Abstract
Many fungi that cause invasive disease invade host epithelial cells during mucosal and respiratory infection, and subsequently invade endothelial cells during hematogenous infection. Most fungi invade these normally non-phagocytic host cells by inducing their own uptake. Candida albicans hyphae interact with endothelial cells in vitro by binding to N-cadherin on the endothelial cell surface. This binding induces rearrangement of endothelial cell microfilaments, which results in the endocytosis of the organism. The capsule of Cryptococcus neoformans is composed of glucuronoxylomannan, which binds specifically to brain endothelial cells, and appears to mediate both adherence and induction of endocytosis. The mechanisms by which other fungal pathogens induce their own uptake are largely unknown. Some angioinvasive fungi, such as Aspergillus species and the Zygomycetes, invade endothelial cells from the abluminal surface during the initiation of invasive disease, and subsequently invade the luminal surface of endothelial cells during hematogenous dissemination. Invasion of normally non-phagocytic host cells has different consequences, depending on the type of invading fungus. Aspergillus fumigatus blocks apoptosis of pulmonary epithelial cells, whereas Paracoccidioides brasiliensis induces apoptosis of epithelial cells. This review summarizes the mechanisms by which diverse fungal pathogens invade normally non-phagocytic host cells and discusses gaps in our knowledge that provide opportunities for future research.
Introduction
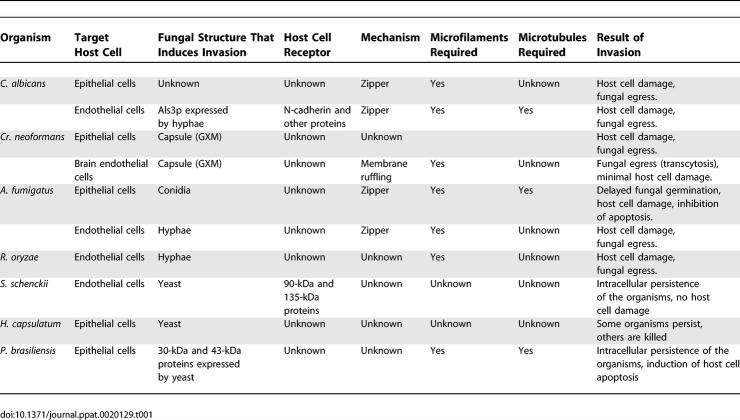
Pathogenic fungi interact with a variety of host cells during the induction of disease. To cross tissue planes and cause invasive disease, these organisms must invade normally non-phagocytic host cells such as epithelial cells and endothelial cells. The mechanisms by which bacteria invade these cells have been a subject of intense investigation for many years (reviewed in [1]). Since the 1990s researchers have been investigating the processes by which pathogenic fungi invade mammalian cells. This review summarizes the results of these investigations (Table 1) and describes gaps in our knowledge of fungal invasion. For the purpose of this article, we will use the term invasion to indicate the penetration of all or part of a fungus into a normally non-phagocytic host cell.
Table 1.
Summary of the Invasion Mechanisms of the Different Fungi and Their Host Cell Targets
Candida Species
Epithelial cell invasion.
Fungi of the genus Candida are part of the normal human flora and typically grow on mucosal surfaces, such as those in the mouth and vagina. They can cause a variety of different superficial diseases, including oropharyngeal, esophageal, vulvovaginal, and cutaneous candidiasis. A common histopathologic finding in these diseases is the presence of fungal cells within epithelial cells. For example, intraepithelial fungi have been observed in specimens from humans with oropharyngeal candidiasis [2–5], vulvovaginal candidiasis [6], and cutaneous candidiasis [7]. It is postulated that the intracellular location of the organisms protects them from the host immune response [6].
C. albicans is the predominant cause of virtually all types of candidiasis. Thus, the interactions of this organism with epithelial cells have been studied in the greatest detail. A key virulence factor of C. albicans is its capacity to interconvert between an ovoid-shaped blastospore and a filamentous hypha [8,9]. Ultrastructural studies of specimens from humans and experimental animals have suggested that C. albicans hyphae are the invasive form of the organism, because hyphae are found within epithelial cells, whereas blastospores are generally found either on the epithelial cell surface or between these cells [7,10].
Two different mechanisms of oral epithelial cell invasion have been described. One mechanism is the production of lytic enzymes, such as secreted aspartyl proteinases (SAPs), by the organism. It has been proposed that these enzymes digest the surface of the epithelial cell and thereby provide an entrance into the cell. SAPs may be especially important for the invasion of keratinized epithelial cells [10,11]. For example, C. albicans blastospores induce depressions in the surface of corneocytes in mice with cutaneous candidiasis, but pepstatin A, an inhibitor of aspartyl proteinases, reduces the formation of these depressions [10]. In fact, C. albicans mutants containing disruptions of various SAP genes have a reduced capacity to damage vaginal and oral epithelial cells in vitro [12,13]. As epithelial cell invasion is likely a precursor of epithelial cell damage, it is possible that the reduced damage caused by the sapΔ/sapΔ mutants is due in part to decreased epithelial cell invasion. Consistent with the in vitro results, many of these sapΔ/sapΔ mutant strains have attenuated virulence in the rat model of vaginal candidiasis [14]. It is also possible that C. albicans SAPs play a role in tissue penetration by facilitating the passage of the organism between host cells. In this regard, the SAPs of C. albicans appear to be functionally similar to the cysteine proteases of Porphyromonas gingivalis and group A Streptococcus, which enable these bacteria to invade and damage epithelial cells [15,16].
Another mechanism of candidal invasion of epithelial cells is the induction of epithelial cell endocytosis. It has been observed that C. albicans induces epithelial cells to produce pseudopods that surround the organism and pull it into the cell. The formation of these pseudopods is accompanied by the accumulation of epithelial cell microfilaments around the organism. These microfilaments are required for endocytosis because disrupting them with cytochalasin D blocks the uptake of C. albicans [17].
A variety of human epithelial cell lines are able to endocytose C. albicans, including HeLa cells, HET1-A esophageal cells, FaDu pharyngeal cells, and OKF6/TERT-2 oral epithelial cells [17–19]. However, the formation of pseudopods by epithelial cells is difficult to observe in vivo. Thus, the relative contribution of endocytosis versus local proteolytic digestion to the invasion of epithelial cells by C. albicans in vivo remains to be determined. However, it is clear that secreted proteases are not necessary for C. albicans to induce its own endocytosis by epithelial cells in vitro, because killed organisms are endocytosed as avidly as are live organisms [17].
