshultz S. E., Rifai N., Sallan S. E., Lipsitz S. R., Dalton V., Sacks D. B., Ottlinger M. E. Predictive value of cardiac troponin T in pediatric patients at risk for myocardial injury. Circulation. 1997 Oct 21;96(8):2641–2648. doi: 10.1161/01.cir.96.8.2641. [DOI] [PubMed] [Google Scholar]
- Medbø S., Yu X. Q., Asberg A., Saugstad O. D. Pulmonary hemodynamics and plasma endothelin-1 during hypoxemia and reoxygenation with room air or 100% oxygen in a piglet model. Pediatr Res. 1998 Dec;44(6):843–849. doi: 10.1203/00006450-199812000-00004. [DOI] [PubMed] [Google Scholar]
- Morin F. C., 3rd Hyperventilation, alkalosis, prostaglandins, and pulmonary circulation of the newborn. J Appl Physiol (1985) 1986 Dec;61(6):2088–2094. doi: 10.1152/jappl.1986.61.6.2088. [DOI] [PubMed] [Google Scholar]
- Panteghini M., Agnoletti G., Pagani F., Spandrio M. Cardiac troponin T in serum as marker for myocardial injury in newborns. Clin Chem. 1997 Aug;43(8 Pt 1):1455–1457. [PubMed] [Google Scholar]
- Ranjit M. S. Cardiac abnormalities in birth asphyxia. Indian J Pediatr. 2000 Mar;67(3 Suppl):S26–S29. [PubMed] [Google Scholar]
- Rootwelt T., Odden J. P., Hall C., Saugstad O. D. Regional blood flow during severe hypoxemia and resuscitation with 21% or 100% O2 in newborn pigs. J Perinat Med. 1996;24(3):227–236. doi: 10.1515/jpme.1996.24.3.227. [DOI] [PubMed] [Google Scholar]
- Rudolph A. M., Yuan S. Response of the pulmonary vasculature to hypoxia and H+ ion concentration changes. J Clin Invest. 1966 Mar;45(3):399–411. doi: 10.1172/JCI105355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saugstad O. D. Is oxygen more toxic than currently believed? Pediatrics. 2001 Nov;108(5):1203–1205. doi: 10.1542/peds.108.5.1203. [DOI] [PubMed] [Google Scholar]
- Saugstad O. D. Role of xanthine oxidase and its inhibitor in hypoxia: reoxygenation injury. Pediatrics. 1996 Jul;98(1):103–107. [PubMed] [Google Scholar]
- Soldin S. J., Murthy J. N., Agarwalla P. K., Ojeifo O., Chea J. Pediatric reference ranges for creatine kinase, CKMB, Troponin I, iron, and cortisol. Clin Biochem. 1999 Feb;32(1):77–80. doi: 10.1016/s0009-9120(98)00084-8. [DOI] [PubMed] [Google Scholar]
- Strømme J. H., Rolstad O. J., Mangschau A. Troponiner og andre nye biokjemiske hjertemarkører--tid for et skifte. Tidsskr Nor Laegeforen. 2000 Jun 20;120(16):1863–1869. [PubMed] [Google Scholar]
- Tapia-Rombo C. A., Carpio-Hernández J. C., Salazar-Acuña A. H., Alvarez-Vázquez E., Mendoza-Zanella R. M., Pérez-Olea V., Rosas-Fernández C. Detection of transitory myocardial ischemia secondary to perinatal asphyxia. Arch Med Res. 2000 Jul-Aug;31(4):377–383. doi: 10.1016/s0188-4409(00)00088-6. [DOI] [PubMed] [Google Scholar]
- Vento M., Asensi M., Sastre J., García-Sala F., Pallardó F. V., Viña J. Resuscitation with room air instead of 100% oxygen prevents oxidative stress in moderately asphyxiated term neonates. Pediatrics. 2001 Apr;107(4):642–647. doi: 10.1542/peds.107.4.642. [DOI] [PubMed] [Google Scholar]
- Vento M., Asensi M., Sastre J., García-Sala F., Viña J. Six years of experience with the use of room air for the resuscitation of asphyxiated newly born term infants. Biol Neonate. 2001;79(3-4):261–267. doi: 10.1159/000047103. [DOI] [PubMed] [Google Scholar]
- Walther F. J., Siassi B., Ramadan N. A., Wu P. Y. Cardiac output in newborn infants with transient myocardial dysfunction. J Pediatr. 1985 Nov;107(5):781–785. doi: 10.1016/s0022-3476(85)80417-0. [DOI] [PubMed] [Google Scholar]
- Williams C. E., Mallard C., Tan W., Gluckman P. D. Pathophysiology of perinatal asphyxia. Clin Perinatol. 1993 Jun;20(2):305–325. [PubMed] [Google Scholar]