Abstract
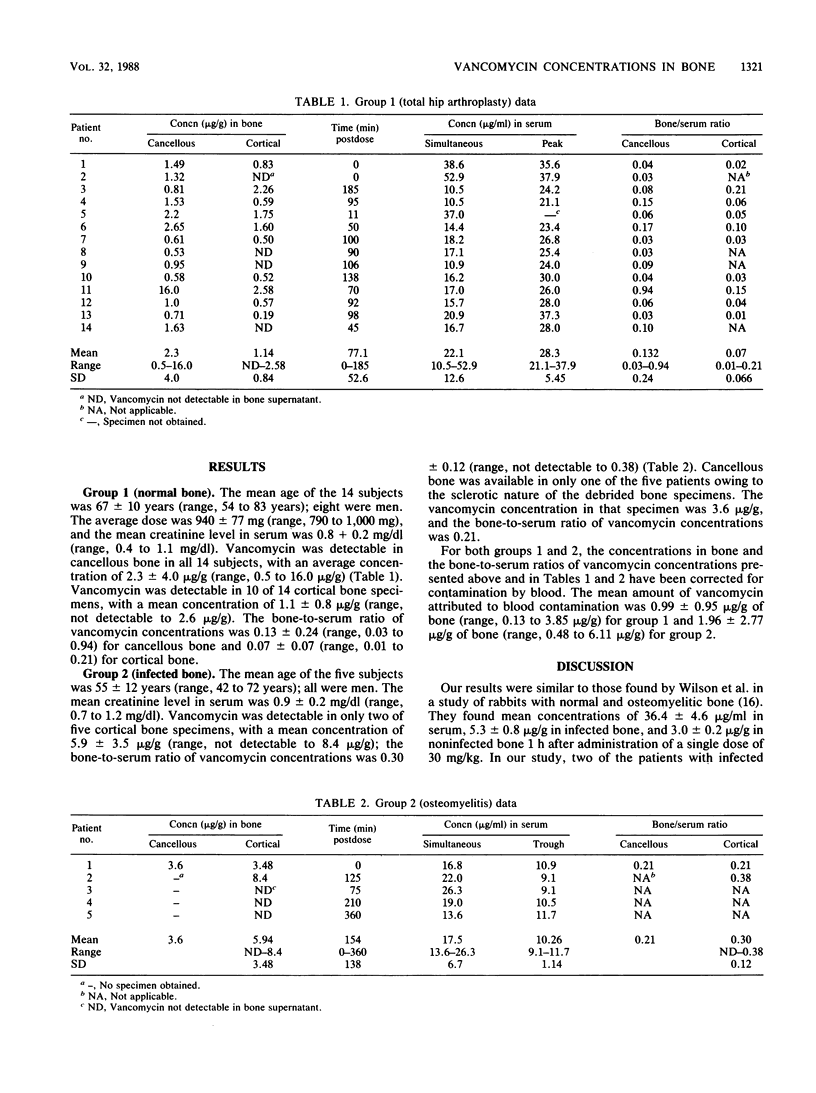
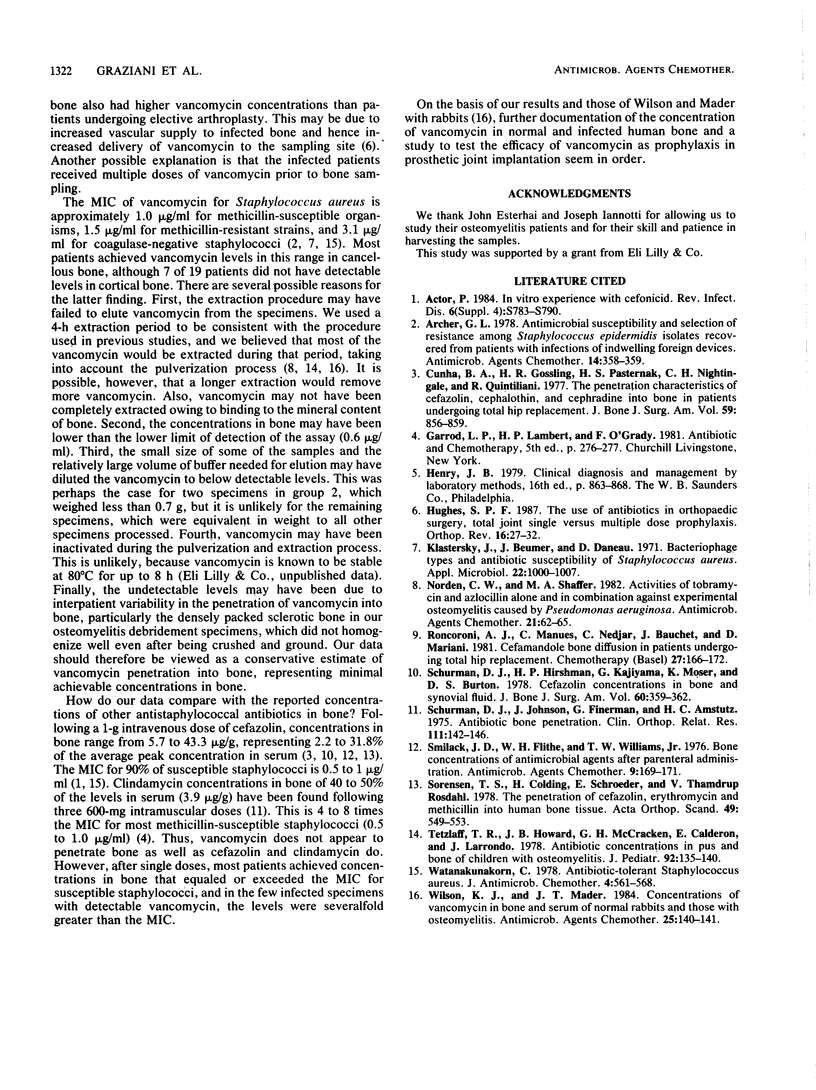
Concentrations of vancomycin in bones of 14 patients undergoing total hip arthroplasty (group 1) and 5 patients with osteomyelitis (group 2) were studied. Group 1 received vancomycin, 15 mg/kg intravenously, 1 h prior to anesthesia. Group 2 received doses adjusted to achieve peak levels in serum of 20 to 30 micrograms/ml and trough levels of less than 12 micrograms/ml; bone specimens were collected during surgical debridement. The specimens were pulverized and eluted into phosphate buffer, and the supernatants were analyzed for vancomycin content by fluorescence polarization immunoassay. In group 1, vancomycin was detectable in all cancellous specimens with a mean concentration of 2.3 +/- 4.0 micrograms/g (range, 0.5 to 16 micrograms/g); 10 of 14 cortical specimens had detectable vancomycin; the mean cortical concentration was 1.1 +/- 0.8 micrograms/g (range, not detectable to 2.6 micrograms/g). In group 2, vancomycin was detectable in only two of five cortical bone specimens (mean concentration, 5.9 +/- 3.5 micrograms/g). Cancellous bone was obtained in one patient; the vancomycin concentration was 3.6 micrograms/g. In most patients the vancomycin levels in bones were higher than the MIC for susceptible staphylococci following single prophylactic doses. In the few infected patients studied, penetration was variable and deserves further study.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Actor P. In vitro experience with cefonicid. Rev Infect Dis. 1984 Nov-Dec;6 (Suppl 4):S783–S790. doi: 10.1093/clinids/6.supplement_4.s783. [DOI] [PubMed] [Google Scholar]
- Archer G. L. Antimicrobial susceptibility and selection of resistance among Staphylococcus epidermidis isolates recovered from patients with infections of indwelling foreign devices. Antimicrob Agents Chemother. 1978 Sep;14(3):353–359. doi: 10.1128/aac.14.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bargar W. L. A conversation with William L. Bargar, MD. Custom cementless total hip replacement. Orthop Rev. 1987 Jan;16(1):27–37. [PubMed] [Google Scholar]
- Cunha B. A., Gossling H. R., Pasternak H. S., Nightingale C. H., Quintiliani R. The penetration characteristics of cefazolin, cephalothin, and cephradine into bone in patients undergoing total hip replacement. J Bone Joint Surg Am. 1977 Oct;59(7):856–859. [PubMed] [Google Scholar]