Although both yeast and hypha phase organisms can induce endocytosis, hyphae are more efficient at stimulating this process. For example, an efg1Δ/efg1Δ mutant that does not germinate on oral epithelial cells has a significantly reduced capacity to induce endocytosis [17]. The greater capacity of hyphae to induce endocytosis compared with that of blastospores suggests that hyphae express specific invasin-like molecules on their surface that bind to one or more epithelial cell receptors and induce endocytosis. However, the identities of these candidal invasins and their epithelial receptors are unknown at this time.
Two different signal transduction mutants of C. albicans have been discovered to have a reduced capacity to induce endocytosis by oral epithelial cells, even though they have little or no defects in hypha formation. These mutants lack either Tpk2, which is a catalytic subunit of protein kinase A, or Cka2, which is a catalytic subunit of protein kinase CK2 [17,20]. However, it is not known whether Tpk1 and Cka2 govern the expression of the same or different epithelial cell invasins. A C. albicans mutant that lacks the glycosylphosphatidylinositol-linked protein Ecm33 also has a reduced capacity to invade oral epithelial cells [21]. Ecm33 is likely expressed on the fungal surface and is required for normal cell wall assembly [22,23]. The heterologous expression of ECM33 in Saccharomyces cerevisiae does not result in enhanced endocytosis of this organism, suggesting that Ecm33 itself does not mediate epithelial cell invasion. Also, the ecm33Δ/ecm33Δ mutant has aberrant expression of at least one other cell surface protein. Therefore, it is likely that the invasion defect of the ecm33Δ/ecm33Δ mutant is due to abnormal function and expression of one or more other cell surface proteins.
Endothelial cell invasion.
In susceptible patients, Candida species can enter the bloodstream either by translocation across the gastrointestinal mucosa or via an intravascular catheter. To escape from the bloodstream and invade target organs, these organisms must cross the endothelial cell lining of the blood vessels. There are three general mechanisms by which this process can occur. The first mechanism is the phagocytosis of the organism by a leukocyte, which then diapedeses across the endothelial cell lining of the blood vessel. Indeed, Candida species have been observed inside leukocytes of patients with candidemia [24]. However, there must be other mechanisms by which these organisms can escape from the bloodstream, because disseminated candidiasis can occur in patients with profound leucopenia. A second mechanism is the passage of the organism between the endothelial cells. Such a process would likely occur in vascular beds of organs such as the kidney, where the endothelial cell lining of the blood vessels is fenestrated. A third mechanism is the endocytosis of the organism by endothelial cells. This mechanism clearly occurs in vitro, and has been the focus of multiple investigations [21,25–33].
Researchers have observed that C. albicans is endocytosed by human umbilical vein endothelial cells [26–28], endothelial cells in porcine vascular explants [25], and human brain microvascular endothelial cells [32,34]. In most cases, the endothelial cells produce pseudopods that engulf the organism. Endocytosis of C. albicans requires intact endothelial cell microfilaments and microtubules [27]; it is also governed in part by the tyrosine phosphorylation of endothelial cell proteins [31]. This process is passive on the part of the organism because killed organisms are able to induce endocytosis similarly to live organisms [27,29]. C. albicans hyphae induce endocytosis by human umbilical vein endothelial cells much more efficiently than do blastospores [29].
The results of several studies have led to the development of a model of how C. albicans hyphae induce their own endocytosis by human umbilical vein endothelial cells in vitro. In this model, C. albicans hyphae express an invasin-like protein, Als3, which can bind to N-cadherin and other proteins on the endothelial cell surface (Q. Phan, C. Myers, Y. Fu, D. Sheppard, M. Yeaman, et al., unpublished data). Binding to these surface proteins induces the phosphorylation of at least two different endothelial cell proteins, which in turn causes the rearrangement of the endothelial cell microfilaments to produce pseudopods and initiate endocytosis [19,30,31,35]. The N-terminal region of Als3 contains the ligand-binding domain. This region is predicted to share structural homology with the invasin protein of Yersinia pseudotuberculsosis [35]. However, this method of host cell invasion by C. albicans is reminiscent of that induced by internalin A of Listeria monocytogenes, which induces epithelial cell endocytosis by binding to E-cadherin [36]. Many details of this model have yet to be elucidated, including the identities of the endothelial cell surface proteins other than N-cadherin that are bound by C. albicans, and the identities of the proteins that are tyrosine phosphorylated during the endocytosis of C. albicans. It also is not yet known whether the binding of Als3 to N-cadherin mediates endocytosis of C. albicans by endothelial cells in vivo.
It is clear that C. albicans interacts differently with endothelial cells from different vascular beds. For example, although human umbilical vein endothelial cells preferentially endocytose hyphae, blastospores have been found to be avidly endocytosed by porcine endothelial cells and human brain microvascular endothelial cells in vitro [25,32,34]. In addition, endothelial cells may act differently in vitro than in vivo. For example, Saville et al. [9] investigated the role of hypha formation in C. albicans virulence by constructing a strain of C. albicans in which hypha formation was regulated by the presence of tetracycline. They found that the fungal burden of the kidneys, spleens, and brains of mice infected intravenously with organisms that grew only as blastospores was at least as high as that of mice infected with organisms that formed hyphae. Thus, hypha formation does not appear to be necessary for C. albicans to escape from the bloodstream and invade target organs in immunocompetent mice. Furthermore, some species of Candida, such as Candida glabrata, are incapable of forming hyphae, yet are able to cause hematogenously disseminated candidiasis in humans. How blastospores of Candida species are able cross the endothelial cell lining of the vasculature is currently unknown.
Cryptococcus neoformans
Epithelial cell invasion.
Cryptococcosis develops when a susceptible host inhales Cr. neoformans. Once inside the lungs, the organism penetrates the alveolus. Cr. neoformans adheres to and is internalized by pulmonary epithelial cells in vitro [37–39]. However, relatively little is known about its mechanisms of epithelial cell invasion. A key virulence factor of Cr. neoformans is the presence of a capsule, which is composed of glucuronoxylomannan (GXM). This capsule inhibits phagocytosis of Cr. neoformans by leukocytes. Interestingly, type II pneumocytes apparently have a receptor for GXM. These cells can internalize both unencapsulated and encapsulated strains of Cr. neoformans, as well as purfied GXM [38,39]. Furthermore, adherence of encapsulated organisms to these epithelial cells can be inhibited by GXM. However, the identity of the GXM receptor on pulmonary epithelial cells remains to be determined.
