Abstract
Background: Multiorgan dysfunction (MOD) is one of four consensus based criteria for the diagnosis of intrapartum asphyxia. The theoretical concept behind MOD is the diving reflex (conservation of blood flow to vital organs at the cost of non-vital organs).
Objectives: To assess the patterns of involvement of each major organ/system and combinations of involvement in infants with post-asphyxial hypoxic-ischaemic encephalopathy (HIE), and to describe this in relation to long term outcome.
Design: Retrospective cohort study.
Setting: Regional tertiary neonatal intensive care unit at the Hospital for Sick Children, Toronto, Canada.
Patients: Term neonates with post-intrapartal asphyxial HIE assessed for kidney, cardiovascular system, lung, and liver function.
Outcome: Death and presence or absence of severe neurodevelopmental disability.
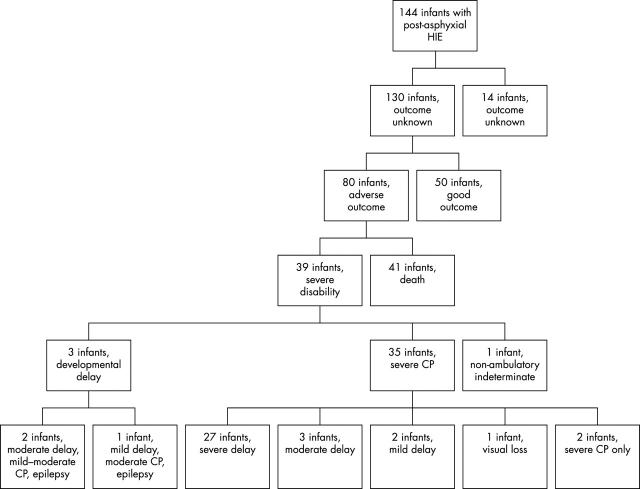
Results: Out of 130 of 144 eligible infants with outcome data, 80 (62%) had severe adverse outcome and 50 (38%) had good outcome. All infants had evidence of MOD (at least one organ dysfunction in addition to HIE). Renal, cardiovascular, pulmonary, and hepatic dysfunction was present in 58–88% of infants with good outcome and 64–86% of infants with adverse outcome.
Conclusions: MOD was present in all the infants with severe post-asphyxial HIE. However, there was no association between MOD and outcome in these infants. No relation between individual or combinations of organ involvements and long term outcomes was observed.
Full Text
The Full Text of this article is available as a PDF (236.4 KB).
Figure 1 .
Outcome data of the study cohort. CP, Cerebral palsy.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bocking A. D., Gagnon R., White S. E., Homan J., Milne K. M., Richardson B. S. Circulatory responses to prolonged hypoxemia in fetal sheep. Am J Obstet Gynecol. 1988 Dec;159(6):1418–1424. doi: 10.1016/0002-9378(88)90567-4. [DOI] [PubMed] [Google Scholar]
- Bueva A., Guignard J. P. Renal function in preterm neonates. Pediatr Res. 1994 Nov;36(5):572–577. doi: 10.1203/00006450-199411000-00005. [DOI] [PubMed] [Google Scholar]
- Chauhan Suneet P., Magann Everett F., Morrison John C. Neonatal organ system injury in acute birth asphyxia sufficient to result in neonatal encephalopathy. Obstet Gynecol. 2003 Jan;101(1):203–204. doi: 10.1016/s0029-7844(02)02577-2. [DOI] [PubMed] [Google Scholar]
- Gordjani N., Burghard R., Leititis J. U., Brandis M. Serum creatinine and creatinine clearance in healthy neonates and prematures during the first 10 days of life. Eur J Pediatr. 1988 Nov;148(2):143–145. doi: 10.1007/BF00445923. [DOI] [PubMed] [Google Scholar]
- Hankins Gary D. V., Koen Sophia, Gei Alfredo F., Lopez Suzanne M., Van Hook James W., Anderson Garland D. Neonatal organ system injury in acute birth asphyxia sufficient to result in neonatal encephalopathy. Obstet Gynecol. 2002 May;99(5 Pt 1):688–691. doi: 10.1016/s0029-7844(02)01959-2. [DOI] [PubMed] [Google Scholar]
- Hellström-Westas L., Rosén I., Svenningsen N. W. Predictive value of early continuous amplitude integrated EEG recordings on outcome after severe birth asphyxia in full term infants. Arch Dis Child Fetal Neonatal Ed. 1995 Jan;72(1):F34–F38. doi: 10.1136/fn.72.1.f34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jedeikin R., Primhak A., Shennan A. T., Swyer P. R., Rowe R. D. Serial electrocardiographic changes in healthy and stressed neonates. Arch Dis Child. 1983 Aug;58(8):605–611. doi: 10.1136/adc.58.8.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen A., Garnier Y., Berger R. Dynamics of fetal circulatory responses to hypoxia and asphyxia. Eur J Obstet Gynecol Reprod Biol. 1999 Jun;84(2):155–172. doi: 10.1016/s0301-2115(98)00325-x. [DOI] [PubMed] [Google Scholar]
