Abstract
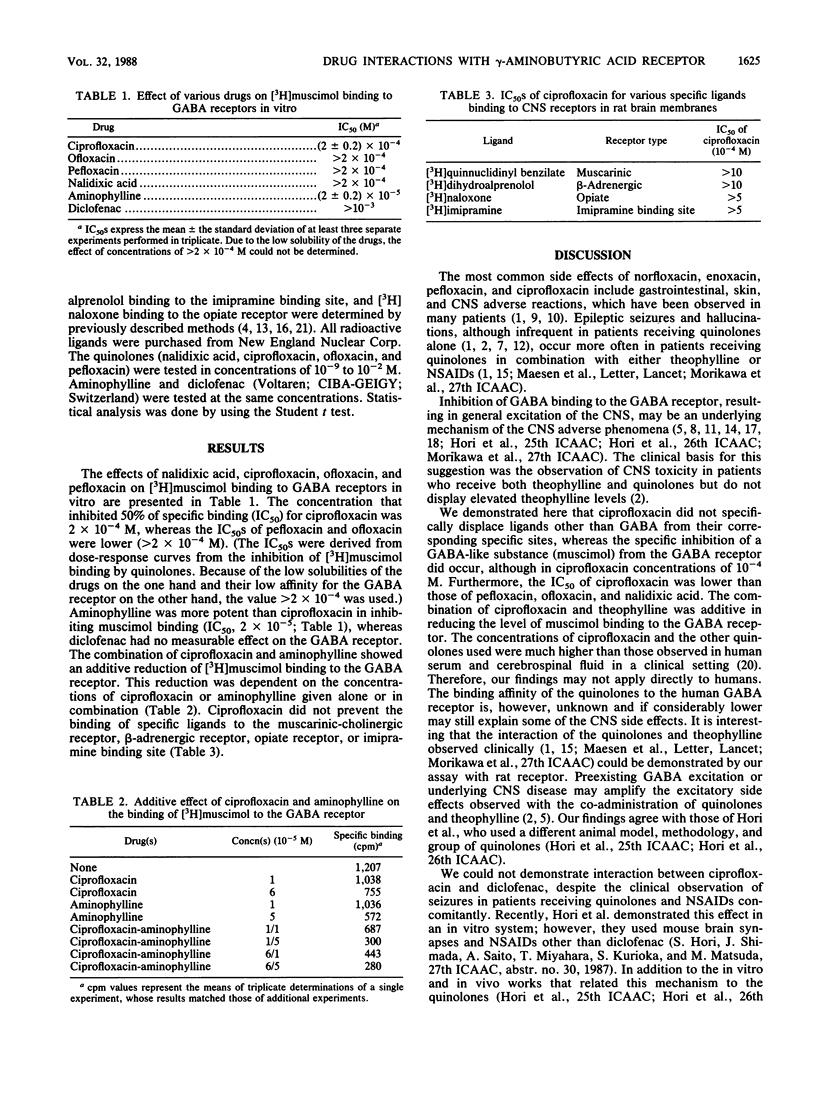
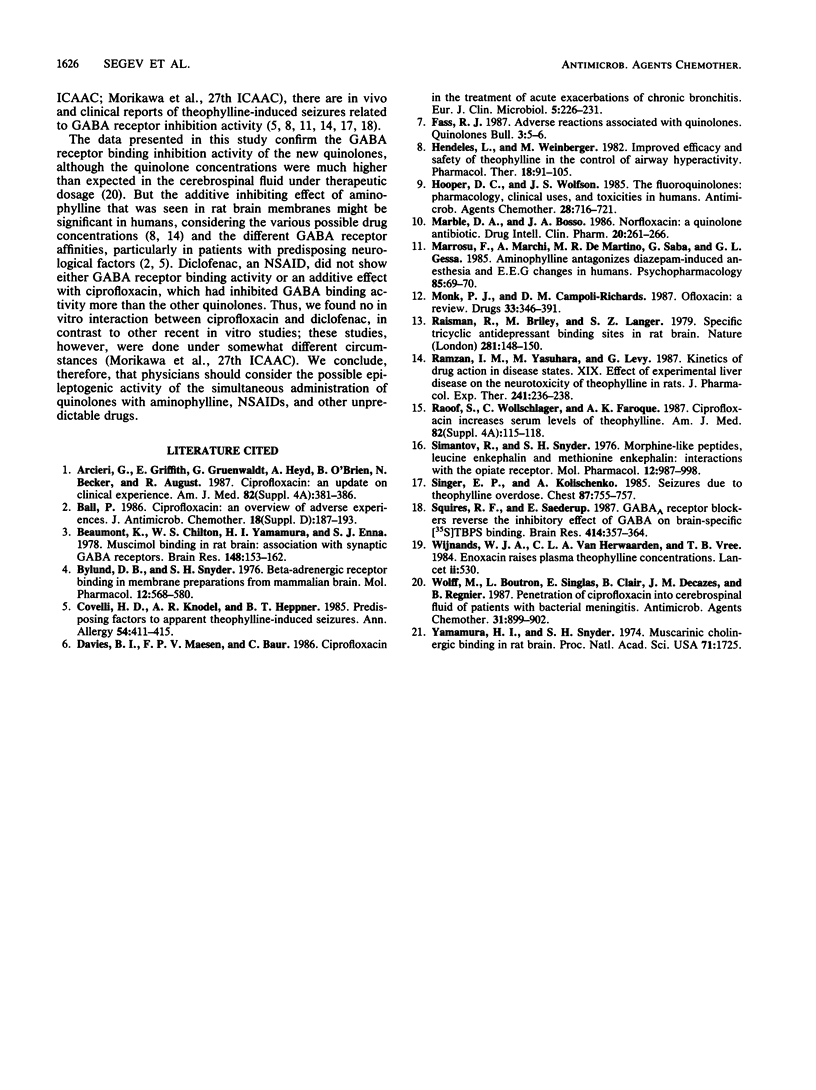
Epileptic seizures and hallucinations, which are rare in patients receiving quinolones, have been observed more frequently in patients receiving both quinolones and either theophylline or nonsteroidal anti-inflammatory drugs. Inhibition of gamma-aminobutyric acid (GABA) binding to the GABA receptor, resulting in general excitation of the central nervous system, may be the underlying mechanism of these adverse phenomena. We demonstrate here that ciprofloxacin displaced a GABA-like substance (muscimol) from the GABA receptor when administered in concentrations of greater than 10(-4) M. These concentrations were lower than those needed by pefloxacin, ofloxacin, and nalidixic acid to reach a concentration that inhibits 50% of binding. The combination of ciprofloxacin and theophylline was additive in reducing the level of muscimol binding to the GABA receptor, whereas a diclofenac-ciprofloxacin combination had no effect. The concentrations of both ciprofloxacin and the other quinolones used were much higher than those observed in human serum and cerebrospinal fluid in a clinical setting; however, different human GABA receptor affinities, preexisting GABA excitation, or underlying central nervous system disease may amplify the excitatory side effects observed by the co-administration of quinolones and theophylline. Attention should be paid to the possible epileptogenic activity of the simultaneous administration of quinolones with aminophylline, nonsteroidal anti-inflammatory drugs, or other unpredictable drugs.
Full text
PDF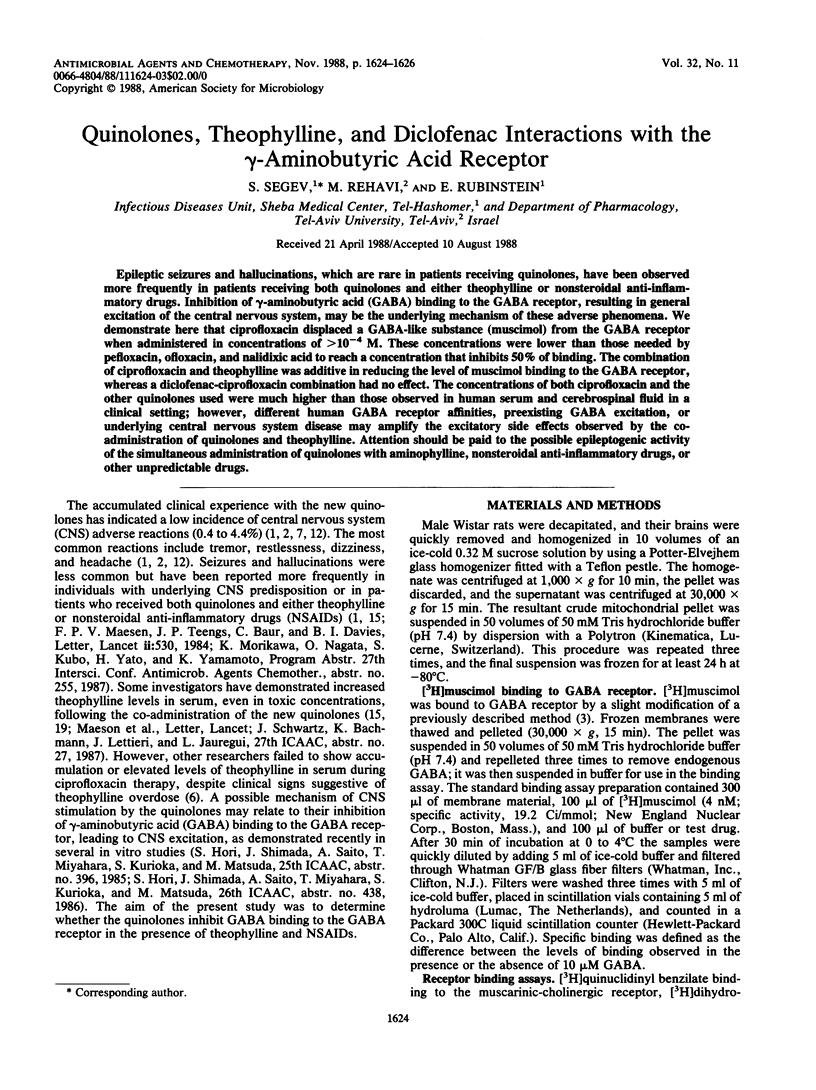
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arcieri G., Griffith E., Gruenwaldt G., Heyd A., O'Brien B., Becker N., August R. Ciprofloxacin: an update on clinical experience. Am J Med. 1987 Apr 27;82(4A):381–386. [PubMed] [Google Scholar]