Endothelial cell invasion.
To cause meningitis, Cr. neoformans must enter the bloodstream, and then cross the microvascular endothelial cells that form the blood–brain barrier. Two different studies have found Cr. neoformans cells inside of brain endothelial cells in mice infected intravenously with live organisms [40,41]. Thus, Cr. neoformans can cross the endothelial cell lining of the cerebral blood vessels by a transcellular mechanism. The interaction of Cr. neoformans with endothelial cells has also been analyzed in vitro. Both encapsulated and unencapsulated organisms are able to induce their own endocytosis by brain microvascular endothelial cells [41,42]. The organisms induce membrane ruffling and projection of microvilli that surround the organisms and pull them into the cell. This membrane ruffling is induced by rearrangement of the endothelial cell microfilaments; this rearrangement is likely stimulated by the dephosphorylation of cofilin [42].
Once Cr. neoformans is internalized by a brain microvascular endothelial cell, it can exit through the abluminal surface of the cell. Thus, these in vitro findings support the conclusion of the above animal studies that Cr. neoformans can cross brain microvascular endothelial cells by the process of transcytosis. Interestingly, although there is a suggestion that the tight junctions between the brain microvascular endothelial cells are weakened by the transcytosis of Cr. neoformans, there is no reduction in transendothelial cell electrical resistance. Therefore, the transcytosis process appears to cause minimal endothelial cell damage. [42].
Although both encapsulated and unencapsulated strains can transcytose across brain microvascular endothelial cells, studies with isogenic mutants suggest that the presence of a capsule enhances initial adherence to these endothelial cells, as well as the rate of transcytosis [42,43]. The presence of a capsule has a completely different effect on the interactions of Cr. neoformans with human umbilical vein endothelial cells. Ibrahim et al. [44] found that these endothelial cells can endocytose unencapsulated Cr. neoformans, but not encapsulated strains. Moreover, efficient endocytosis of the uncapsulated strain of Cr. neoformans by human umbilical vein endothelial cells requires the presence of a heat-labile serum factor. Therefore, it is likely that the tropism of Cr. neoformans for the brain is due in part to the unique ability of brain endothelial cells to bind and endocytose encapsulated organisms. Strains of Escherichia coli that cause meningitis in neonates also have tropism for the central nervous system. It has been found that microvascular brain endothelial cells express a protein called gp96 that is bound by the E. coli OmpA. Endothelial cells from other vascular beds do not express this protein, and thus are invaded poorly by E. coli in vitro [45]. Based on these results, it seems likely that the Cr. neoformans capsule is bound by a receptor that is expressed most highly by brain endothelial cells.
Coenjaerts et al. [46] used serial analysis of gene expression to identify Cr. neoformans genes that were up-regulated in response to endocytosis by human umbilical vein endothelial cells. They determined that SKN7, which encodes the effector element of a two-component signaling system, was up-regulated by 4.5-fold in Cr. neoformans cells that were endocytosed by endothelial cells. Interestingly, a skn7Δ deletion mutant appeared to be killed by the umbilical vein endothelial cells after it had been endocytosed. However, although this strain was hypersensitive to hydrogen peroxide, it was not more susceptible to killing by either neutrophils or peripheral blood mononuclear cells. The skn7Δ deletion mutant did have attenuated virulence in mice inoculated intravenously, though. These results suggest that endothelial cells from systemic blood vessels may actually be able to kill Cr. neoformans. The role of Skn7 in governing the response of Cr. neoformans to brain endothelial cells is unknown at this time.
Aspergillus fumigatus
Invasion of epithelial cells.
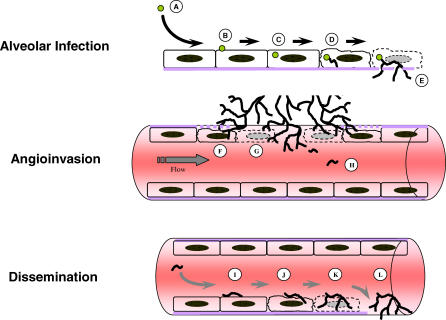
Invasive aspergillosis is initiated by inhalation of conidia, which, by virtue of their small size, are deposited in the alveoli. These conidia subsequently invade the epithelial cell lining of the alveoli (Figure 1). A. fumigatus causes the majority of cases of invasive aspergillosis [47], and the interactions of this organism with host cells have therefore been studied in greater detail than other Aspergillus species. A. fumigatus conidia and hyphae have been found to induce their own endocytosis by type II pneumocytes [48–50]. Conidia can also be endocytosed by tracheal epithelial cells, but at a lower efficiency than that of type II pneumocytes [49]. Contact with A. fumigatus conidia induces type II pneumocytes to produce pseudopods that engulf the organism [49]. The formation of these pseudopods requires intact host cell microfilaments and microtubules. Once the conidia are internalized by type II pneumocytes, they traffic to late endosomes/lysosomes, as indicated by the presence of lysosomal-associated protein 1 and cathepsin D in these vacuoles. Approximately half of the vacuoles containing conidia are acidic [51].
Figure 1. Model of Aspergillus fumigatus Interactions with Pulmonary Epithelial Cells and Vascular Endothelial Cells during Angioinvasion and Dissemination.
Invasive aspergillosis occurs via the following steps: infection is initiated by the inhalation of small numbers of airborne conidia (A), which adhere to pulmonary epithelial cells (B), and are rapidly endocytosed (C). Within the epithelial cells, the conidia germinate to form hyphae (D), which grow by apical extension and escape from the epithelial cells (E). Next, emergent hyphae penetrate the abluminal surface of endothelial cells (F) and induce endothelial cell damage (G). Hyphal fragments disseminate hematogenously (H) and adhere to the luminal endothelial cell surface (I) before invading these cells (J). Luminal invasion results in endothelial cell damage (K) and extravascular invasion of deep organs (L). Steps (A–E) occur in the pulmonary alveoli, (F–H) in the pulmonary blood vessels, and (I–L) in the systemic blood vessels.