- Lackmann G. M., Töllner U. The predictive value of elevation in specific serum enzymes for subsequent development of hypoxic-ischemic encephalopathy or intraventricular hemorrhage in full-term and premature asphyxiated newborns. Neuropediatrics. 1995 Aug;26(4):192–198. doi: 10.1055/s-2007-979752. [DOI] [PubMed] [Google Scholar]
- MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: international consensus statement. BMJ. 1999 Oct 16;319(7216):1054–1059. doi: 10.1136/bmj.319.7216.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín-Ancel A., García-Alix A., Gayá F., Cabañas F., Burgueros M., Quero J. Multiple organ involvement in perinatal asphyxia. J Pediatr. 1995 Nov;127(5):786–793. doi: 10.1016/s0022-3476(95)70174-5. [DOI] [PubMed] [Google Scholar]
- Peeters L. L., Sheldon R. E., Jones M. D., Jr, Makowski E. L., Meschia G. Blood flow to fetal organs as a function of arterial oxygen content. Am J Obstet Gynecol. 1979 Nov 1;135(5):637–646. doi: 10.1016/s0002-9378(16)32989-1. [DOI] [PubMed] [Google Scholar]
- Perlman J. M., Tack E. D., Martin T., Shackelford G., Amon E. Acute systemic organ injury in term infants after asphyxia. Am J Dis Child. 1989 May;143(5):617–620. doi: 10.1001/archpedi.1989.02150170119037. [DOI] [PubMed] [Google Scholar]
- Perlman J. M., Tack E. D. Renal injury in the asphyxiated newborn infant: relationship to neurologic outcome. J Pediatr. 1988 Nov;113(5):875–879. doi: 10.1016/s0022-3476(88)80023-4. [DOI] [PubMed] [Google Scholar]
- Phelan J. P., Ahn M. O., Korst L., Martin G. I., Wang Y. M. Intrapartum fetal asphyxial brain injury with absent multiorgan system dysfunction. J Matern Fetal Med. 1998 Jan-Feb;7(1):19–22. doi: 10.1002/(SICI)1520-6661(199801/02)7:1<19::AID-MFM5>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- Primhak R. A., Jedeikin R., Ellis G., Makela S. K., Gillan J. E., Swyer P. R., Rowe R. D. Myocardial ischaemia in asphyxia neonatorum. Electrocardiographic, enzymatic and histological correlations. Acta Paediatr Scand. 1985 Jul;74(4):595–600. doi: 10.1111/j.1651-2227.1985.tb11036.x. [DOI] [PubMed] [Google Scholar]
- Sacks H., Chalmers T. C., Smith H., Jr Randomized versus historical controls for clinical trials. Am J Med. 1982 Feb;72(2):233–240. doi: 10.1016/0002-9343(82)90815-4. [DOI] [PubMed] [Google Scholar]
- Shankaran S., Woldt E., Koepke T., Bedard M. P., Nandyal R. Acute neonatal morbidity and long-term central nervous system sequelae of perinatal asphyxia in term infants. Early Hum Dev. 1991 May;25(2):135–148. doi: 10.1016/0378-3782(91)90191-5. [DOI] [PubMed] [Google Scholar]
- Sheldon R. E., Peeters L. L., Jones M. D., Jr, Makowski E. L., Meschia G. Redistribution of cardiac output and oxygen delivery in the hypoxemic fetal lamb. Am J Obstet Gynecol. 1979 Dec 15;135(8):1071–1078. doi: 10.1016/0002-9378(79)90739-7. [DOI] [PubMed] [Google Scholar]
- Volpe J. J. Neonatal seizures: current concepts and revised classification. Pediatrics. 1989 Sep;84(3):422–428. [PubMed] [Google Scholar]
- Zanardo V., Bondio M., Perini G., Temporin G. F. Serum glutamic-oxaloacetic transaminase and glutamic-pyruvic transaminase activity in premature and full-term asphyxiated newborns. Biol Neonate. 1985;47(2):61–69. doi: 10.1159/000242092. [DOI] [PubMed] [Google Scholar]