- Ball P. Ciprofloxacin: an overview of adverse experiences. J Antimicrob Chemother. 1986 Nov;18 (Suppl 500):187–193. doi: 10.1093/jac/18.sd.187. [DOI] [PubMed] [Google Scholar]
- Beaumont K., Chilton W. S., Yamamura H. I., Enna S. J. Muscimol binding in rat brain: association with synaptic GABA receptors. Brain Res. 1978 Jun 9;148(1):153–162. doi: 10.1016/0006-8993(78)90385-2. [DOI] [PubMed] [Google Scholar]
- Bylund D. B., Snyder S. H. Beta adrenergic receptor binding in membrane preparations from mammalian brain. Mol Pharmacol. 1976 Jul;12(4):568–580. [PubMed] [Google Scholar]
- Covelli H. D., Knodel A. R., Heppner B. T. Predisposing factors to apparent theophylline-induced seizures. Ann Allergy. 1985 May;54(5):411–415. [PubMed] [Google Scholar]
- Davies B. I., Maesen F. P., Baur C. Ciprofloxacin in the treatment of acute exacerbations of chronic bronchitis. Eur J Clin Microbiol. 1986 Apr;5(2):226–231. doi: 10.1007/BF02013995. [DOI] [PubMed] [Google Scholar]
- Hendeles L., Weinberger M. Improved efficacy and safety of theophylline in the control of airways hyperreactivity. Pharmacol Ther. 1982;18(1):91–105. doi: 10.1016/0163-7258(82)90027-4. [DOI] [PubMed] [Google Scholar]
- Hooper D. C., Wolfson J. S. The fluoroquinolones: pharmacology, clinical uses, and toxicities in humans. Antimicrob Agents Chemother. 1985 Nov;28(5):716–721. doi: 10.1128/aac.28.5.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marble D. A., Bosso J. A. Norfloxacin: a quinoline antibiotic. Drug Intell Clin Pharm. 1986 Apr;20(4):261–266. doi: 10.1177/106002808602000402. [DOI] [PubMed] [Google Scholar]
- Marrosu F., Marchi A., De Martino M. R., Saba G., Gessa G. L. Aminophylline antagonizes diazepam-induced anesthesia and EEG changes in humans. Psychopharmacology (Berl) 1985;85(1):69–70. doi: 10.1007/BF00427325. [DOI] [PubMed] [Google Scholar]