The endocytosis of A. fumigatus conidia by type II pneumocytes has significant effects on both the organism and the host cell. Germination of the endocytosed conidia is significantly delayed compared with conidia that are grown in the absence of pneumocytes. However, many of the conidia eventually germinate, and the resultant hyphae can escape from the endosome and penetrate the plasma membrane of the pneumocyte. Remarkably, this process causes virtually no detectable damage to the host cell [51]. In fact, A. fumigatus conidia have been found to suppress apoptosis of type II pneumocytes induced by either tumor necrosis factor α (TNF-α) or staurosporine. Inhibition of apoptosis is an active process on the part of the conidia because killed conidia do not inhibit pneumocyte apoptosis, even though they are endocytosed [52]. The mechanism by which conidia inhibit pneumocyte apoptosis is currently unknown. However, it is likely that ability of A. fumigatus to use viable type II pneumocytes as a sanctuary contributes to the virulence of this organism.
Invasion of endothelial cells.
Invasion of the blood vessels is a key feature of invasive aspergillosis [53,54]. This angioinvasion contributes to tissue necrosis at the foci of infection and reduces the penetration of leukocytes and antifungal drugs to these sites. There are two types of angioinvasion that occur during invasive aspergillosis (Figure 1); the first type occurs in the lungs. After A. fumigatus hyphae have penetrated the pulmonary epithelium, they invade the vasculature by passing from the abluminal to the luminal surface of the pulmonary endothelial cells. This process results in disruption of the endothelial cell monolayer at the focus of angioinvasion and intravascular thrombosis. This type of angioinvasion is most common. The second type of angioinvasion occurs in profoundly immunocompromised patients. In these patients, hyphae that have entered the bloodstream break off, and the resultant hyphal fragments disseminate hematogenously throughout the body. For these hyphal fragments to invade the target organs, they must penetrate the luminal surface of the vascular endothelial cells.
Endothelial cells are polarized.
For example, unstimulated endothelial cells constitutively secrete 3-fold more von Willebrand factor via their abluminal surface than via their luminal surface. When these cells are stimulated with TNF-α, virtually all of the von Willebrand factor is secreted luminally [55]. Also, endothelial cells exhibit a greater increase in permeability when TNF-α is applied to their luminal surface compared with their abluminal surface [56]. Therefore, it is likely that endothelial cells respond differently to A. fumigatus when it invades their abluminal surface than when it invades their luminal surface.
To date, all of the published studies of the interactions of A. fumigatus with endothelial cells have focused on luminal infection. A. fumigatus conidia and hyphae can invade the luminal surface of endothelial cells by inducing their own endocytosis in vitro [49,57,58]. The significance of conidial invasion of endothelial cells is uncertain because it is highly probable that the organism has formed hyphae by the time it invades endothelial cells in vivo [53]. Hyphae are endocytosed by the luminal surface of human umbilical vein endothelial cells more slowly than are conidia. Endocytosis of hyphae causes endothelial cell damage as well as up-regulation of endothelial cell–tissue factor expression [57]. It is likely that the expression tissue factor contributes to the vascular thrombosis at sites of A. fumigatus angioinvasion.
Recently, we compared the response of endothelial cells to A. fumigatus hyphae when they were infected via their luminal surface with the response of cells to hyphae infected via their abluminal surface in vitro. The hyphae invaded both surfaces of the endothelial cells. Luminal invasion caused greater endothelial cell damage, yet induced less expression of mRNA for E-selectin, TNF-α, interleukin-8, and tissue factor (Y. Kamai, A. Lossinsky, D. Sheppard, and S. Filler, unpublished data). These results suggest that the pathogenesis of angioinvasion during locally invasive aspergillosis may be different from that of hematogenously disseminated aspergillosis. The A. fumigatus invasins and endothelial cell receptors that mediate invasion of the luminal versus abluminal surface of endothelial cells remain to be identified.
Other Fungi
Zygomycetes.
Zygomycosis, also known as mucormycosis, is caused by fungi of the class Zygomycetes. This disease is usually initiated by inhalation, and the fungus is believed to penetrate the epithelial cell lining of the nasopharynx or pulmonary alveoli [59]. Like invasive aspergillosis, zygomycosis is characterized by angioinvasion from the abluminal to the luminal surface of the blood vessels [60]. The Zygomycetes occasionally cause hematogenously disseminated disease. Despite the prominence of angioinvasion in the pathogenesis of zygomycosis, there has only been one report of the interactions of a Zygomycete with endothelial cells. Ibrahim et al. [61] examined the endothelial cell interactions of Rhizopus oryzae, the most common cause of zygomycosis. They found that both live and killed R. oryzae hyphae were endocytosed by human umbilical vein endothelial cells. The endocytosis of live hyphae caused significant endothelial cell damage. Interestingly, killed hyphae induced a similar extent of endothelial cell damage, suggesting that a factor associated with the fungal cell wall is toxic to these cells. Damage to endothelial cells results in exposure of vascular smooth muscle cells, which can release large quantities of tissue factor and cause intravascular thrombosis [62]. Thus, induction of endothelial cell damage during angioinvasion may contribute to thrombosis and tissue infarction, which are characteristic of mucormycosis.
Sporothrix schenckii.
Sporotrichosis is caused by S. schenckii [63] and primarily involves the skin and lymphatic channels, but hematogenous dissemination may also occur [63,64]. During hematogenous dissemination, it is likely that the organism penetrates the endothelial cell lining of the vasculature to invade the deep tissues. S. schenckii has been found to invade human umbilical vein endothelial cells in vitro by inducing its own endocytosis [65]. Unlike other pathogens, endothelial cell invasion does not result in detectable endothelial cell damage. Binding of S. schenckii to endothelial cells is enhanced when the host cells are stimulated with interleukin-1β, indicating that this organism binds to an inducible receptor on the endothelial cell surface [65]. This situation is similar to that which has been seen with Streptococcus pneumoniae, which binds to the platelet-activating factor receptor. This receptor is up-regulated on the surface of activated endothelial cells [66].
Histoplasma capsulatum.
Pulmonary or disseminated histoplasmosis is initiated by the inhalation of H. capsulatum. After initial infection, the organism can persist in the host for years and reactivate when immunity wanes [67]. It is possible that H. capsulatum survives for long periods of time in more than one type of host cell. For example, the organism is known to persist in macrophages in vivo and in vitro [68]. H. capsulatum yeast can also survive after being endocytosed by hamster tracheal epithelial cells in vitro [69,70]. Whether this organism persists in epithelial cells in vivo is currently unknown. Some of the yeast that are endocytosed by epithelial cells contain α-(1,3)-glucan in their cell walls, whereas others do not. The yeast with α-(1,3)-glucan appear to be killed by the epithelial cells. It remains to be determined whether this killing is mediated by epithelial cell–derived reactive oxygen intermediates and/or defensins. Other yeast spontaneously lose the ability to produce α-(1,3)-glucan and are able to persist in the epithelial cells; these persistent organisms may serve as a reservoir for latent infection [69,70].