- Klastersky J., Beumer J., Daneau D. Bacteriophage types and antibiotic susceptibility of Staphylococcus aureus. Appl Microbiol. 1971 Dec;22(6):1000–1007. doi: 10.1128/am.22.6.1000-1007.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norden C. W., Shaffer M. A. Activities of tobramycin and azlocillin alone and in combination against experimental osteomyelitis caused by Pseudomonas aeruginosa. Antimicrob Agents Chemother. 1982 Jan;21(1):62–65. doi: 10.1128/aac.21.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roncoroni A. J., Manuel C., Nedjar C., Bauchet J., Mariani D. Cefamandole bone diffusion in patients undergoing total hip replacement. Chemotherapy. 1981;27(3):166–172. doi: 10.1159/000237973. [DOI] [PubMed] [Google Scholar]
- Schurman D. J., Hirshman H. P., Kajiyama G., Moser K., Burton D. S. Cefazolin concentrations in bone and synovial fluid. J Bone Joint Surg Am. 1978 Apr;60(3):359–362. [PubMed] [Google Scholar]
- Schurman D. J., Johnson B. L., Jr, Finerman G., Amstutz H. C. Antibiotic bone penetration. Concentrations of methicillin and clindamycin phosphate in human bone taken during total hip replacement. Clin Orthop Relat Res. 1975 Sep;(111):142–146. [PubMed] [Google Scholar]
- Smilack J. D., Flittie W. H., Williams T. W., Jr Bone concentrations of antimicrobial agents after parenteral administration. Antimicrob Agents Chemother. 1976 Jan;9(1):169–171. doi: 10.1128/aac.9.1.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen T. S., Colding H., Schroeder E., Rosdahl V. T. The penetration of cefazolin, erythromycin and methicillin into human bone tissue. Acta Orthop Scand. 1978 Dec;49(6):549–553. doi: 10.3109/17453677808993236. [DOI] [PubMed] [Google Scholar]
- Tetzlaff T. R., Howard J. B., McCraken G. H., Calderon E., Larrondo J. Antibiotic concentrations in pus and bone of children with osteomyelitis. J Pediatr. 1978 Jan;92(1):135–140. doi: 10.1016/s0022-3476(78)80095-x. [DOI] [PubMed] [Google Scholar]
- Watanakunakorn C. Antibiotic-tolerant Staphylococcus aureus. J Antimicrob Chemother. 1978 Nov;4(6):561–568. doi: 10.1093/jac/4.6.561. [DOI] [PubMed] [Google Scholar]
- Wilson K. J., Mader J. T. Concentrations of vancomycin in bone and serum of normal rabbits and those with osteomyelitis. Antimicrob Agents Chemother. 1984 Jan;25(1):140–141. doi: 10.1128/aac.25.1.140. [DOI] [PMC free article] [PubMed] [Google Scholar]