- Monk J. P., Campoli-Richards D. M. Ofloxacin. A review of its antibacterial activity, pharmacokinetic properties and therapeutic use. Drugs. 1987 Apr;33(4):346–391. doi: 10.2165/00003495-198733040-00003. [DOI] [PubMed] [Google Scholar]
- Raisman R., Briley M., Langer S. Z. Specific tricyclic antidepressant binding sites in rat brain. Nature. 1979 Sep 13;281(5727):148–150. doi: 10.1038/281148a0. [DOI] [PubMed] [Google Scholar]
- Ramzan I. M., Yasuhara M., Levy G. Kinetics of drug action in disease states. XIX. Effect of experimental liver disease on the neurotoxicity of theophylline in rats. J Pharmacol Exp Ther. 1987 Apr;241(1):236–238. [PubMed] [Google Scholar]
- Raoof S., Wollschlager C., Khan F. A. Ciprofloxacin increases serum levels of theophylline. Am J Med. 1987 Apr 27;82(4A):115–118. [PubMed] [Google Scholar]
- Simantov R., Snyder S. H. Morphine-like peptides, leucine enkephalin and methionine enkephalin: interactions with the opiate receptor. Mol Pharmacol. 1976 Nov;12(6):987–998. [PubMed] [Google Scholar]
- Singer E. P., Kolischenko A. Seizures due to theophylline overdose. Chest. 1985 Jun;87(6):755–757. doi: 10.1378/chest.87.6.755. [DOI] [PubMed] [Google Scholar]
- Squires R. F., Saederup E. GABAA receptor blockers reverse the inhibitory effect of GABA on brain-specific [35S]TBPS binding. Brain Res. 1987 Jun 30;414(2):357–364. doi: 10.1016/0006-8993(87)90017-5. [DOI] [PubMed] [Google Scholar]
- Wolff M., Boutron L., Singlas E., Clair B., Decazes J. M., Regnier B. Penetration of ciprofloxacin into cerebrospinal fluid of patients with bacterial meningitis. Antimicrob Agents Chemother. 1987 Jun;31(6):899–902. doi: 10.1128/aac.31.6.899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamura H. I., Snyder S. H. Muscarinic cholinergic binding in rat brain. Proc Natl Acad Sci U S A. 1974 May;71(5):1725–1729. doi: 10.1073/pnas.71.5.1725. [DOI] [PMC free article] [PubMed] [Google Scholar]