Paracoccidioides brasiliensis.
Infection with P. brasiliensis usually begins following inhalation of conidia. These conidia transform into yeast, which cause both pulmonary and disseminated disease [71]. The yeast have been visualized within the alveolar walls and macrophages during experimental pulmonary infection in mice [72]. In vitro investigations of the interactions of P. brasiliensis with normally non-phagocytic host cells have mainly used African green monkey kidney cells (Vero cells) [73–75]. However, there is one report of the interactions of this organism with a type II pneumocyte cell line [74]: P. brasiliensis adheres to and then is endocytosed by epithelial cells. Adherence is mediated in part by two different P. brasiliensis proteins with molecular masses of 30 and 43 kDa [75]. The endocytosis of this fungus requires intact epithelial cell microfilaments and microtubules, and triggers host cell apoptosis [74]. The identities of the P. brasiliensis adhesins and the host receptors to which they bind are currently unknown.
Summary
Most pathogenic fungi invade normally non-phagocytic host cells by inducing their own endocytosis. Although the invasion of these host cells is likely central to pathogenesis of disease, there are large gaps in our knowledge about whether invasion is induced by a membrane-ruffling or zipper mechanism. Furthermore, for those fungi that induce their own endocytosis by a zipper mechanism, there is a paucity of knowledge about the fungal surface proteins that induce invasion, the host cell receptor to which these endocytosing-inducing proteins bind, and the host cell signal transduction mechanisms that govern fungal invasion. However, the tools to efficiently fill these gaps in knowledge have already been developed within the last decade during the study of host cell invasion by viral, bacterial, and protozoal pathogens. Therefore it is highly likely that mechanisms of fungal invasion will be more clearly elucidated in the near future.
Acknowledgments
We thank the members of the Filler and Sheppard laboratories for stimulating and insightful discussions about this topic.
Abbreviations
- GXM
glucuronoxylomannan
- SAP
secreted aspartyl proteinase
- TNF-α
tumor necrosis factor α
Footnotes
Scott G. Filler is in the Division of Infectious Diseases at the Los Angeles Biomedical Research Institute at Harbor-UCLA Medical Center, Torrance, California, United States of America. Donald C. Sheppard is in the Department of Microbiology and Immunology, Faculty of Medicine, McGill University, Montreal, Quebec, Canada.
Competing interests. Scott G. Filler has equity in Novadigm Therapeutics, a company that is developing a vaccine against C. albicans.
Author contributions. SGF and DCS wrote the paper.
Funding. This work was supported in part by Public Health Service grants R01DE017088 and R01AI054928 from the National Institutes of Health. DCS is supported by a Clinician Scientist Award from the Canadian Institutes of Health Research, and a Career Award in the Biomedical Sciences from the Burroughs Wellcome Fund.
References
- Pizarro-Cerda J, Cossart P. Bacterial adhesion and entry into host cells. Cell. 2006;124:715–727. doi: 10.1016/j.cell.2006.02.012. [DOI] [PubMed] [Google Scholar]
- Montes LF, Wilborn WH. Ultrastructural features of host–parasite relationship in oral candidiasis. J Bacteriol. 1968;96:1349–1356. doi: 10.1128/jb.96.4.1349-1356.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawson RA, Rajasingham KC. Ultrastructural features of the invasive phase of Candida albicans. Br J Dermatol. 1972;87:435–443. doi: 10.1111/j.1365-2133.1972.tb01591.x. [DOI] [PubMed] [Google Scholar]
- Reichart PA, Philipsen HP, Schmidt-Westhausen A, Samaranayake LP. Pseudomembranous oral candidiasis in HIV infection: Ultrastructural findings. J Oral Pathol Med. 1995;24:276–281. doi: 10.1111/j.1600-0714.1995.tb01182.x. [DOI] [PubMed] [Google Scholar]
- Marrie TJ, Costerton JW. The ultrastructure of Candida albicans infections. Can J Microbiol. 1981;27:1156–1164. doi: 10.1139/m81-181. [DOI] [PubMed] [Google Scholar]
- Garcia-Tamayo J, Castillo G, Martinez AJ. Human genital candidiasis: Histochemistry, scanning and transmission electron microscopy. Acta Cytol. 1982;26:7–14. [PubMed] [Google Scholar]
- Scherwitz C. Ultrastructure of human cutaneous candidosis. J Invest Dermatol. 1982;78:200–205. doi: 10.1111/1523-1747.ep12506451. [DOI] [PubMed] [Google Scholar]
- Lo HJ, Kohler JR, DiDomenico B, Loebenberg D, Cacciapuoti A, et al. Nonfilamentous C. albicans mutants are avirulent. Cell. 1997;90:939–949. doi: 10.1016/s0092-8674(00)80358-x. [DOI] [PubMed] [Google Scholar]
- Saville SP, Lazzell AL, Monteagudo C, Lopez-Ribot JL. Engineered control of cell morphology in vivo reveals distinct roles for yeast and filamentous forms of Candida albicans during infection. Eukaryot Cell. 2003;2:1053–1060. doi: 10.1128/EC.2.5.1053-1060.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray TL, Payne CD. Scanning electron microscopy of epidermal adherence and cavitation in murine candidiasis: A role for Candida acid proteinase. Infect Immun. 1988;56:1942–1949. doi: 10.1128/iai.56.8.1942-1949.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stringaro A, Crateri P, Pellegrini G, Arancia G, Cassone A, et al. Ultrastructural localization of the secretory aspartyl proteinase in Candida albicans cell wall in vitro and in experimentally infected rat vagina. Mycopathologia. 1997;137:95–105. doi: 10.1023/a:1006897208863. [DOI] [PubMed] [Google Scholar]
- Schaller M, Korting HC, Schafer W, Bastert J, Chen W, et al. Secreted aspartic proteinase (Sap) activity contributes to tissue damage in a model of human oral candidosis. Mol Microbiol. 1999;34:169–180. doi: 10.1046/j.1365-2958.1999.01590.x. [DOI] [PubMed] [Google Scholar]
- Schaller M, Bein M, Korting HC, Baur S, Hamm G, et al. The secreted aspartyl proteinases Sap1 and Sap2 cause tissue damage in an in vitro model of vaginal candidiasis based on reconstituted human vaginal epithelium. Infect Immun. 2003;71:3227–3234. doi: 10.1128/IAI.71.6.3227-3234.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bernardis F, Arancia S, Morelli L, Hube B, Sanglard D, et al. Evidence that members of the secretory aspartyl proteinase gene family, in particular SAP2, are virulence factors for Candida vaginitis. J Infect Dis. 1999;179:201–208. doi: 10.1086/314546. [DOI] [PubMed] [Google Scholar]
- Andrian E, Grenier D, Rouabhia M. In vitro models of tissue penetration and destruction by Porphyromonas gingivalis. Infect Immun. 2004;72:4689–4698. doi: 10.1128/IAI.72.8.4689-4698.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai PJ, Kuo CF, Lin KY, Lin YS, Lei HY, et al. Effect of group A streptococcal cysteine protease on invasion of epithelial cells. Infect Immun. 1998;66:1460–1466. doi: 10.1128/iai.66.4.1460-1466.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park H, Myers CL, Sheppard DC, Phan QT, Sanchez AA, et al. Role of the fungal Ras-protein kinase A pathway in governing epithelial cell interactions during oropharyngeal candidiasis. Cell Microbiol. 2005;7:499–510. doi: 10.1111/j.1462-5822.2004.00476.x. [DOI] [PubMed] [Google Scholar]
- Drago L, Mombelli B, De Vecchi E, Bonaccorso C, Fassina MC, et al. Candida albicans cellular internalization: A new pathogenic factor? Int J Antimicrob Agents. 2000;16:545–547. doi: 10.1016/s0924-8579(00)00296-x. [DOI] [PubMed] [Google Scholar]
- Enache E, Eskandari T, Borja L, Wadsworth E, Hoxter B, et al. Candida albicans adherence to a human oesophageal cell line. Microbiology. 1996;142:2741–2746. doi: 10.1099/13500872-142-10-2741. [DOI] [PubMed] [Google Scholar]
- Chiang LY, Sheppard DC, Bruno VM, Mitchell AP, Edwards JE, Jr, et al. Candida albicans protein kinase CK2 governs virulence during oropharyngeal candidiasis. Cell Microbiol. 2006. E-pub 24 August 2006. [DOI] [PubMed]
- Martinez-Lopez R, Park H, Myers CL, Gil C, Filler SG. Candida albicans Ecm33p is important for normal cell wall architecture and interactions with host cells. Eukaryot Cell. 2006;5:140–147. doi: 10.1128/EC.5.1.140-147.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Groot PW, de Boer AD, Cunningham J, Dekker HL, de Jong L, et al. Proteomic analysis of Candida albicans cell walls reveals covalently bound carbohydrate-active enzymes and adhesins. Eukaryot Cell. 2004;3:955–965. doi: 10.1128/EC.3.4.955-965.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Lopez R, Monteoliva L, Diez-Orejas R, Nombela C, Gil C. The GPI-anchored protein CaEcm33p is required for cell wall integrity, morphogenesis and virulence in Candida albicans. Microbiology. 2004;150:3341–3354. doi: 10.1099/mic.0.27320-0. [DOI] [PubMed] [Google Scholar]
- Nadir E, Kaufshtein M. Images in clinical medicine. Candida albicans in a peripheral-blood smear. N Engl J Med. 2005;353:e9. doi: 10.1056/NEJMicm041054. [DOI] [PubMed] [Google Scholar]
- Klotz SA, Drutz DJ, Harrison JL, Huppert M. Adherence and penetration of vascular endothelium by Candida yeasts. Infect Immun. 1983;42:374–384. doi: 10.1128/iai.42.1.374-384.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotrosen D, Edwards JE, Jr, Gibson TR, Moore JC, Cohen AH, et al. Adherence of Candida to cultured vascular endothelial cells: Mechanisms of attachment and endothelial cell penetration. J Infect Dis. 1985;152:1264–1274. doi: 10.1093/infdis/152.6.1264. [DOI] [PubMed] [Google Scholar]
- Filler SG, Swerdloff JN, Hobbs C, Luckett PM. Penetration and damage of endothelial cells by Candida albicans. Infect Immun. 1995;63:976–983. doi: 10.1128/iai.63.3.976-983.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fratti RA, Ghannoum MA, Edwards JE, Jr, Filler SG. Gamma interferon protects endothelial cells from damage by Candida albicans by inhibiting endothelial cell phagocytosis. Infect Immun. 1996;64:4714–4718. doi: 10.1128/iai.64.11.4714-4718.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phan QT, Belanger PH, Filler SG. Role of hyphal formation in interactions of Candida albicans with endothelial cells. Infect Immun. 2000;68:3485–3490. doi: 10.1128/iai.68.6.3485-3490.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phan QT, Fratti RA, Prasadarao NV, Edwards JE, Jr, Filler SG. N-cadherin mediates endocytosis of Candida albicans by endothelial cells. J Biol Chem. 2005;280:10455–10461. doi: 10.1074/jbc.M412592200. [DOI] [PubMed] [Google Scholar]
- Belanger PH, Johnston D, Fratti RA, Zhang M, Filler SG. Endocytosis of Candida albicans by vascular endothelial cells is associated with tyrosine phosphorylation of specific host cell proteins. Cell Microbiol. 2002;4:805–812. doi: 10.1046/j.1462-5822.2002.00232.x. [DOI] [PubMed] [Google Scholar]
- Jong AY, Stins MF, Huang SH, Chen SH, Kim KS. Traversal of Candida albicans across human blood–brain barrier in vitro. Infect Immun. 2001;69:4536–4544. doi: 10.1128/IAI.69.7.4536-4544.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jong AY, Chen SH, Stins MF, Kim KS, Tuan TL, et al. Binding of Candida albicans enolase to plasmin(ogen) results in enhanced invasion of human brain microvascular endothelial cells. J Med Microbiol. 2003;52:615–622. doi: 10.1099/jmm.0.05060-0. [DOI] [PubMed] [Google Scholar]
- Lossinsky AS, Jong A, Fiala M, Mukhtar M, Buttle KF, et al. The histopathology of Candida albicans invasion in neonatal rat tissues and in the human blood–brain barrier in culture revealed by light, scanning, transmission and immunoelectron microscopy. Histol Histopathol. 2006;21:1029–1041. doi: 10.14670/HH-21.1029. [DOI] [PubMed] [Google Scholar]
- Sheppard DC, Yeaman MR, Welch WH, Phan QT, Fu Y, et al. Functional and structural diversity in the Als protein family of Candida albicans. J Biol Chem. 2004;279:30840–30849. doi: 10.1074/jbc.M401929200. [DOI] [PubMed] [Google Scholar]
- Mengaud J, Ohayon H, Gounon P, Mege RM, Cossart P. E-cadherin is the receptor for internalin, a surface protein required for entry of L. monocytogenes into epithelial cells. Cell. 1996;84:923–932. doi: 10.1016/s0092-8674(00)81070-3. [DOI] [PubMed] [Google Scholar]
- Merkel GJ, Cunningham RK. The interaction of Cryptococcus neoformans with primary rat lung cell cultures. J Med Vet Mycol. 1992;30:115–121. [PubMed] [Google Scholar]
- Barbosa FM, Fonseca FL, Holandino C, Alviano CS, Nimrichter L, et al. Glucuronoxylomannan-mediated interaction of Cryptococcus neoformans with human alveolar cells results in fungal internalization and host cell damage. Microbes Infect. 2006;8:493–502. doi: 10.1016/j.micinf.2005.07.027. [DOI] [PubMed] [Google Scholar]
- Merkel GJ, Scofield BA. The in vitro interaction of Cryptococcus neoformans with human lung epithelial cells. FEMS Immunol Med Microbiol. 1997;19:203–213. doi: 10.1111/j.1574-695X.1997.tb01089.x. [DOI] [PubMed] [Google Scholar]
- Chretien F, Lortholary O, Kansau I, Neuville S, Gray F, et al. Pathogenesis of cerebral Cryptococcus neoformans infection after fungemia. J Infect Dis. 2002;186:522–530. doi: 10.1086/341564. [DOI] [PubMed] [Google Scholar]
- Chang YC, Stins MF, McCaffery MJ, Miller GF, Pare DR, et al. Cryptococcal yeast cells invade the central nervous system via transcellular penetration of the blood–brain barrier. Infect Immun. 2004;72:4985–4995. doi: 10.1128/IAI.72.9.4985-4995.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen SH, Stins MF, Huang SH, Chen YH, Kwon-Chung KJ, et al. Cryptococcus neoformans induces alterations in the cytoskeleton of human brain microvascular endothelial cells. J Med Microbiol. 2003;52:961–970. doi: 10.1099/jmm.0.05230-0. [DOI] [PubMed] [Google Scholar]
- Chang YC, Jong A, Huang S, Zerfas P, Kwon-Chung KJ. CPS1, a homolog of the Streptococcus pneumoniae type 3 polysaccharide synthase gene, is important for the pathobiology of Cryptococcus neoformans. Infect Immun. 2006;74:3930–3938. doi: 10.1128/IAI.00089-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim AS, Filler SG, Alcouloumre MS, Kozel TR, Edwards JE, Jr, et al. Adherence to and damage of endothelial cells by Cryptococcus neoformans in vitro: Role of the capsule. Infect Immun. 1995;63:4368–4374. doi: 10.1128/iai.63.11.4368-4374.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasadarao NV, Srivastava PK, Rudrabhatla RS, Kim KS, Huang SH, et al. Cloning and expression of the Escherichia coli K1 outer membrane protein A receptor, a gp96 homologue. Infect Immun. 2003;71:1680–1688. doi: 10.1128/IAI.71.4.1680-1688.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coenjaerts FE, Hoepelman AI, Scharringa J, Aarts M, Ellerbroek PM, et al. The Skn7 response regulator of Cryptococcus neoformans is involved in oxidative stress signalling and augments intracellular survival in endothelium. FEMS Yeast Res. 2006;6:652–661. doi: 10.1111/j.1567-1364.2006.00065.x. [DOI] [PubMed] [Google Scholar]
- Marr KA, Carter RA, Crippa F, Wald A, Corey L. Epidemiology and outcome of mould infections in hematopoietic stem cell transplant recipients. Clin Infect Dis. 2002;34:909–917. doi: 10.1086/339202. [DOI] [PubMed] [Google Scholar]
- DeHart DJ, Agwu DE, Julian NC, Washburn RG. Binding and germination of Aspergillus fumigatus conidia on cultured A549 pneumocytes. J Infect Dis. 1997;175:146–150. doi: 10.1093/infdis/175.1.146. [DOI] [PubMed] [Google Scholar]
- Paris S, Boisvieux-Ulrich E, Crestani B, Houcine O, Taramelli D, et al. Internalization of Aspergillus fumigatus conidia by epithelial and endothelial cells. Infect Immun. 1997;65:1510–1514. doi: 10.1128/iai.65.4.1510-1514.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Liu R, Noordhoek JA, Kauffman HF. Interaction of airway epithelial cells (A549) with spores and mycelium of Aspergillus fumigatus. J Infect. 2005;51:375–382. doi: 10.1016/j.jinf.2004.12.012. [DOI] [PubMed] [Google Scholar]
- Wasylnka JA, Moore MM. Aspergillus fumigatus conidia survive and germinate in acidic organelles of A549 epithelial cells. J Cell Sci. 2003;116:1579–1587. doi: 10.1242/jcs.00329. [DOI] [PubMed] [Google Scholar]
- Berkova N, Lair-Fulleringer S, Femenia F, Huet D, Wagner MC, et al. Aspergillus fumigatus conidia inhibit tumour necrosis factor- or staurosporine-induced apoptosis in epithelial cells. Int Immunol. 2006;18:139–150. doi: 10.1093/intimm/dxh356. [DOI] [PubMed] [Google Scholar]
- Fraser RS. Pulmonary aspergillosis: Pathologic and pathogenetic features. Pathol Annu. 1993;28(Part 1):231–277. [PubMed] [Google Scholar]
- Shaukat A, Bakri F, Young P, Hahn T, Ball D, et al. Invasive filamentous fungal infections in allogeneic hematopoietic stem cell transplant recipients after recovery from neutropenia: Clinical, radiologic, and pathologic characteristics. Mycopathologia. 2005;159:181–188. doi: 10.1007/s11046-004-5495-0. [DOI] [PubMed] [Google Scholar]
- van Buul-Wortelboer MF, Brinkman HJ, Reinders JH, van Aken WG, van Mourik JA. Polar secretion of von Willebrand factor by endothelial cells. Biochim Biophys Acta. 1989;1011:129–133. doi: 10.1016/0167-4889(89)90199-7. [DOI] [PubMed] [Google Scholar]
- Mark KS, Miller DW. Increased permeability of primary cultured brain microvessel endothelial cell monolayers following TNF-alpha exposure. Life Sci. 1999;64:1941–1953. doi: 10.1016/s0024-3205(99)00139-3. [DOI] [PubMed] [Google Scholar]
- Lopes-Bezerra LM, Filler SG. Interactions of Aspergillus fumigatus with endothelial cells: Internalization, injury, and stimulation of tissue factor activity. Blood. 2004;103:2143–2149. doi: 10.1182/blood-2003-06-2186. [DOI] [PubMed] [Google Scholar]
- Wasylnka JA, Moore MM. Uptake of Aspergillus fumigatus conidia by phagocytic and nonphagocytic cells in vitro: Quantitation using strains expressing green fluorescent protein. Infect Immun. 2002;70:3156–3163. doi: 10.1128/IAI.70.6.3156-3163.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown J. Zygomycosis: An emerging fungal infection. Am J Health Syst Pharm. 2005;62:2593–2596. doi: 10.2146/ajhp050188. [DOI] [PubMed] [Google Scholar]
- Frater JL, Hall GS, Procop GW. Histologic features of zygomycosis: Emphasis on perineural invasion and fungal morphology. Arch Pathol Lab Med. 2001;125:375–378. doi: 10.5858/2001-125-0375-HFOZ. [DOI] [PubMed] [Google Scholar]
- Ibrahim AS, Spellberg B, Avanessian V, Fu Y, Edwards JE., Jr Rhizopus oryzae adheres to, is phagocytosed by, and damages endothelial cells in vitro. Infect Immun. 2005;73:778–783. doi: 10.1128/IAI.73.2.778-783.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stampfuss JJ, Censarek P, Fischer JW, Schror K, Weber AA. Rapid release of active tissue factor from human arterial smooth muscle cells under flow conditions. Arterioscler Thromb Vasc Biol. 2006;26:e34–37. doi: 10.1161/01.ATV.0000216407.89528.b0. [DOI] [PubMed] [Google Scholar]
- da Rosa AC, Scroferneker ML, Vettorato R, Gervini RL, Vettorato G, et al. Epidemiology of sporotrichosis: A study of 304 cases in Brazil. J Am Acad Dermatol. 2005;52:451–459. doi: 10.1016/j.jaad.2004.11.046. [DOI] [PubMed] [Google Scholar]
- Davis DA, Bruno V, Loza L, Filler SG, Mitchell AP. C. albicans Mds3p, a conserved regulator of pH responses and virulence identified through insertional mutagenesis. Genetics. 2002;162:1573–1581. doi: 10.1093/genetics/162.4.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figueiredo CC, De Lima OC, De Carvalho L, Lopes-Bezerra LM, Morandi V. The in vitro interaction of Sporothrix schenckii with human endothelial cells is modulated by cytokines and involves endothelial surface molecules. Microb Pathog. 2004;36:177–188. doi: 10.1016/j.micpath.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Cundell DR, Gerard NP, Gerard C, Idanpaan-Heikkila I, Tuomanen EI. Streptococcus pneumoniae anchor to activated human cells by the receptor for platelet-activating factor. Nature. 1995;377:435–438. doi: 10.1038/377435a0. [DOI] [PubMed] [Google Scholar]
- Woods JP, Heinecke EL, Luecke JW, Maldonado E, Ng JZ, et al. Pathogenesis of Histoplasma capsulatum. Semin Respir Infect. 2001;16:91–101. doi: 10.1053/srin.2001.24239. [DOI] [PubMed] [Google Scholar]
- Porta A, Maresca B. Host response and Histoplasma capsulatum/macrophage molecular interactions. Med Mycol. 2000;38:399–406. doi: 10.1080/mmy.38.6.399.406. [DOI] [PubMed] [Google Scholar]
- Eissenberg LG, West JL, Woods JP, Goldman WE. Infection of P388D1 macrophages and respiratory epithelial cells by Histoplasma capsulatum: Selection of avirulent variants and their potential role in persistent histoplasmosis. Infect Immun. 1991;59:1639–1646. doi: 10.1128/iai.59.5.1639-1646.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eissenberg LG, Moser SA, Goldman WE. Alterations to the cell wall of Histoplasma capsulatum yeasts during infection of macrophages or epithelial cells. J Infect Dis. 1997;175:1538–1544. doi: 10.1086/516496. [DOI] [PubMed] [Google Scholar]
- Borges-Walmsley MI, Chen D, Shu X, Walmsley AR. The pathobiology of Paracoccidioides brasiliensis. Trends Microbiol. 2002;10:80–87. doi: 10.1016/s0966-842x(01)02292-2. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Lenzi HL, Motta EM, Caputo L, Sahaza JH, et al. Expression of adhesion molecules in lungs of mice infected with Paracoccidioides brasiliensis conidia. Microbes Infect. 2005;7:666–673. doi: 10.1016/j.micinf.2005.01.004. [DOI] [PubMed] [Google Scholar]
- Hanna SA, Monteiro da Silva JL, Giannini MJ. Adherence and intracellular parasitism of Paracoccidioides brasiliensis in Vero cells. Microbes Infect. 2000;2:877–884. doi: 10.1016/s1286-4579(00)00390-7. [DOI] [PubMed] [Google Scholar]
- Mendes-Giannini MJ, Hanna SA, da Silva JL, Andreotti PF, Vincenzi LR, et al. Invasion of epithelial mammalian cells by Paracoccidioides brasiliensis leads to cytoskeletal rearrangement and apoptosis of the host cell. Microbes Infect. 2004;6:882–891. doi: 10.1016/j.micinf.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Andreotti PF, Monteiro da Silva JL, Bailao AM, Soares CM, Benard G, et al. Isolation and partial characterization of a 30 kDa adhesin from Paracoccidioides brasiliensis. Microbes Infect. 2005;7:875–881. doi: 10.1016/j.micinf.2005.02.005. [DOI] [PubMed] [Google Scholar]